Abstract
Simvastatin is used to reduce plasma cholesterol by inhibiting 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase and is primarily used to treat hypercholesterolemia. This study was conducted to assess the bioequivalence between the generic formulation of simvastatin 20 mg and the branded formulation of simvastatin 20 mg. A generic formulation of simvastatin 20 mg tablet was developed and the pharmacokinetics of the generic formulation were compared with those of the branded formulation of simvastatin 20 mg tablet in 33 healthy male volunteers after a single oral dose in a randomized, open-label, two-period, two-sequence, crossover study. The reference (Zocor®, MSD Korea LTD.) and test (Simvarotin®, Korea Arlico Pharm Co., Ltd.) formulations, two 20 mg tablets each, were administered to all subjects in fasting status. The serial blood samples for pharmacokinetic analysis were collected before dosing and up to 24 hours post-dose, and plasma concentrations of simvastatin were determined by liquid chromatography-tandem mass spectrometry. The pharmacokinetic parameters including Tmax, Cmax, AUClast, AUCinf and t½ were calculated for both formulations by non-compartmental method, and the log-transformed Cmax and AUClast were compared statistically. Geometric mean ratios (90% confidence intervals) of the test to the reference formulation in Cmax and AUClast were 0.9652 (0.8302–1.1223) and 0.9891 (0.8541–1.1455), respectively. No significant differences in tolerability profiles were noted between the two formulations. The two formulations of simvastatin 20 mg tablets exhibited comparable pharmacokinetic profiles and 90% confidence intervals were within the acceptable range of bioequivalence criteria.
Simvastatin is an anti-hyperlipidemic agent primarily used to treat hypercholesterolemia. It specifically inhibits the enzyme 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase. Inhibition of this enzyme results in plasma cholesterol level reduction by inhibiting cholesterol biosynthesis and increasing the number of low-density lipoprotein (LDL) receptors on both hepatic and extrahepatic tissues. The elevation of the number of LDL receptors enhances sequestering of LDL from blood circulation and promotes its catabolism in the liver resulting in lowering of plasma LDL level. Simvastatin is also known to reduce the level of triglyceride and increase high-density lipoprotein cholesterol level.[1]
Simvastatin is an inactive prodrug that is absorbed well through the oral route and undergoes extensive first-pass hepatic metabolism, resulting in its low oral bioavailability (approximately 5%). Simvastatin is hydrolyzed into simvastatin β-hydroxyacid by esterases or paraoxonases in the liver and this metabolite competes for and specifically inhibits HMG-CoA reductase. Simvastatin and simvastatin β-hydroxyacid both exhibit high (approximately 95%) human plasma protein binding;[2] simvastatin β-hydroxyacid is metabolized by cytochrome P450 enzyme. In the 14C-labeled simvastatin study, 13% of the administered dose is excreted through urine whereas 60% of the administered dose is excreted via fecal route.[3] The elimination half-life of simvastatin is 2 hours, which is similar to that of simvastatin β-hydroxyacid (1.9 hours). Owing to its short elimination half-life, long-term administration of simvastatin did not result in accumulation of simvastatin or its metabolite.
The anti-hyperlipidemic drug market is continuously expanding in Korea and is expected to be over US $500 million. A number of simvastatin generic products have been introduced to the market by various manufacturers. One such new generic tablet formulation of simvastatin 20 mg (Simvarotin®) was developed by Korea Arlico Pharm Co., Ltd., Korea. The objective of this study was to evaluate and compare the pharmacokinetic profile and the tolerability of Simvarotin® with that of the branded formulation Zocor® (MSD Korea LTD.).
Simvarotin® (simvastatin 20 mg tablet, Korea Arlico Pharm Co., Ltd.) and Zocor® (simvastatin 20 mg tablet, MSD Korea LTD.) were used as the test and reference investigational products, respectively.
Thirty-four healthy adult male volunteers were enrolled in this study and informed consent was obtained from each prior to the commencement of study. The study was performed according to the Declaration of Helsinki for biomedical research involving human subjects and the rules of Korean Good Clinical Practices were followed. All subjects were in good physical condition as determined by clinical laboratory tests and physical examination. Subjects who took the drugs that might affect the pharmacokinetics of simvastatin 10 days prior to the commencement of study, who participated in other clinical studies within 3 months prior to the commencement of study, or who experienced hypersensitivity to simvastatin were excluded from the study.
