Abstract
Background and Objectives
Blood neutrophil-to-lymphocyte ratio (NLR) has been reported to have poor prognostic impact in variable malignancies. However, studies evaluating the clinical significance of blood NLR in patient with papillary thyroid carcinoma (PTC) has been relatively rare, and the outcomes were inconsistent. In this study, we sought to analyze the clinical value of NLR in patients with PTC who had cervical lymph node metastasis.
Materials and Methods
Retrospective chart review was conducted with 174 patients with confirmed neck metastasis of PTC after initial thyroidectomy. Blood NLR was estimated by dividing the absolute number of blood neutrophil with that of lymphocyte. Statistical analysis was conducted to evaluate correlation between NLR and clinicopathologic factors, patterns of metastatic lymph nodes, and recurrence.
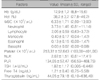
Figures and Tables
References
1. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; 26(1):1–133.

2. Mazzaferri EL, Kloos RT. Clinical review 128: Current approaches to primary therapy for papillary and follicular thyroid cancer. J Clin Endocrinol Metab. 2001; 86(4):1447–1463.

3. Ito Y, Miyauchi A. Prognostic factors and therapeutic strategies for differentiated carcinomas of the thyroid. Endocr J. 2009; 56(2):177–192.

4. Moo TA, McGill J, Allendorf J, Lee J, Fahey T 3rd, Zarnegar R. Impact of prophylactic central neck lymph node dissection on early recurrence in papillary thyroid carcinoma. World J Surg. 2010; 34(6):1187–1191.

5. Randolph GW, Duh QY, Heller KS, LiVolsi VA, Mandel SJ, Steward DL, et al. The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid. 2012; 22(11):1144–1152.

6. Lee HS, Park C, Kim SW, Noh WJ, Lim SJ, Chun BK, et al. Pathologic features of metastatic lymph nodes identified from prophylactic central neck dissection in patients with papillary thyroid carcinoma. Eur Arch Otorhinolaryngol. 2016; 273(10):3277–3285.

7. Lee HS, Park C, Kim SW, Park T, Chun BK, Hong JC, et al. Correlation of minimal extrathyroidal extension with pathologic features of lymph node metastasis in patients with papillary thyroid carcinoma. J Surg Oncol. 2015; 112(6):592–596.

8. Melo M, Gaspar da, Batista R, Vinagre J, Martins MJ, Costa G, et al. TERT, BRAF, and NRAS in primary thyroid cancer and metastatic disease. J Clin Endocrinol Metab. 2017; 102(6):1898–1907.

9. Yin Y, Wang J, Wang X, Gu L, Pei H, Kuai S, et al. Prognostic value of the neutrophil to lymphocyte ratio in lung cancer: a meta-analysis. Clinics (Sao Paulo). 2015; 70(7):524–530.

10. Wei B, Yao M, Xing C, Wang W, Yao J, Hong Y, et al. The neutrophil lymphocyte ratio is associated with breast cancer prognosis: an updated systematic review and meta-analysis. Onco Targets Ther. 2016; 9:5567–5575.

11. Gu X, Gao X, Li X, Qi X, Ma M, Qin S, et al. Prognostic significance of neutrophil-to-lymphocyte ratio in prostate cancer: evidence from 16,266 patients. Sci Rep. 2016; 6:22089.

12. Yang JJ, Hu ZG, Shi WX, Deng T, He SQ, Yuan SG. Prognostic significance of neutrophil to lymphocyte ratio in pancreatic cancer: a meta-analysis. World J Gastroenterol. 2015; 21(9):2807–2815.

13. Li MX, Liu XM, Zhang XF, Zhang JF, Wang WL, Zhu Y, et al. Prognostic role of neutrophil-to-lymphocyte ratio in colorectal cancer: a systematic review and meta-analysis. Int J Cancer. 2014; 134(10):2403–2413.

14. Liu JF, Ba L, Lv H, Lv D, Du JT, Jing XM, et al. Association between neutrophil-to-lymphocyte ratio and differentiated thyroid cancer: a meta-analysis. Sci Rep. 2016; 6:38551.

15. Kim SM, Kim EH, Kim BH, Kim JH, Park SB, Nam YJ, et al. Association of the preoperative neutrophil-to-ymphocyte count ratio and platelet-to-lymphocyte count ratio with clinicopathological characteristics in patients with papillary thyroid cancer. Endocrinol Metab (Seoul). 2015; 30(4):494–501.

16. Han SW, Kang SY, Kim SK, Youn HJ, Jung SH. Clinical significance of blood neutrophil-to-lymphocyte ratio in patients with papillary thyroid carcinoma. Korean J Endocr Surg. 2014; 14(4):184–189.

17. Pak K, Suh S, Kim SJ, Kim IJ. Prognostic value of genetic mutations in thyroid cancer: a meta-analysis. Thyroid. 2015; 25(1):63–70.

18. Lang BH, Ng CP, Au KB, Wong KP, Wong KK, Wan KY. Does preoperative neutrophil lymphocyte ratio predict risk of recurrence and occult central nodal metastasis in papillary thyroid carcinoma. World J Surg. 2014; 38(10):2605–2612.

19. Liu CL, Lee JJ, Liu TP, Chang YC, Hsu YC, Cheng SP. Blood neutrophil-to-lymphocyte ratio correlates with tumor size in patients with differentiated thyroid cancer. J Surg Oncol. 2013; 107(5):493–497.

20. Gong W, Yang S, Yang X, Guo F. Blood preoperative neutrophil-to-lymphocyte ratio is correlated with TNM stage in patients with papillary thyroid cancer. Clinics (Sao Paulo). 2016; 71(6):311–314.

21. Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010; 140(6):883–899.

22. Hong IS. Stimulatory versus suppressive effects of GM-CSF on tumor progression in multiple cancer types. Exp Mol Med. 2016; 48(7):e242.

23. Powell DR, Huttenlocher A. Neutrophils in the tumor microenvironment. Trends Immunol. 2016; 37(1):41–52.

24. Liu J, Du J, Fan J, Liu K, Zhang B, Wang S, et al. The neutrophil-to-lymphocyte ratio correlates with age in patients with papillary thyroid carcinoma. ORL J Otorhinolaryngol Relat Spec. 2015; 77(2):109–116.

25. Ito Y, Kudo T, Takamura Y, Kobayashi K, Miya A, Miyauchi A. Prognostic factors of papillary thyroid carcinoma vary according to sex and patient age. World J Surg. 2011; 35(12):2684. 2690.

26. Gwak MS, Choi SJ, Kim JA, Ko JS, Kim TH, Lee SM, et al. Effects of gender on white blood cell populations and neutrophil-lymphocyte ratio following gastrectomy in patients with stomach cancer. J Korean Med Sci. 2007; 22:S104–S108.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download