Abstract
Background and Objectives
Anaplastic thyroid carcinoma (ATC) is commonly related with concurrent differentiated thyroid carcinoma (DTC). We aimed to examine the clinicopathologic characteristics, prognosis and gene expression of DTC with anaplastic foci.
Materials and Methods
Eighteen patients with DTC with anaplastic foci were enrolled in this study. To compare the clinicopathologic characteristics and prognosis of anaplastic foci subjects with conventional ATC or DTC, we additionally included 12 ATC and 1030 DTC patients who diagnosed during same period. Immunohistochemistry was performed to check the gene expression in anaplastic foci and DTC component.
Results
In anaplastic foci group, tumor size was larger (2.5±1.3 vs. 1.2±0.9 cm, p=0.001), distant metastasis was more frequent (11.1 vs. 0%, p=0.000) and 1-year survival rate was low (88.9 vs. 100%, p=0.000) than DTC group. In contrast, compared with ATC group, anaplastic foci group showed younger age at diagnosis (50±16 vs. 63±18 years, p=0.039), smaller tumor size (2.5±1.3 vs. 3.8±1.4 cm, p=0.027), less distant metastasis (11.1 vs. 41.7%, p=0.084) and longer 1-year survival rate (88.9 vs. 25.0%, p=0.001). Expression of p53 protein was observed in 100% of anaplastic foci, ATC and 12.5% of papillary thyroid carcinoma component.
Anaplastic thyroid carcinoma (ATC) is rare and accounts for only 2% of thyroid cancer.1) However ATC is the most aggressive form of thyroid cancer, so overall median survival is limited to months. Despite this poor prognosis, some patients with ATC survived relatively longer periods after diagnosis of ATC. In previous studies, long-term survival is possible when patient is younger age and tumor has smaller size, localizes in thyroid parenchyma and can be completely resected by surgery.234)
Currently, it is generally accepted that ATC does not arise de novo but rather transforms or evolves from differentiated thyroid carcinoma (DTC).56) ATC is commonly related with previous or concurrent thyroid disorders, including DTC.78) This pathological association of ATC with DTC has led to the emergence of the concept of anaplastic transformation which means an intratumoral evolution or progression from DTC to ATC.9)
According to the Surveillance, Epidemiology and End Results (SEER) Program of National Cancer Institute, incidence of ATC has decreased by 22% during 1973-2003.10) In contrast, recent study reported that ATC with coexistent DTC was significantly increased from 1995 to 2010.11) These results suggested that the incidence of ATC was decreased by early elimination of anaplastic transformation. In addition, the prognosis of DTC including small foci of anaplastic transformation was better than expected than ATC.11) However, due to scarcity, there are still not many reports of DTC with small foci of ATC.
The aim of the present study is to examine the clinicopathologic characteristics, prognosis and gene expression of DTC with small foci of anaplastic transformation.
Medical records of patients diagnosed with thyroid cancer at Seoul National University Hospital from January 2003 to July 2009 were retrospectively reviewed in February 2010. Among them, eighteen patients underwent total thyroidectomy for preoperative diagnosis of DTC and small foci of anaplastic transformation change in their surgical specimen were discovered incidentally. Foci of anaplastic transformation were defined when areas of anaplastic change didn't exceed 10% of total surface of DTC. Pathology of DTC with foci of anaplastic transformation was reexamined by one pathologist (K.C.J). In all 18 patients, DTC components were diagnosed with papillary thyroid carcinoma (PTC).
To compare the clinicopathologic characteristics and prognosis of DTC accompanied by foci of anaplastic transformation with conventional ATC or DTC, we additionally included 12 ATC and 1030 DTC (all PTCs) patients who diagnosed at Seoul National University Hospital during same period (from January 2003 to July 2009). Patients with PTC accompanied by foci of anaplastic transformation was named anaplastic foci group. This study's protocol and survey were approved by the Seoul National University Hospital Institutional Review Board.
