Abstract
Riedel's thyroiditis is a rare fibrotic condition that results in the destruction of the thyroid and infiltration into surrounding tissues. The exact etiology is not yet clear, although systemic fibrosing disorder, a variant of Hashimoto's thyroiditis, a primary inflammatory disorder of the thyroid, and even a manifestation of end-stage subacute thyroiditis has been suggested. Although various treatments have been applied, no definitive treatment has yet been established. We report a case of Riedel's thyroiditis treated without complications using microscopic surgery. A 54-year-old man visited our clinic presenting with neck tightness and a left neck mass. A gun biopsy revealed a benign thyroid mass, although the radiologic findings showed a malignant thyroid tumor with invasion into the trachea and strap muscles. The patient underwent a left hemi-thyroidectomy and shaving of the trachea, esophagus and recurrent laryngeal nerve under microscopy. The final pathology revealed Riedel's thyroiditis combined with Hashimoto's thyroiditis. The patient had symptomatic relief without vocal fold paralysis and hypocalcemia. Surgical treatment using microscopic dissection can be considered to be one of treatment option for Riedel's thyroiditis.
Riedel's thyroiditis is a rare inflammatory disease of the thyroid gland and has been reported in 0.05% of thyroid surgeries. It was first described by Bernhard Riedel in 1896 as a fibro-inflammatory process associated with thyroid infiltration. The etiology of Riedel's thyroiditis is unknown, although an autoimmune process is the most probable etiology. Recently, several authors have proposed that this inflammatory condition of the thyroid is a local manifestation of a systemic fibrotic process or an autoimmune process. The condition is characterized by an overgrowth of progressively fibrosing connective tissue that may invade surrounding structures. Treatments for Riedel's thyroiditis have been applied, including surgery, medication, irradiation and isotope therapy, although no definitive treatment currently exists. Surgery has been deferred to a second-line treatment because of a tendency of incomplete resection owing to the high risk of complications. In this paper, we report a case of Riedel's thyroiditis that was successfully treated by performing microscopic surgery.
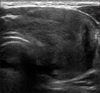
A 50-year-old male was referred to our clinic, presenting with a 1-month history of aggravated neck tightness and a 3-year history of a palpable neck mass. He had a 1-year history of diabetes mellitus and was taking metformin. Physical examination revealed a 5-cm-sized mass with firm density in the left thyroid gland. Laryngoscopy showed normal vocal fold movement. Computed tomography (CT) showed a 4.3×4.1×3.2 cm thyroid mass with invasion into the trachea and strap muscle (Fig. 1). Thyroid ultrasonography revealed a hypoechoic lesion with extracapsular invasion in the left thyroid lobe (Fig. 2). Bronchoscopy showed no definite intra-luminal invasion of a thyroid tumor. Thyroid function tests showed normal T3, T4, TSH and calcitonin levels and elevated anti-microsomal antibody (>600 IU/mL). Thyroid scintigraphy revealed decreased and nonhomogenous uptake. Fine-needle aspiration was performed, but the cytology report indicated insufficient cellularity. Core needle biopsy followed, and the pathology indicated a benign fibrous and myofibroblastic lesion with no thyroidal tissue.
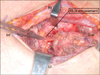
Surgery was performed to confirm the diagnosis and remove the thyroid tumor. During the operation, the right thyroid gland appeared normal, while the left thyroid mass was firm and fixed to the adjacent tissues. A frozen biopsy was taken from the isthmus and demonstrated a benign spindle cell lesion with dense fibrosis. The tumor has invaded the strap muscle, trachea and esophagus, encasing the recurrent laryngeal nerve (Fig. 3). Because the frozen biopsy revealed a benign lesion, gross total tumor resection using microscopy was chosen. Total thyroidectomy was performed, and the left strap muscle was resected with the thyroid mass with shaving the tumor off the trachea and esophagus (Fig. 4). The tumor around the recurrent laryngeal nerve was removed by piecemeal resection, using micro-scissors under a microscopic view.
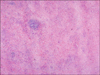
The histopathological findings revealed fibrosis, the growth of hyalinized dense collagen tissue with the involvement of muscles and nerve fibers and atrophy of the thyroid tissue (Fig. 5). In the immunohistochemistry study, EMA, cytokeratin, thyroglobulin, and calcitonin were negative, while vimentin, LCA, CD20, and CD3 were positive. The final diagnosis was Riedel's thyroiditis. The patient's postoperative vocal fold movement was normal. The patient noted relief of his neck tightness after surgery. Serum IgG and IgG4 levels were elevated (IgG 1120 mg/dL, IgG4 187 mg/dL). The patient was followed up with no additional treatment for 5 years and there was no evidence of recurrence in the neck by ultrasonography during follow-up.
