Abstract
Coexistence of moyamoya disease and Graves' disease is rare. A 41-year-old woman presented with symptoms of left-sided hemiparesis and dysarthria. Magnetic resonance imaging and angiography revealed acute infarction of the right thalamus and occipital lobe with complete obstruction of the distal internal carotid arteries and obstruction of the right P2. Free thyroxine, thyroid-stimulating hormone (TSH), and TSH receptor antibody levels were 79.33 pmol/L, 0.007 uIU/mL, and 151.5 u/L, respectively. She received antiplatelet therapy and standard antithyroid drug dose. After admission, seizure and unexplained fever occurred. The thyroid storm score (Burch and Wartofsky scale) was 90 points. After intensive treatment, mental status and thyrotoxicosis-related symptoms ameliorated and vital signs stabilized. We describe a case of thyroid storm following cerebrovascular ischemic events in a Korean woman with moyamoya disease and Graves' disease. Thyroid storm combined with cerebrovascular events can lead to severe morbidity and mortality. Prompt recognition and strict management are crucial.
Moyamoya disease (MMD) is a cerebrovascular condition that is characterized by progressive occlusion of the terminal portion of the internal carotid artery, resulting in the formation of collateral abnormal vessels at the base of the brain. MMD has been reported to be associated with various disease entities.1) Coexistence of MMD and Graves' disease is rare; however, various cases of concurrent MMD and Graves' disease have been reported recently. Thyroid storm is a life-threatening endocrine condition associated with uncontrolled hyperthyroidism and a high mortality rate. Thyroid storm in a patient with underlying MMD can lead to increased morbidity and mortality rates. We herein describe a case of thyroid storm following cerebrovascular ischemic events in a Korean patient with MMD and Graves' disease.
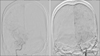
A 41-year-old Korean woman was referred to our emergency department owing to symptoms of leftsided hemiparesis and dysarthria. The patient had been diagnosed with Graves' disease about 10 years ago and had been taking antithyroid drug irregularly. There was no history of treatment with other drugs or alcohol abuse. The patient showed an alert mental state, slurred speech, and left-sided weakness corresponding to the MRC (Medical Research Council) grade II. A neurological examination demonstrated left-sided hemiparesis. A physical examination revealed bilateral exophthalmos and a diffuse goiter (Grade 2, according to the WHO differentiation). In the emergency room, the patient's blood pressure was 125/75 mmHg, heart rate was 109 bpm, respiratory rate was 18 breaths per minute, and body temperature was 36.2℃. Electrocardiography revealed sinus tachycardia and magnetic resonance imaging (MRI) of the brain revealed acute infarction of the right thalamus and occipital lobe (Fig. 1). Cerebral angiography revealed complete obstruction of both distal internal carotid arteries and obstruction of the right P2 (Fig. 2). Thyroid function test revealed the following: thyroid-stimulating hormone (TSH), 0.007 microunits/mL (reference range, 0.55–4.78 microunits/mL); triiodothyronine, 3.60 ng/mL (reference range, 0.78–1.82 ng/mL); free thyroxine (T4), 79.33 pmol/L (reference range, 11.5–22.7 pmol/L); and TSH receptor antibody, 151.5 U/L (reference range, 0–10 U/L). A thyroid ultrasonography revealed a diffusely enlarged thyroid gland without any nodule or mass. Thyroid scintigraphy revealed homogeneously increased Tc-99m uptake (thyroid uptake: 50.5%) (Fig. 3).
The patient was admitted to the neurology department and diagnosed with MMD combined with acute cerebral infarction and Graves' disease. The patient received antiplatelet therapy and propylthiouracil (200 mg/day). As the patient exhibited an alert mental state and stable vital signs, she was prescribed a standard dose of antithyroid drug. However, after admission, the patient suddenly developed an unexplained fever and had a seizure. The mental status of patient was checked as stupor and seizure was repeated. The vital signs were as follows: blood pressure, 170/113 mmHg; heart rate, 140 bpm (tachycardia); and fever, 38.8℃. Physical examination revealed bibasilar crackles and an irregular rhythm. Electrocardiography revealed atrial fibrillation with a rapid ventricular response (Fig. 4) and chest radiography showed cardiomegaly (Fig. 5). To exclude additional infarction or cerebral hemorrhage due to aggravated neurologic symptoms, brain MRI was performed again, which did not reveal any evidence of newly progressed infarction or hemorrhagic lesion and there was no interval change compared with the prior image. The thyroid storm score (Burch and Wartofsky score) was 90 points.2) For thyroid storm management, we initiated high-dose propylthiouracil, Lugol's solution, and hydrocortisone. An echocardiogram revealed global hypokinetic wall movement with mild left ventricular systolic dysfunction (ejection fraction, 48%). Rate control and management for heart failure were conducted simultaneously. After intensive treatment, the patient's mental status improved and thyrotoxicosis-related symptoms ameliorated. Moreover, her vital signs stabilized and she was discharged in an improved state.
