Abstract
Sweet's syndrome, or acute febrile neutrophilic dermatosis, occurs in association with autoimmune diseases such as Hashimoto's thyroiditis but is rare in Graves' disease, in which all cases are induced by propylthiouracil (PTU). We report a case of Sweet's syndrome in a patient with Graves' disease treated with methimazole (MMI) during three weeks. A 34-year-old man presented with the acute onset of high fever, skin rashes on the whole body, arthralgia, and acroparesthesia. Laboratory results showed leukocytosis and elevated C-reactive protein. MMI first stopped and antibiotics and antihistamine therapy started, but his symptoms dramatically improved after oral prednisolone. Graves' disease has again been treated by MMI because of his aggravated ophthalmopathy. After one year of retreatment with MMI, there has been no recurrence of Sweet's syndrome, supporting that Sweet's syndrome in this case was not related to MMI exposure. To our knowledge, this is the first report of Sweet's syndrome associated with Graves' disease per se but not PTU or MMI use.
Sweet's syndrome, or acute febrile neutrophilic dermatosis, is an infrequent skin disease characterized by sudden onset of fever, leukocytosis, tender erythematous plaques or nodules, and diffuse infiltrate consisting predominantly of mature neutrophils that are typically located in the upper dermis without vasculitis.12) Sweet's syndrome is associated with many conditions including cancer, infections, inflammatory bowel disease, drugs, pregnancy, and autoimmune connective tissue diseases.13) Sweet's syndrome can also occur in patients with Hashimoto's thyroiditis,456) and rarely in patients with Graves' disease, in which all reported cases were caused by use of propylthiouracil (PTU).789) Extracutaneous manifestations of Sweet's syndrome can present in the ocular mucosa and mouth, as well as in the bone, central nervous system, kidneys, intestines, liver, heart, lungs, muscles, and spleen.18) Here we report a case of Sweet's syndrome associated with Graves' disease per se but not a drug use.
A 34-year-old man was referred for typical thyrotoxic symptoms and signs, diffuse goiter, and ophthalmopathy. He had heat intolerance and sweating, palpitations, 20 kg weight loss despite increased appetite and oral intake, and hand tremor during about four months. His pulse rate was 140 beats/minute with sinus rhythm and his thyroid was diffusely enlarged to four to five times its normal size. He also had ophthalmopathy grade 2 including lid retractions, periorbital edema, and proptosis (18 mm). He had no other medical diseases or surgery on the past history and no specific diseases including autoimmune thyroid disease on family history. He was smoker but non- drinker. Thyroid function tests were as follows: free thyroxine (T4) 8.33 ng/dL (0.78–1.94), thyrotropin (TSH) 0.01 mIU/L (0.25–4.0), anti-TSH receptor antibody (anti-TSH-R) 21.4 IU/L (0–1.5), anti-thyroid peroxidase antibody (anti-TPO) 586.1 mIU/L (0–100), and anti-thyroglobulin antibody (anti-Tg) 509.1 mIU/L (0-70). There was a diffuse enlargement of thyroid glands and increased technetium uptake in thyroid scintigraphy. He was diagnosed with Graves' disease and prescribed with methimazole (MMI) 30 mg daily and betaxolol 10 mg daily as a beta-adrenergic blocker.
After three weeks, he presented to the emergency department with the acute onset of fever and multiple pruritic erythematous wheals and flares on the whole body during three days. He stopped all medications for two days after symptoms. The patient's clinical details were as follows: blood pressure 146/72 mmHg, heart rate 105 beats/minute, respiration rate 20/minute, and body temperature 38.8℃. Laboratory results showed leukocytosis (WBC 15,190/µL, neutrophil 88.5%) and elevated C-reactive protein (CRP) of 11.0 mg/dL (0–0.5). The hepatic and renal functions and urine analysis were normal. Blood, urine, and sputum cultures were obtained and ceftizoxime and antipyretics therapy for fever were initiated. Intravenous (chlorpheniramine maleate) and oral antihistamines (azelastine Hcl, bepotastine, and ketotifen fumarate) were administrated for urticaria. MMI treatment and beta-blocker were discontinued. Itching and ulticaria improved slightly but the fever persisted. Laboratory results revealed erythrocyte sedimentation rate (ESR) 28 mm/hr (0–20), CRP levels 14.19 mg/dL three days after admission. Thyroid function tests were free T4 1.25 ng/dL, TSH 0.02 mIU/L, and anti-TSH-R 21.3 IU/L. Antibiotic therapy was changed into ceftriaxone due to persistent fever, and potassium iodide (1 g/mL of water) 2 drops 3 times per day was started for Graves' disease with oral beta-blocker. He also had painful erythematous papules with tenderness on the left palm, arthralgia and tenderness on the right second and third metatarsophalangeal joints, and acroparesthesia on