Riedel's thyroiditis is a rare disease, and it has been reported to occur in 0.06% of thyroid surgeries and 1.06 of every 100,000 people. It has been reported to have a higher incidence in females than males and commonly occurs in patients aged between 30 and 50 years.1)
The etiology of Riedel's thyroiditis is still unclear, and there is controversy regarding whether it is a primary autoimmune process, a variant of Hashimoto's thyroiditis, or a primary fibrotic disease. The evidence supporting autoimmune mechanisms of Riedel's thyroiditis includes the association of Riedel's thyroiditis with Hashimoto's thyroiditis2) and Graves' disease3) and that one-third of patients with Riedel's thyroiditis develop other associated fibrosing disorders within 10 years.1)
Recently, IgG4-related systemic disease has received attention as the possible etiology of Riedel's thyroiditis. IgG4-related systemic disease affects medium and small veins in tissues and leads to an obliterated phlebitis, which is demonstrable with histopathology. Elevated serum IgG4 levels are frequently identified and have proven to be a useful tool in the identification of the nature of the underlying inflammatory disease. Most recently, investigators have directly linked Riedel's thyroiditis to IgG4-related systemic disease by demonstrating excessive numbers of IgG4+ plasma cells in clinically diagnosed thyroid histology samples by immunohistochemistry.4) In our case, the elevated serum IgG4 level may suggest that IgG4-related disease played a role in the etiology.
A definite diagnosis of Riedel's thyroiditis is based on histopathological findings. The histopathological findings of Riedel's thyroiditis include proliferating fibrous tissue, bands of hyalinized collagen, and prominent inflammatory infiltration of lymphocytes and plasma cells. In the head and neck region, the histopathological differential diagnosis of Riedel's thyroiditis includes fibromatosis, nodular fasciitis, fibrosarcoma, a wall of chronic abscess, and chronic histoplasmosis.5) In addition to the difficulty of the differential diagnosis of the disease from thyroid malignancies, papillary thyroid carcinoma was also shown to coexist in two of the three simultaneous Riedel's thyroiditis and fibrosing Hashimoto's thyroiditis cases,6) and an association between follicular carcinoma and Riedel's thyroiditis has also been reported.7) In our case, concomitant Hashimoto's thyroiditis was present.
The treatment of Riedel's thyroiditis varies. Although surgery was initially the primary treatment performed for Riedel's thyroiditis, drug therapy is the current mainstay of treatment. Steroid administration has been reported to be effective for Riedel's thyroiditis.8) Steroid treatment resulted in the regression of fibrosclerosis in a case of Riedel's thyroiditis in which surgery was ineffective.9) There was a report that recurrent laryngeal nerve paralysis was reversible after steroid administration.1)
Surgery is generally reserved for lesions that do not respond to steroids.8) Due to the obliteration of tissue planes by the fibrotic process, the danger of hypoparathyroidism and recurrent laryngeal nerve damage makes aggressive surgical intervention to be problematic.10) When the complete resection of a mass is impossible, open biopsy, isthmectomy and the excision of at least a portion of the thyroid have been reported to be good treatment options.11) Extensive surgical procedures may be considered inappropriate in the management of Riedel's thyroiditis because of the high risk of complications. However, another report recommends the complete resection of Riedel's thyroiditis to relieve pressure symptoms.12) In addition, the recurrent laryngeal nerve should be preserved even if it is paralyzed because recovery of the nerve and subsequent improved voice symptoms after decompression has been reported.7)13) Meticulous dissection using microscope or intraoperative nerve monitoring would be helpful for reducing recurrent laryngeal nerve injury. In our case, although the fibrotic mass encased the recurrent laryngeal nerve and invaded the trachea and esophagus, we could remove the mass by microsurgery without any complications. This case may suggest that surgical treatment can be an alternative treatment option for Riedel's thyroiditis.
Figures and Tables
Fig. 1
Radiologic evaluation. CT scan shows large exophytic mass in left thyroid gland showing extracapsular invasion (arrows).
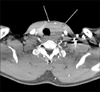
Fig. 2
Ultrasonographic evaluation. Hypoechoic mass is shown in left thyroid gland with suspicious tracheal invasion.
References
1. Yasmeen T, Khan S, Patel SG, Reeves WA, Gonsch FA, de Bustros A, et al. Clinical case seminar: Riedel's thyroiditis: report of a case complicated by spontaneous hypoparathyroidism, recurrent laryngeal nerve injury, and Horner's syndrome. J Clin Endocrinol Metab. 2002; 87(8):3543–3547.