After 6 weeks of treatment, hyperthyroidism had stabilized (free T4, 18.89 pmol/L; TSH, 0.010 uIU/mL) and neurologic symptoms had ameliorated significantly. The patient maintained regular antithyroid medication and had no additional cerebral complications.
To date, about 50 cases of concurrent MMD and Graves' disease have been described in the literature.3) In Korea, interesting cases associated with MMD and Graves' disease were reported.4)5) Although the relationship between Graves' disease and cerebrovascular accidents in MMD is unclear, the coexistence of both diseases is rare and noteworthy.6)
MMD is symptomatic whenever the collateral vessels fail to compensate for the cerebral blood flow deficit produced by the progressive stenotic lesion in the major cerebral arteries.7) In the thyrotoxicosis state, excessive thyroid hormones can alter vascular reactivity and cause cerebral perfusion impairment. Therefore, cerebrovascular ischemic symptoms in MMD can be precipitated by activities associated with thyrotoxicosis.1)8) Moreover, previous reports have suggested that altered cerebral hemodynamics and hypercoagulability in thyrotoxicosis may trigger vascular attacks in patients with MMD.9)10)
Some physicians have argued that an autoimmune mechanism, which contributes to the development of Graves' disease, may also play an important role in the onset and progression of MMD-related cerebrovascular events.7) Lei et al.11) demonstrated that increased thyroid function and autoantibodies are associated with MMD. A Korean study observed that patients with MMD were more likely to have elevated thyroid autoantibody levels than those with non-MMD strokes, despite being in a euthyroid state.12) Similarly, the patient in our study had high levels of TSH receptor antibody when symptoms developed. Another possible link between these disorders is atherosclerosis. Colleran et al.13) demonstrated a positive correlation between free T4 levels and both homocysteine and methylmalonic acid levels, suggesting that thyrotoxicosis may induce hyperhomocysteinemia. As hyperhomocysteinemia has been implicated in atherosclerotic and embolic disorders,14)15) it could be another key to the pathophysiology of MMD.16) In our case, due to the patient had a history of uncontrolled longstanding Graves' disease, aggravation of MMD can be affected by chronic hyperthyroidism.
Although a thyroid storm associated with cerebrovascular ischemic events is very rare in patients with both MMD and Graves' disease, it is still a life-threatening condition that can cause severe morbidity and mortality. Hsu et al.17) reported a case of Graves' disease with thyroid storm associated with MMD in 2006, which unlike previously reported cases, progressed rapidly and was ultimately fatal.
In our case, the thyroid storm occurred during the management of cerebral infarction. Thyroid storm is typically triggered by stressful medical events or conditions. The cerebrovascular accidents may contribute to the occurrence of thyroid storm. Although the order of the incidents is not clear, if transient ischemic attacks or cerebral infarction occurs in a patient with both Graves' disease and MMD, it can also induce a thyroid storm. Prompt recognition and treatment are crucial for improving prognosis. Furthermore, maintenance of a long-term euthyroid state is essential and it is important to prevent a relapse of hyperthyroidism after normal thyroid function is restored in MMD patients.1)
Here, we report a case of thyroid storm and acute cerebral infarction associated with MMD in a patient with Graves' disease. The case has enhanced our understanding of a few aspects. First, we should keep in mind the possibility of combined problems with GD, such as MMD, especially patients that have neurological signs and symptoms. In such cases, further studies are warranted. Second, the cerebrovascular ischemic events can be a triggering factor (or risk factor) for thyroid storm, like in our case. Therefore, if transient ischemic attacks or cerebral infarction occurs in a patient with Graves' disease combined with MMD, emergent treatment should be initiated.
Figures and Tables
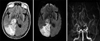 | Fig. 1Brain magnetic resonance of T2 FLAIR axial image, diffusion-weighted image and brain MR angiography maximum intensity projection showing acute infarction of the right thalamus and occipital lobe. |
References
1. Im SH, Oh CW, Kwon OK, Kim JE, Han DH. Moyamoya disease associated with Graves disease: special considerations regarding clinical significance and management. J Neurosurg. 2005; 102(6):1013–1017.