the both hands and feet. Computed tomographic images of the chest and abdomen and cultures for work-up of fever were normal. Serologic tests were negative for antinuclear antibody, anti-neutrophil cytoplasmic antibody (ANCA), and rheumatoid factor. There was no definite electrophysiological evidence of peripheral neuropathy in nerve conduction velocity study. A skin biopsy was done at the right arm. On the considering his all clinical manifestations, he was strongly suspected with Sweet's syndrome and treated with prednisolone 20 mg per day. His fever resolved shortly after treatment of prednisolone. His arthralgia and acroparesthesia as well as skin rash improved after starting steroid therapy and he discharged (Fig. 1). One week after discharge, his previous symptoms resolved completely and prednisolone stopped. A skin biopsy from right arm showed only mild acanthosis. But he also newly developed conjunctival injection and swelling, crust and vesicles in upper eyelid, and dendritic corneal ulcer on the right eye after discharge. Herpetic keratitis resolved after administration of acyclovir 3% eye ointment and levofloxacin 0.5% eye drop. However, he was again hyperthyroidism state (free T4 7.77 ng/dL and TSH 0.005 mIU/L) accompanied with aggravated ophthalmopathy (proptosis 23 mm, grade 3), so thyroid surgery or radioactive iodine therapy could not be performed as definitive therapy for Graves' disease. To the best of our knowledge, there had been no reported cases of Sweet's syndrome caused by MMI for the treatment of Graves' disease. Potassium iodide stopped and MMI 10 mg once daily started for Graves' disease. There was no recurrence of Sweet's syndrome after MMI challenge, although the dose of MMI increased to 30 mg daily for control of hyperthyroidism thereafter. After about one year of follow-up, he remained euthyroid state with MMI 5 mg daily (Fig. 2), there has been no recurrence of Sweet's syndrome and further investigations have revealed no underlying malignancy.
Anti-thyroid drugs (ATDs) including MMI, PTU, and carbimazole, a precursor of MMI, are thionamide drugs, which are commonly used as first-line therapy in the treatment of Graves' disease.10) These medications can be associated with potential adverse reactions such as rash, joint pain, agranulocytosis, and hepatotoxicity. PTU very infrequently causes ANCA-positive small-vessel vasculitis, with a risk that appears to increase with time. The opposite trend is observed for the adverse effects seen with ATDs, which typically occur early in the course of treatment.11) Minor cutaneous allergic reactions may be managed with concurrent antihistamine therapy, changing to radioactive iodine or surgery, or switching to the other ATD. A differential white blood cell count and liver function should be obtained when there are symptoms suggestive of agranulocytosis or hepatic injury. In a patient developing agranulocytosis or other serious side effects while taking ATDs, use of ATDs is absolutely contraindicated owing to risk of cross-reactivity between medications.1011)
Sweet's syndrome is an acute febrile neutrophilic dermatosis which is characterized by painful papules and nodules, fever, elevated neutrophil count and ESR, and infiltration of neutrophils into the dermis.128) Sweet's syndrome presents in three clinical setting.1212) The classical or idiopathic type usually presents in middle aged women, and may be associated with upper respiratory tract or gastrointestinal infection, inflammatory bowel disease, or pregnancy. A malignancy-associated form can occur as a paraneoplastic syndrome of established cancer or may be the first sign of malignancy or its recurrence. The drug-induced type most commonly occurs in patients treated with granulocyte-colony stimulating factor (G-CSF), although many case reports describe an association with several drugs including antibiotics (minocycline, nitrofurantoin, trimethoprim–sulfamethoxazole), antiepileptics (carbamazepine, diazepam), hydralazine, clozapine, contraceptives, furosemide, retinoids, and nonsteroidal anti-inflammatory agents (e.g., celecoxib, diclofenac), as well as PTU.1212) The classical or malignancy-induced Sweet's syndrome is diagnosed based on fulfilling the two major (painful skin lesion and typical histopathologic evidence) and two of four minor criteria. The diagnostic criteria for drug-induced Sweet's syndrome require two major criteria of classical Sweet's syndrome and three additional criteria including temporal relationships between clinical manifestations and a drug ingestion or withdrawal (Table 1).128) Systemic corticosteroids are the gold standard for the treatment of Sweet's syndrome. Topical and intralesional corticosteroids, oral therapy with potassium iodide or colchicine, indomethacin, clofazimine, cyclosporine, and dapsone are also considered as other therapeutic agents.18)
