Abstract
Objective
The authors evaluate the clinical and radiographic outcome of the management of acute thoracolumbar burst fractures by anterolateral or posterior approach.
Methods
Thirty four (34) consecutive patients with a single-level traumatic unstable burst fracture at the thoracolumbar junction were surgically treated between Jan. 2004 and Dec. 2006. Twenty one patients were operated on by anterolateral approach, strut graft and fixation with a Kaneda plate. Thirteen patients were treated with posterior approach and transpedicular screw fixation. Clinical and radiographic evaluation was performed on all 34 patients before and after surgery.
Results
There were 34 thoracolumbar burst fractures in 27 male and 7 female patients. Fifty-nine percent (20 of 34) of patients presented with a neurologic deficit. The mean follow-up duration was 18.5 months (range 7-44 months). Preoperative canal encroachment in the anterolateral and posterior groups measured 49.3±7.6%, 27.3±9% respectively (p=0.001). Preoperative angular deformity in the anterolateral and posterior groups measured 19.4±8.4° and 12.9±4.5° respectively. At discharge, angular deformity had been corrected to 10.5±7.3° and 7.6±4.9° in both groups, respectively. Preoperative Frankel grade grade in the anterolateral and posterior groups was 3.9±1.2, 3.9±1.5 respectively (p=0.9). Postoperatively, it had been improved to 4.4±1.1, 4.2±1.4 in both groups, respectively.
Unstable thoracolumbar burst fractures may be treated with anterior, posterior or circumferential fusion. The anterolateral retroperitoneal flank approach for the thoracolumbar spinal trauma is one of the excellent choices. It allows the surgeon to perform corpectomy and fusion, reconstructing the anterior and middle columns and fusion of only 2 levels.7,13,14) It provides more visibility of many forms of surgical pathology and easier procedure to achieve acceptable reduction and fixation than the other fixation procedures in thoracolumbar injuries. This led some surgeons to advocate anterolateral approaches.11,18) But anterolateral retroperitoneal flank approach is not familiar with neurosurgeon and it is more stressful to patients. The development of posterior pedicle screw instrumentation allowed more rigid fixation.5,19)
Using posterior fixation, canal encroachment is improved indirectly by ligamentotaxis. Alternatively, a transpedicular or costotransversectomy decompression technique can be used.27) Canal decompression is limited, though, and often incomplete. Regardless of approach, surgical goal of fixation is to minimize spinal instability and recover the neurological deficit.
This study compares the preoperative factors and clinical outcome of anterolateral or posterior approach for treatment of lumbar burst fractures. Postoperative radiographic outcomes for 34 patients treated with anterolateral or posteroior approach of segmental fixation were retrospectively reviewed to evaluate the safety/feasibility of fracture reduction and maintenance of correction after operation.
A total of 34 consecutive adult patients with unstable thoracolumbar burst fractures treated with anterolateral or posterior approach. The mean follow-up was 18.5 months (range, 7-44 months) and the surgery was performed between January 2004 and December 2007 in a single institution. There were 27 males, and 7 females. The causes of injuries were fall down in 20 of patients, motor-vehicle accidents in 8 and other accident in 6. For the instrumentation, the patients were divided into two groups: anterolateral approach group of 21 patients for Kaneda plate system (DePuy spine, Raynham, MA)(M : F=15 : 6) and posterior approach group of 13 patients for transpedicular screw fixation (M : F=12 : 1). The selection of approach was decided by neurological status, percentage of vertebral height loss and canal encroachment.
In anterolateral approach group, the surgical indications are vertebral height loss over 40%, canal encroachment over 50% with neurological deficits. In posterior approach group, indications are vertebral height loss over 30%, below 50%, canal encroachment over 30%, below 50% and/or neurological deficit.
Patients underwent a single-stage anterolateral approach (thoracoabdominal, or retroperitoneal) with single-level corpectomy decompression and reduction.
We made a standard skin incision over the 11th rib and resected the 11th rib from the from the angle of the rib to the junction of rib and costal cartilage, leaving the rib bed intact.
Complete discectomy at the level caudad and cephalad to the fracture was performed. A large ronguer is used to remove the anterior cancellous portion of the vertebral body.
After corpectomy, we inserted the titanium-mesh cage packed with corpected vertebral body and rib. Instrumentation was performed with Kaneda device (Depuy Acromed®). Bicortical fixation was performed in all constructs, which were appropriately compressed to improve load sharing. Postoperatively, all patients were managed in a total-contact thoracolumbar sacral orthosis for 3 months.
Thirteen Patients were surgically treated with posterior segmental fixation and posterolateral fusion using iliac crest bone graft. We performed pedicle screws fixation at 2 level above and 1 level below the fracture site. Decompression was achieved through a transpedicular approach in 1 patient. Other patients did not performed decompression (laminectomy, transpedicular and transfacet approach). For fusion, bone harvested from the decompression site or iliac crest autograft augmented.