2. Julie C, Vieillefond A, Desligneres S, Schaison G, Grunfeld JP, Franc B. Hashimoto's thyroiditis associated with Riedel's thyroiditis and retroperitoneal fibrosis. Pathol Res Pract. 1997; 193(8):573–577. discussion 8.

3. Heufelder AE, Hay ID. Evidence for autoimmune mechanisms in the evolution of invasive fibrous thyroiditis (Riedel's struma). Clin Investig. 1994; 72(10):788–793.

4. Dahlgren M, Khosroshahi A, Nielsen GP, Deshpande V, Stone JH. Riedel's thyroiditis and multifocal fibrosclerosis are part of the IgG4-related systemic disease spectrum. Arthritis Care Res (Hoboken). 2010; 62(9):1312–1318.

5. Frankenthaler R, Batsakis JG, Suarez PA. Tumefactive fibroinflammatory lesions of the head and neck. Ann Otol Rhinol Laryngol. 1993; 102(6):481–482.

6. Baloch ZW, Feldman MD, LiVolsi VA. Combined Riedel's disease and fibrosing hashimoto's thyroiditis: a report of three cases with two showing coexisting papillary carcinoma. Endocr Pathol. 2000; 11(2):157–163.

7. Hao SP, Chen JF, Yen KC. Riedel's thyroiditis associated with follicular carcinoma. Eur Arch Otorhinolaryngol. 1999; 256(9):470–472.

8. Hostalet F, Hellin D, Ruiz JA. Tumefactive fibroinflammatory lesion of the head and neck treated with steroids: a case report. Eur Arch Otorhinolaryngol. 2003; 260(4):229–231.

9. Bagnasco M, Passalacqua G, Pronzato C, Albano M, Torre G, Scordamaglia A. Fibrous invasive (Riedel's) thyroiditis with critical response to steroid treatment. J Endocrinol Invest. 1995; 18(4):305–307.

10. Hennessey JV. Clinical review: Riedel's thyroiditis: a clinical review. J Clin Endocrinol Metab. 2011; 96(10):3031–3041.
11. Fatourechi MM, Hay ID, McIver B, Sebo TJ, Fatourechi V. Invasive fibrous thyroiditis (Riedel thyroiditis): the Mayo Clinic experience, 1976-2008. Thyroid. 2011; 21(7):765–772.

12. Papi G, Corrado S, Cesinaro AM, Novelli L, Smerieri A, Carapezzi C. Riedel's thyroiditis: clinical, pathological and imaging features. Int J Clin Pract. 2002; 56(1):65–67.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download