The pathogenesis of Sweet's syndrome remains to be definitely determined. An infection or a hypersensitivity reaction to eliciting bacterial, viral, or tumor antigen may promote the development of Sweet's syndrome. Circulating antibodies, cytokines, dermal dendrocytes, human leukocyte antigen serotypes, immune complexes, and leukotactic mechanisms have all been postulated to contribute to the pathogenesis of Sweet's syndrome.12) The most frequently proposed hypothesis for the pathogenesis of Sweet's syndrome is the overproduction and inappropriate regulation of inflammatory cytokines such as interleukin (IL)-1, IL-3, IL-6, IL-8, G-CSF and granulocyte macrophage colony stimulating factor (GMCSF).2) Significantly elevated levels of helper T-cell type 1 cytokines (IL-2 and interferon-gamma) and normal levels of a helper T-cell type 2 cytokine (IL-4) were observed in Sweet's syndrome patient serum.1) Increased levels of G-CSF can explain leukocytosis, neutrophilic dermatosis and skin lesions, while increased levels of IL-6 are thought to be associated with fever and pain.8)
The possible link between Sweet's syndrome and autoimmune thyroid disease is supported by the proposed role of immune-mediated T cytokine expression in both diseases.6) Magri et al.13) reported a case of a 50-year-old woman who had a relapse of Sweet's syndrome associated with changes in thyroid autoimmunity. She was documented anti-TPO and anti-Tg positivity (previously negative) and a free T4 within the low normal range during the relapse of Sweet's syndrome. The authors mentioned that the cytokine cascade occurring in Sweet's syndrome can stimulate human leukocyte antigen class II expression on immune thyroid epithelial cells and may play a cytotoxic effect on and induce apoptosis of thyroid cells.12) The association of Sweet's syndrome with Graves' disease is uncommon. Only three cases have been reported in the literature, two reports by PTU and one report by G-CSF.789) The first case was a 37-year-old woman who had been diagnosed with Graves' disease three years ago.7) She was treated with PTU without any problems for the first two years. PTU had been recommended at a dose 100 mg three times daily for three months before the presentation with Sweet's syndrome. She had no other medical or medication history.7) The second case was a 33-year-old woman treated with PTU for 13 months.9) The last case was a 43-year-old woman who developed fever and pancytopenia as an adverse effect of PTU after the treatment with PTU 300 mg daily for three weeks.8) She was treated with G-CSF for agranulocytosis and developed Sweet's syndrome by G-CSF use. ANCA was positive after using PTU in all three cases, suggesting a pathogenic role of PTU-induced ANCA in Sweet's syndrome.789)
The present patient developed fever, skin rash, arthralgia, acroparesthesia after initiation of MMI and beta-blocker. Itching urticarial lesions on the whole body were considered as MMI-induced minor side effects and controlled by antihistamines. But high fever non-responsive to antibiotics, painful erythematous papules, arthralgia, acroparesthesia, leukocytosis, neutrophilia, elevated ESR and CRP levels, and an excellent response to corticosteroid strongly suggested Sweet's syndrome, although skin biopsy revealed no Sweet's syndrome because it was done at other site and inadequate. Furthermore, his Sweet's syndrome was not induced by MMI, because there was no temporal relationship between clinical manifestations and a drug withdrawal or challenge. To our knowledge, there has been no reported case of Sweet's syndrome by MMI use, and this is the first report of Sweet's syndrome associated with Graves' disease per se. The present case has the differences with previous reported cases about Sweet's syndrome associated with Graves' disease: male, no PTU use and negative ANCA. It is noticeable that his thyroid function state showed a big and rapid improvement after taking MMI. It supports the role of immune-mediated T cytokine expression in both diseases again and that many pathogenic mechanisms proposed for Sweet's syndrome are potentially able to affect thyroid gland.613)
In conclusion, clinicians should be aware of very rare associations with Sweet's syndrome and autoimmune thyroid disease, including Graves' disease or rare adverse effects of PTU but not MMI. Our case suggests an expanded differential diagnosis for fever and skin rash in patients with underlying Graves' disease.
Figures and Tables
Fig. 1
Clinical characteristics and laboratory results during the admission. Day 0 represents the day of admission. *,†Peak body temperature before and after the administration of oral prednisolone, respectively. AB: antibiotics, AH: antihistamines, BT: body temperature, CRP: C-reactive protein, DC: discharge, KI: potassium iodide, MMI: methimazole, OPD: outpatient department, PD: prednisolone