Clinical outcomes were measured before surgery and at the final follow-up in out patient department using the Frankel motor score system (Table 1).9) For ease of statistical analysis, the Frankel grade was converted into a numerical score in which A is equal to 1 (complete motor and sensory paralysis below the lesion), B is 2 (complete motor paralysis but some residual sensory perception), C is 3 (residual motor function but not of practical usefulness to the patient), D is 4 (useful but subnormal motor function below the lesion), and E is 5 (normal motor and sensory function). Results are expressed as the means±the standard deviations.
Regardless of which approach was used, the goal of surgery was to decompress the canal, correct the kyphosis, and stabilize the spine. After surgery, Patients were mobilized gradually while wearing lumbar orthoses. Braces were generally worn for 3 months postoperatively. All the patients had preoperative plain radiographs, CT scans and MRI scan. The patients underwent postoperative radiograph before discharge. They were followed up 1, 3, 6 months postoperatively and then annually. In addition to radiographic analysis, postoperative follow-up evaluation included review of medical records and postoperative visit in out patient department. The radiographs were obtained standing lateral views and were analyzed with particular attention paid to the sagittal Cobb's angles at the operation segments (Figure 1).
Data were analyzed using analysis of variance, the Wilcoxon test, and the Fisher exact test.
Significance was accepted at a probability value of less than or equal to 0.05.
Of 34 patients who had undergone fusion surgery, 27 were male and 7 were female.
The mean patient age at the time of surgery was 45.5 years (range, 19-79 years). The mean follow-up period was 18.5 months (range, 7-44 months). Twenty one patients underwent the anterolateral retroperitoneal flank approach, 13 patients underwent a posterior approach. Patient demographics is summarized in Table 2.
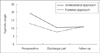
Preoperative and postoperative neurological status, represented by Frankel scores, is summarized in Table 3. The mean preoperative Frankel scores in the anterolateral and posterior groups were 3.9±1.2 and 3.9±1.5, respectively (p=0.672). There was a trend for improvement in each treatment group, with the mean Frankel scores improving to 4.4±1.1 and 4.2±1.4 in the anterolateral and posterior groups, respectively (Figure 2). The improvement of the Frankel scores, however, was significant in each group-anterolateral (p=0.012) and posterior (p=0.014).
The mean postraumatic loss of anterior vertebral body height in the anterolateral and posterior groups were 50.1±7.5% and 32±5.1%, respectively (p=0.001). Preoperative CT scanning demonstrated that the canal encroachment at the fracture site averaged 49±7.6% in the anterolateral group and 27.3±9% in the posterior group (p=0.001).
Preoperative angular deformity in the anterolateral and posterior groups measured 19.4±8.4° and 12.9±4.5°, respectively. There is significant difference between two groups (p=0.001).
Whereas postoperatively angular deformity had been corrected to 10.5±7.3 and 7.6±4.9° in the anterolateral (p=0.001) and posterior groups (p=0.001), respectively. At the last follow-up examination, angular deformity had progressed to 12.8±6.4° in the anterolateral group (p=0.078) and to 10.8±4.8° in the posterior group (p=0.003) (Table 4). Compared with the extent of angulation on admission, it had decreased by 6.6° in the anterolateral group and had decreased by 2.4° in the posterior group. The last follow up changes in angulation were significant in both groups-anterolateral (p=0.001) and posterior (p=0.003) (Figure 3).
There was no progression of initial neurologic deficit in any of the 34 patients.
There were no complications such as intraoperative vascular injuries, neural structure injury and hardware failure. In anterolateral approach group, three patients required chest tube after surgery due to open the pleura cavity during the operation. Two patients who underwent anterolateral approaches developed low thoracic dermatomal pain from intercostal neuralgia that was improved with pain medication (Gabapentine). One patient in anterolateral approach group suffered from operation site infection. It was successfully treated with antibiotics. Residual back pain was more common in posterior group.
Almost two thirds of all traumatic TL spine injuries occur at the TL junction, most frequently at L1, followed by T12.16) About half of all TL junction lesions are characterized by a burst of the vertebral body. Due to the anterior column destruction, traumatic TL junction burst fractures typically show a marked initial regional kyphosis of 10-32°on supine lateral radiographs.2,6,21,22) From an anatomical standpoint, the ideal treatment of unstable TL junction fractures should consist of complete kyphosis correction and optimal spinal canal decompression in case of a neurological deficit. The treatment of TL junction burst fractures remains very controversial for a number of reasons. In a comparison between anterolateral and posterior decompression, the anterolateral approach allows direct decompression of ventral osseous and offering superior canal clearance as compared with posterior approach (ligamentotaxis, posterolateral decompression techniques).8,15,25) Bradford and McBride3) reported improved better neurological outcome in the anterolateral approach group as compared with the posterior management of thoracolumbar fractures, and this correlated with significantly less residual canal stenosis.3,12) Additionally, anterolateral thoracolumbar treatment of unstable injuries allows short-segment constructs to be used, saving motion segments.11,25)