Among 12 ATC patients, 3 patients did not get thyroidectomy and paraffin blocks of other 3 patients who had thyroidectomy were not available for immunohistochemistry (IHC), we evaluated IHC for the rest 6 ATC patients. Sixteen of the 18 cases of anaplastic foci group had available tissue for IHC evaluation. Specimens were fixed in 10% buffered formalin, embedded in paraffin wax, and stained Hematoxylin and Eosin (H&E) for histologic examination. Among 18 PTC with anaplastic transformation patients, 11 Paraffin blocks which included both PTC and anaplastic foci components were available for immunohistochemistry staining.
Four micron-thick sections were deparaffinized, rehydrated in graded alcohols, and processed using DAKO envision detection kit (DakoCytomation, Carpinteria, CA, USA). Briefly, antigen retrieval was performed in a microwave oven for 15 min in 10 mM citrate buffer pH 6.0. Endogenous peroxidase activity was blocked with a 3% H2O2-methanol solution, and the slides were incubated in 10% normal goat serum for 30 min to prevent non-specific staining. They were then incubated for 1 hour at room temperature with an appropriately diluted primary antibody. The following monoclonal antibodies were used: p53 (clone DO-7, DaKoCytomation; dilution 1:1000), E-cadherin (clone 36B5, Novocastra laboratories Ltd, Newcastle, UK; dilution 1:100), Thyroglobulin (clone DAK-Tg6, DaKoCytomation; dilution 1:15000), Bcl-2 (clone 124, DaKoCytomation, Carpinteria, CA, USA; dilution 1:200), Cyclin D1 (clone DCS-6, NeoMarker, Fremont, CA, USA; dilution 1:50). Thereafter, the sections were incubated with DAKO Envision/HRP for 30 min. Diaminobenzidine was used as a chromogen, and the sections were counterstained with Mayer's hematoxylin. As a negative control, non-immune serum was substituted for the primary antibody.
Nuclear staining for p53, cyclin D1 was interpreted positive, if more than 50% of cancer cell showed strong nuclear reactivity. Cytoplasmic Bcl-2 and thyroglobulin and membranous E-cadherin were scored positive when they showed strong staining. Weak or negative staining was interpreted negative. IHC results were scored by one pathologist (K.C.J) who were blinded to all patients' clinical data.
All continuous variables were expressed as means±SD. Statistical analysis was performed by a Pearson's chi-square test, Student's t-test or Mann-Whitney U test. The cumulative survival rate of patients was analyzed from the date of diagnosis of thyroid cancer to the date of death or last follow up day using the Kaplan-Meier method and log-rank test. A p<0.05 was considered significant. These analyses were performed using SPSS for Windows (SPSS 16.0, Chicago, IL, USA).
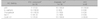
Firstly, we compared anaplastic foci group with DTC group. In anaplastic foci group, tumor size was larger (2.5±1.3 vs. 1.2±0.9 cm, p=0.001), distant metastasis was more frequent (11.1 vs. 0%, p=0.000) and 1-year survival rate was low (88.9 vs. 100%, p= 0.000). In contrast, compared with ATC group, anaplastic foci group showed younger age at diagnosis (50±16 vs. 63±18 years, p=0.039), smaller tumor size (2.5±1.3 vs. 3.8±1.4 cm, p=0.027), less distant metastasis (11.1 vs. 41.7%, p=0.084) and longer 1-year survival rate (88.9 vs. 25.0%, p=0.001) (Table 1).
The cumulative survival curves of three patient groups (DTC, anaplastic foci and ATC) are shown in Fig. 1. Anaplastic foci group survived significantly longer than ATC group and showed shorter cumulative survival rate than DTC group (log rank test p=0.000).
To compare the gene expression of anaplastic foci and PTC, we performed immunohistochemistry staining both anaplastic foci and PTC components. We also stained ATC for comparison of gene expression. In immunohistochemistry staining, expression of p53 protein was observed in 100% of anaplastic foci, ATC and 12.5% of PTC component. Expression of E-cadherin, thyroglobulin and Bcl-2 was decreased in anaplastic foci and ATC (Table 2).
Among 18 anaplastic foci patients, 2 patients were died due to brain metastasis (Table 3, Pt No 15, 18). One patient was diagnosed as brain metastasis after thyroid surgery and the other patient detected brain metastasis after radiation therapy (RT). Other 16 patients were still alive until now, and median follow up period was 115 months (range, 73 to 180 months). After surgery, 12 patients were received postoperative RT (2 Gy per fraction, once a day; total dose 58-66 Gy) and 4 patients were treated with two or three times radioactive iodine (RAI) therapy (Table 3).
Age at diagnosis is younger (47±14 vs. 75±4 years, p=0.013), total tumor size was smaller (2.2±1.2 vs. 4.3±1.1 cm, p=0.052) in survivor group than death group. Other pathological characteristics, such as extrathyroidal invasion, multiplicity and lymph node metastasis were not different between survivor and death group (data not shown).