2. Burch HB, Wartofsky L. Life-threatening thyrotoxicosis. Thyroid storm. Endocrinol Metab Clin North Am. 1993; 22(2):263–277.

3. Ren SC, Gao BQ, Yang WL, Feng WX, Xu J, Li SW, et al. Von Willebrand factor and coagulation factor VIII in Moyamoya disease associated with Graves' disease: a case report. Exp Ther Med. 2016; 12(5):3195–3200.

4. Back JH, Kang HM, Min BD, Gil SH, Kim SJ, Oh BC, et al. A case of Graves' disease associated with myasthenia gravis and complicated with Moyamoya disease. Korean J Med. 2010; 79(2):195–200.
5. Shin DW, Seo JY, Lee JG, Kim JS, Lee KB, Roh H, et al. Acute ischemic stroke in Moyamoya disease associated with thyrotoxic crisis. J Korean Neurol Assoc. 2014; 32(2):95–97.
6. Cheon CK, Kim SY, Yoo JH. Two adolescent patients with coexistent Graves' disease and Moyamoya disease in Korea. Korean J Pediatr. 2014; 57(6):287–291.

7. Shen AL, Ryu SJ, Lin SK. Concurrent moyamoya disease and Graves' thyrotoxicosis: case report and literature review. Acta Neurol Taiwan. 2006; 15(2):114–119.
8. Sasaki T, Nogawa S, Amano T. Co-morbidity of moyamoya disease with Graves' disease. report of three cases and a review of the literature. Intern Med. 2006; 45(9):649–653.

9. Siegert CE, Smelt AH, de Bruin TW. Superior sagittal sinus thrombosis and thyrotoxicosis. Possible association in two cases. Stroke. 1995; 26(3):496–497.

10. Ni J, Zhou LX, Wei YP, Li ML, Xu WH, Gao S, et al. Moyamoya syndrome associated with Graves' disease: a case series study. Ann Transl Med. 2014; 2(8):77.
11. Lei C, Wu B, Ma Z, Zhang S, Liu M. Association of moyamoya disease with thyroid autoantibodies and thyroid function: a case-control study and meta-analysis. Eur J Neurol. 2014; 21(7):996–1001.

12. Kim SJ, Heo KG, Shin HY, Bang OY, Kim GM, Chung CS, et al. Association of thyroid autoantibodies with moyamoya-type cerebrovascular disease: a prospective study. Stroke. 2010; 41(1):173–176.

13. Colleran KM, Ratliff DM, Burge MR. Potential association of thyrotoxicosis with vitamin B and folate deficiencies, resulting in risk for hyperhomocysteinemia and subsequent thromboembolic events. Endocr Pract. 2003; 9(4):290–295.

14. Iso H, Moriyama Y, Sato S, Kitamura A, Tanigawa T, Yamagishi K, et al. Serum total homocysteine concentrations and risk of stroke and its subtypes in Japanese. Circulation. 2004; 109(22):2766–2772.

15. van Diemen-Steenvoorde R, van Nieuwenhuizen O, de Klerk JB, Duran M. Quasi-moyamoya disease and heterozygosity for homocystinuria in a five-year-old girl. Neuropediatrics. 1990; 21(2):110–112.

16. Lee R, Sung K, Park YM, Yu JJ, Koh YC, Chung S. A case of Moyamoya disease in a girl with thyrotoxicosis. Yonsei Med J. 2009; 50(4):594–598.

17. Hsu SW, Chaloupka JC, Fattal D. Rapidly progressive fatal bihemispheric infarction secondary to Moyamoya syndrome in association with Graves thyrotoxicosis. AJNR Am J Neuroradiol. 2006; 27(3):643–647.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download