In posterior approach, Bradford and McMarkel and Graziano17) reported that posterior decompression and fusion led to excellent correction of spinal deformity, improvement in neurological function, and high fusion rates. Despite improved results, the constructs still require fixation two levels above and below the injury. Attempts to shorten the constructs have resulted in higher failure rates. Short-segment posterior constructs have been associated with reportedly high failure rates, ranging from 10% to 50%.1,23)
Analysis of our clinical outcome demonstrates that neurological improvement was documented in our patients regardless of which approach was used. Radiological results in our study show that angulation decreased only 2.4° between admission and discharge, and it progressed to 10.8±4.8° at the final follow-up examination in the posterior group. In the anterolateral group, however, angulation was corrected by 6.6° between admission and discharge, and the correction persisted at 12.8±6.4° at follow up. At the follow-up evaluation, the correction well maintained after discharge and there is no significant difference in anterolateral group (p=0.078). It means that kyphotic angulation is well corrected regardless of approach, but angular deformity is more successfully maintained after surgery when the anterolateral approach is used.
Currently, guidelines based on randomized trials for the treatment of thoracolumbar burst fractures are unavailable.16) Verlaan et al.26) conducted a literature review of 132 papers, involving 5,748 patients with thoracic and lumbar fractures treated with posterior, anterolateral or combined approaches. They concluded that evidence-based guidelines for the treatment of these fractures were absent and suggested that, for a better comparison of surgical techniques, randomized controlled trials were necessary. We agree with their conclusions, but we need to consider several parameters before we chose the selection of treatment options.
This selection should be based on clinical and radiological finding such as deformity angulation, residual canal diameter and vertebral body height including neurological deficit.13,23) In case of the anterior column alone is affected by loss of height but not canal compromise, surgery is generally not needed.10) For patients have no neurological deficits with burst fractures, angular deformity is less than 30° (it means vertebral body is sufficiently preserved to provide some load sharing) and canal encroachment is less than 40%, posterior approach is sufficient.4,20,24) When significant fragmentation of the vertebral body exists, patients have neurological deficit (either complete or incomplete) and there is poor apposition of the fragments and loss in height, anterior grafts and instrumentation are necessary.23)
There is a primary limitation of this study. The limitation would be potential differences of surgical indication in both patients group. We acknowledge this but our study is not a simple comparison of clinical and radiological outcome in both different approach groups. Analysis of our results, there is no difference of clinical outcome in both groups. Radiological results in our study show that kyphotic angulation is well corrected regardless of approach but angular deformity is more successfully maintained in the anterolateral approach. But final follow up, there is no significant difference of kyphotic angle in both groups. It means that if we choose the proper patients and select the treatment based on clinical and radiological finding, clinical and radiological outcomes will be satisfied.
Advantage of anterolateral approach is fewer spinal segments are immobilized and complete and reliable decompression of the spinal canal. Whereas posterior approach is less invasive and led to excellent correction of spinal deformity. Rigid guidelines for the selection of anterior or posterior approaches are lacking. Evaluation of the authors' results and those of others shows that that angular deformity is successfully corrected regardless of approach and anterior strut is more successfully maintained when using the anterior approach. Before we chose the selection of treatment options, several parameters need to be considered. This selection should be based on clinical and radiological finding including neurological deficit, deformity angulation, residual canal diameter and vertebral body height.
Figures and Tables
 | FIGURE 1The kyphotic angulation. Plain lateral radiograph showing loss in vertebral body (VB) height and kyphotic angulation. It shows change of sagittal Cobb's angle with Kaneda device fixation and posterior screw fusion between preoperative (A), (C) and last follow up (B), (D). |
 | FIGURE 2Bar graph showing preoperative, discharge and follow-up Frankel scores. At follow up, improvement in Frankel scores is noted irrespective of the approach (p=0.672). The difference in Frankel scores between the two groups is not significant on admission, discharge or at follow up; however, the improvement in the Frankel score was significant within each group-anterolateral (white bar) (p=0.012) and posterior (black bar) (p=0.014). |
 | FIGURE 3Line graph showing deformity angles at admission, discharge, and latest follow up in the anterolateral (solid line) and posterior (dot line) instrumentation groups. |
TABLE 1
Standard neurological classification of spinal cord injury according to the Frankel motor score system