In this study, we examined clinicopathologic characteristics and prognosis of DTC with small (less than 10% of total surface) anaplastic foci group compared with DTC and ATC group. In cumulative survival, anaplastic foci group showed shorter survival rate than DTC group but longer survival rate than ATC group. In addition, anaplastic foci group was mild and had better prognosis than ATC group, although it was more aggressive and showed poor prognosis than DTC group. Anaplastic foci group was younger and smaller than ATC, while older and larger than DTC group. In IHC results, anaplastic foci showed increased expression of p53 and decreased expression of E-cadherin, thyroglobulin and Bcl-2, which was consistent with results of previous study about molecular markers altered during transformation of differentiated into ATC.9) All these results support that DTC with anaplastic foci was intermediate state from DTC to ATC.
While it is possible that ATC may arise de novo, it has been generally accepted that ATC can develop from pre-existing DTC.5612) Several evidences support the fact that ATC derives from DTC. One is that ATC concurrent with DTC was found about 50% (23-71%) in several cohort studies about ATC patients.57813) In a study analyzing entire tumor sections, every ATC contained components of papillary or follicular carcinoma or both.14) Second evidence is that BRAF mutation was found in ATC with PTC component. In pooled data using 29 studies, overall prevalence of BRAF mutation of 44% in PTC and 24% in ATC and 0% in medullary and follicular thyroid cancer.15) BRAF was mutated in 78% of ATCs with papillary thyroid cancer background.16) In addition, BRAF mutations were identified in the papillary component and poorly differentiated or anaplastic carcinoma area arising from PTC at the same time.17) However, we could not examine BRAF mutation in anaplastic foci in this study, because the foci of anaplastic tumor were so small, we could not get enough DNA sample from foci of anaplastic tumor.
ATC is nearly always fatal, however sometimes ATC showed long term survival when anaplastic transformation is focal, encapsulated, or tumors can be entirely resected.21819) In this study, most of anaplastic foci group showed long term survival and 66.7% (12/18) patients were younger than 60 years old. Considering the peak incidence of ATC is six to seventh decade of life, most of our patients were detected very early. Only two patients (No 15, 18, Table 3) died due to brain metastasis and they were over 70 years old. Therefore, old age might be considered as a poor prognostic factor and if anaplastic foci were found in elderly, it will be necessary to check whether anaplastic thyroid cancer is metastatic.
Because the strategy to treat DTC with anaplastic foci patients was not established so far, we performed RT for 12 patients and RAI therapy for 4 patients after total thyroidectomy. All four patients in RAI group were survived more than 2 years and still alive until now. The sodium iodine symporter (NIS) mediated iodine uptake to thyroid allows diagnostic thyroid scintigraphy as well as effective therapeutic application of radioiodine in thyroid cancer. Because the expression of NIS is decreased in ATC, ATC does not accumulate I-131 and therefore is refractory to RAI therapy.2021) However, if the patients had thyroid cancer which contained only small component of intrathyroidal ATC and was completely resected, RAI therapy may be considered for ablation of PTC.22) In previous study, both RAI and RT were effective for the improvement of survival of DTC with anaplastic foci and showed no significant difference.23) Therefore, more research is needed to find out which treatment is more appropriate for DTC with anaplastic foci.
In conclusion, DTC with anaplastic foci has a worse prognosis than DTC, but have a better prognosis than ATC. Our results support that DTC with anaplastic foci was intermediate state from DTC to ATC.
Figures and Tables
 | Fig. 1The survival curve of those patients with anaplastic thyroid carcinoma (solid line), papillary thyroid carcinoma with anaplastic foci (dashed line) and papillary thyroid carcinoma (dotted line). p-value 0.000 by log rank test. |
Table 1
Comparison of clinicopathologic characteristics between differentiated thyroid carcinoma (DTC) with anaplastic foci and anaplastic thyroid carcinoma (ATC)