Fig. 2
Follow up of thyroid function tests and the dose of methimazole. The reference ranges of thyroid function tests were as follows: free T4 0.78-1.94 ng/dL (gray area), TSH 0.25-4.0 mIU/L (dash line), anti-TSH-R 0-1.5 IU/L. Adm: admission, anti-TSH-R: anti-TSH receptor antibody, free T4: free thyroxine, MMI: methimazole, TSH: thyrotropin
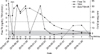
Table 1

*The classical Sweet's syndrome is diagnosed based on fulfilling the two major (1 and 2) and two of four minor criteria (3-6).
†All five criteria (A-E) are required for the diagnosis of drug-induced Sweet's syndrome.
The present case is matched (Y) or not (N) to the diagnostic criteria.
NA: not available
References
1. Cohen PR. Sweet's syndrome--a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis. 2007; 2:34.

2. Raza S, Kirkland RS, Patel AA, Shortridge JR, Freter C. Insight into Sweet's syndrome and associated-malignancy: a review of the current literature. Int J Oncol. 2013; 42(5):1516–1522.

3. Dabade TS, Davis MD. Diagnosis and treatment of the neutrophilic dermatoses (pyoderma gangrenosum, Sweet's syndrome). Dermatol Ther. 2011; 24(2):273–284.

4. Nakayama H, Shimao S, Hamamoto T, Munemura C, Nakai A. Neutrophilic dermatosis of the face associated with aortitis syndrome and Hashimoto's thyroiditis. Acta Derm Venereol. 1993; 73(5):380–381.
5. Medeiros S, Santos R, Carneiro V, Estrela F. Sweet syndrome associated with Hashimoto thyroiditis. Dermatol Online J. 2008; 14(9):10.

6. Francisco CR, Patal PC, Cubillan EA, Isip-Tan IT. Sweet's syndrome associated with Hashimoto's thyroiditis. BMJ Case Rep. 2011; 2011:pii: bcr0220113921.

7. Miller RM, Darben TA, Nedwich J, Savige J. Propylthiouracil-induced antineutrophil cytoplasmic antibodies in a patient with Graves' disease and a neutrophilic dermatosis. Br J Dermatol. 1999; 141(5):943–944.

8. Ozlem C, Deram B, Mustafa S, Koray T, Cuyan D, Ertugrul T. Propylthiouracil-induced anti-neutrophil cytoplasmic antibodies and agranulocytosis together with granulocyte colony-stimulating factor induced Sweet's syndrome in a patient with Graves' disease. Intern Med. 2011; 50(18):1973–1976.

9. Darne S, Natarajan S, Blasdale C. Do antineutrophil cytoplasmic antibodies (ANCA) play a key role in neutrophilic dermatoses? A case of propylthiouracil-induced neutrophilic dermatosis with positive perinuclear ANCA. Clin Exp Dermatol. 2010; 35(4):406–408.

10. Brent GA. Clinical practice. Graves' disease. N Engl J Med. 2008; 358(24):2594–2605.
11. Bahn Chair RS, Burch HB, Cooper DS, Garber JR, Greenlee MC, Klein I, et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid. 2011; 21(6):593–646.

12. Gottlieb CC, Mishra A, Belliveau D, Green P, Heathcote JG. Ocular involvement in acute febrile neutrophilic dermatosis (Sweet syndrome): new cases and review of the literature. Surv Ophthalmol. 2008; 53(3):219–226.

13. Magri F, Gabellieri E, Sorrentino AR, Rizza MI, Chiovato L, Ferrari E. Sweet's syndrome and thyroid diseases: is there a link? Endocr Abstr. 2006; 11:P64.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download