References
1. Alanay A, Acaroglu E, Yazici M, Oznur A, Surat A. Short-segment pedicle instrumentation of thoracolumbar burst fractures: does transpedicular intracorporeal grafting prevent early failure? Spine (Phila Pa 1976). 2001; 26:213–217.
2. Alanay A, Yazici M, Acaroglu E, Turhan E, Cila A, Surat A. Course of nonsurgical management of burst fractures with intact posterior ligamentous complex: an MRI study. Spine (Phila Pa 1976). 2004; 29:2425–2431.

3. Bradford DS, McBride GG. Surgical management of thoracolumbar spine fractures with incomplete neurologic deficits. Clin Orthop Relat Res. 1987; 218:201–216.

4. Cantor JB, Lebwohl NH, Garvey T, Eismont FJ. Nonoperative management of stable thoracolumbar burst fractures with early ambulation and bracing. Spine (Phila Pa 1976). 1993; 18:971–976.

5. Carl AL, Tromanhauser SG, Roger DJ. Pedicle screw instrumentation for thoracolumbar burst fractures and fracture-dislocations. Spine (Phila Pa 1976). 1992; 17:S317–S324.

6. Carl AL, Tranmer BI, Sachs BL. Anterolateral dynamized instrumentation and fusion for unstable thoracolumbar and lumbar burst fractures. Spine (Phila Pa 1976). 1997; 22:686–690.