Acknowledgments
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea, funded by the Ministry of Science, ICT & Future Planning (NRF-2016R1A2B 4012417).
References
2. Haigh PI, Ituarte PH, Wu HS, Treseler PA, Posner MD, Quivey JM, et al. Completely resected anaplastic thyroid carcinoma combined with adjuvant chemotherapy and irradiation is associated with prolonged survival. Cancer. 2001; 91(12):2335–2342.

3. Kim TY, Kim KW, Jung TS, Kim JM, Kim SW, Chung KW, et al. Prognostic factors for Korean patients with anaplastic thyroid carcinoma. Head Neck. 2007; 29(8):765–772.

4. Sugitani I, Miyauchi A, Sugino K, Okamoto T, Yoshida A, Suzuki S. Prognostic factors and treatment outcomes for anaplastic thyroid carcinoma: ATC Research Consortium of Japan cohort study of 677 patients. World J Surg. 2012; 36(6):1247–1254.

5. Spires JR, Schwartz MR, Miller RH. Anaplastic thyroid carcinoma. Association with differentiated thyroid cancer. Arch Otolaryngol Head Neck Surg. 1988; 114(1):40–44.

6. Hunt JL, Tometsko M, LiVolsi VA, Swalsky P, Finkelstein SD, Barnes EL. Molecular evidence of anaplastic transformation in coexisting well-differentiated and anaplastic carcinomas of the thyroid. Am J Surg Pathol. 2003; 27(12):1559–1564.

7. Tan RK, Finley RK 3rd, Driscoll D, Bakamjian V, Hicks WL Jr, Shedd DP. Anaplastic carcinoma of the thyroid: a 24-year experience. Head Neck. 1995; 17(1):41–47. discussion 47-8.

8. McIver B, Hay ID, Giuffrida DF, Dvorak CE, Grant CS, Thompson GB, et al. Anaplastic thyroid carcinoma: a 50-year experience at a single institution. Surgery. 2001; 130(6):1028–1034.

9. Wiseman SM, Griffith OL, Deen S, Rajput A, Masoudi H, Gilks B, et al. Identification of molecular markers altered during transformation of differentiated into anaplastic thyroid carcinoma. Arch Surg. 2007; 142(8):717–727. discussion 727-9.

10. Albores-Saavedra J, Henson DE, Glazer E, Schwartz AM. Changing patterns in the incidence and survival of thyroid cancer with follicular phenotype--papillary, follicular, and anaplastic: a morphological and epidemiological study. Endocr Pathol. 2007; 18(1):1–7.

11. Han JM, Bae Kim W, Kim TY, Ryu JS, Gong G, Hong SJ, et al. Time trend in tumour size and characteristics of anaplastic thyroid carcinoma. Clin Endocrinol (Oxf). 2012; 77(3):459–464.

12. Wiseman SM, Loree TR, Hicks WL Jr, Rigual NR, Winston JS, Tan D, et al. Anaplastic thyroid cancer evolved from papillary carcinoma: demonstration of anaplastic transformation by means of the inter-simple sequence repeat polymerase chain reaction. Arch Otolaryngol Head Neck Surg. 2003; 129(1):96–100.

13. Sugitani I, Kasai N, Fujimoto Y, Yanagisawa A. Prognostic factors and therapeutic strategy for anaplastic carcinoma of the thyroid. World J Surg. 2001; 25(5):617–622.

14. Ibanez ML, Russell WO, Albores-Saavedra J, Lampertico P, White EC, Clark RL. Thyroid carcinoma--biologic behavior and mortality. Postmortem findings in 42 cases, including 27 in which the disease was fatal. Cancer. 1966; 19(8):1039–1052.

16. Quiros RM, Ding HG, Gattuso P, Prinz RA, Xu X. Evidence that one subset of anaplastic thyroid carcinomas are derived from papillary carcinomas due to BRAF and p53 mutations. Cancer. 2005; 103(11):2261–2268.

17. Nikiforova MN, Kimura ET, Gandhi M, Biddinger PW, Knauf JA, Basolo F, et al. BRAF mutations in thyroid tumors are restricted to papillary carcinomas and anaplastic or poorly differentiated carcinomas arising from papillary carcinomas. J Clin Endocrinol Metab. 2003; 88(11):5399–5404.

18. Nilsson O, Lindeberg J, Zedenius J, Ekman E, Tennvall J, Blomgren H, et al. Anaplastic giant cell carcinoma of the thyroid gland: treatment and survival over a 25-year period. World J Surg. 1998; 22(7):725–730.

19. Sugino K, Ito K, Mimura T, Nagahama M, Fukunari N, Kubo A, et al. The important role of operations in the management of anaplastic thyroid carcinoma. Surgery. 2002; 131(3):245–248.

20. Neff RL, Farrar WB, Kloos RT, Burman KD. Anaplastic thyroid cancer. Endocrinol Metab Clin North Am. 2008; 37(2):525–538, xi.

21. O'Neill JP, Power D, Condron C, Bouchier-Hayes D, Walsh M. Anaplastic thyroid cancer, tumorigenesis and therapy. Ir J Med Sci. 2010; 179(1):9–15.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download