7. Dick JC, Brodke DS, Zdeblick TA, Bartel BD, Kunz DN, Rapoff AJ. Anterior instrumentation of the thoracolumbar spine. A biomechanical comparison. Spine (Phila Pa 1976). 1997; 22:744–750.
8. Dunn HK. Anterior stabilization of thoracolumbar injuries. Clin Orthop Relat Res. 1984; 189:116–124.

9. Frankel HL, Hancock DO, Hyslop G, Melzack J, Michaelis LS, Ungar GH, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia. 1969; 7:179–192.
10. Gertzbein SD. Spine update. Classification of thoracic and lumbar fractures. Spine (Phila Pa 1976). 1994; 19:626–628.
11. Ghanayem AJ, Zdeblick TA. Anterior instrumentation in the management of thoracolumbar burst fractures. Clin Orthop Relat Res. 1997; (355):89–100.

12. Hitchon PW, Goel VK, Rogge T, Grosland NM, Torner J. Biomechanical studies on two anterior thoracolumbar implants in cadaveric spines. Spine (Phila Pa 1976). 1999; 24:213–218.

13. Hitchon PW, Torner JC, Haddad SF, Follett KA. Management options in thoracolumbar burst fractures. Surg Neurol. 1998; 49:619–626. discussion 626-627.

14. Kaneda K, Taneichi H, Abumi K, Hashimoto T, Satoh S, Fujiya M. Anterior decompression and stabilization with the Kaneda device for thoracolumbar burst fractures associated with neurological deficits. J Bone Joint Surg Am. 1997; 79:69–83.
15. Kostuik JP. Anterior fixation for fractures of the thoracic and lumbar spine with or without neurologic involvement. Clin Orthop Relat Res. 1984; (189):103–115.

16. Magerl F, Aebi M, Gertzbein S, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994; 3:184–201.

17. Markel DC, Graziano GP. A comparison study of treatment of thoracolumbar fractures using the ACE Posterior Segmental Fixator and Cotrel-Dubousset instrumentation. Orthopedics. 1995; 18:679–686.

18. McDonough PW, Davis R, Tribus C, Zdeblick TA. The management of acute thoracolumbar burst fractures with anterior corpectomy and Z-plate fixation. Spine (Phila Pa 1976). 2004; 29:1901–1908. discussion 1909.

19. McNamara MJ, Stephens GC, Spengler DM. Transpedicular short-segment fusions for treatment of lumbar burst fractures. J Spinal Disord. 1992; 5:183–187.

20. Mumford J, Weinstein JN, Spratt KF, Goel VK. Thoracolumbar burst fractures. The clinical efficacy and outcome of nonoperative management. Spine (Phila Pa 1976). 1993; 18:955–970.
21. Narotam PK, Pauley SM, McGinn GJ. Titanium mesh cages for cervical spine stabilization after corpectomy: a clinical and radiological study. J Neurosurg. 2003; 99:2 Suppl. 172–180.

22. Okuyama K, Abe E, Chiba M, Ishikawa N, Sato K. Outcome of anterior decompression and stabilization for thoracolumbar unstable burst fractures in the absence of neurologic deficits. Spine (Phila Pa 1976). 1996; 21:620–625.

23. Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures: a consecutive 41/2-year series. Spine (Phila Pa 1976). 2000; 25:1157–1170.
24. Rechtine GR 2nd, Cahill D, Chrin AM. Treatment of thoracolumbar trauma: comparison of complications of operative versus nonoperative treatment. J Spinal Disord. 1999; 12:406–409.
25. Shono Y, McAfee PC, Cunningham BW. Experimental study of thoracolumbar burst fractures. A radiographic and biomechanical analysis of anterior and posterior instrumentation systems. Spine (Phila Pa 1976). 1994; 19:1711–1722.
26. Verlaan JJ, Diekerhof CH, Buskens E, van der Tweel I, Verbout AJ, Dhert WJ, et al. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine (Phila Pa 1976). 2004; 29:803–814.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download