This study was designed as a randomized, open-label, two-sequence, two-period crossover study under fasting conditions. Subjects were admitted to the Kyung Hee University Hospital one day prior to the day of dosing and were discharged from the hospital 24 hours after dosing. Subjects were abstained from excessive exercise, smoking, and consuming alcohol or caffeine-containing drinks and kept under fasting state for more than 10 hours before dosing. Subjects in sequence A received two tablets of the reference product (simvastatin, 40 mg) first and after a 7-day washout interval then received two tablets of the test product (simvastatin, 40 mg), whereas subjects in sequence B were administered test product first and after the same washout interval, the reference product. The subjects were randomly assigned to either of the two groups (i.e. A and B, in the ratio of 1:1) and administered the test or reference product along with 240 mL water orally.
Blood samples were obtained from the antecubital vein of the forearm at the following time points: 0 (pre-dose), 0.33, 0.67, 1, 1.33, 1.67, 2, 2.5, 3, 3.5, 4, 5, 6, 8, 10, 12 and 24 hours after administration of investigational products. Blood samples were centrifuged at 1,800 g for 10 minutes at 4℃, the separated plasma transferred to Eppendorf tubes, and stored below -70℃ until the determination of simvastatin concentration.
Simvastatin concentrations in plasma were measured by a validated liquid chromatography-tandem mass spectrometry (LC-MS/MS) method. The internal standard, lovastatin 100 µg/mL, were used in calibration. For each plasma sample, 100 µL of internal standard was added to the 0.5 mL plasma and vortexed thoroughly for 10 seconds. The mixture was extracted with 3 mL of methyl-t-butyl ether. The ether mix was vortexed for 3 minutes and centrifuged at 4,000 rpm for 5 minutes. The ether layer (approximately 2.5 mL) was transferred to another tube and evaporated under a stream of nitrogen gas. Then 200 µL of acetonitrile:methanol:2 mM ammonium formate = 50:20:30 (v/v/v, pH=4.5) mixture was added to solubilize the residue, and 10 µL of this solution was injected into the LC-MS/MS system for analysis. Within the concentrations of 0.2 to 20.0 ng/mL, intra-day variation in precision (%CV, coefficient of variation) was ≤ 6.39% which was within 98.25% to 110.00 % in accuracy; inter-day variation in precision was ≤ 8.86% which was within 98.64% to 101.86% in accuracy.
A non-compartmental method using Phoenix® WinNonlin® software version 6.3 (Certara, St. Louis, MO, USA) was employed to calculate the pharmacokinetic parameters of simvastatin. The maximum observed concentration (Cmax) and the time to reach Cmax (Tmax) were determined. The area under the concentration-time curve from time zero to time of last quantifiable concentration (AUClast) was determined by the linear trapezoidal rule. The AUC from the last measurable time to infinity (AUCextra) was calculated as Clast/λz, (Clast: last measurable concentration, λz: elimination rate constant), and the AUC from time zero to infinity (AUCinf) was calculated as AUClast + AUCextra. The percentage of AUCextra (%) represented as 100×[(AUCinf - AUClast)/AUCinf]. The elimination rate constant (λz) was obtained as the slope of the linear regression of the log-transformed concentration versus time data in the terminal phase and the elimination half-life (t½) was calculated as ln 2/λz.
The pharmacokinetic parameters were statistically analyzed using SPSS® software version 21.0 (IBM® SPSS® Statistics for Windows, Armonk, NY). Log-transformed Cmax and AUClast were compared between the test and reference formulations by analysis of variance as a mixed model. It was explained by considering the sequence, treatment, and period as the fixed effects and the subjects nested within the sequence as a random effect. The 90% confidence intervals (CIs) of the geometric mean ratios of test/reference formulations for Cmax and AUClast were estimated to assess the bioequivalence of the two formulations. The products were considered bioequivalent if the 90% CIs for these parameters were within the range of 0.80-1.25.
A total of 34 subjects were recruited to the current study and one subject was dropped out due to consent withdrawal. Demographic information and pharmacokinetics were analyzed for 33 subjects who completed the study. Average age of subjects was 23.3 ± 2.6 (mean ± standard deviation) years, mean height was 174.8 ± 6.3 cm and average weight was 68.2 ± 9.2 kg.
Both formulations showed comparable concentration-time profiles as shown in Figure 1. Cmax of the reference and test formulations were 6.21 ± 3.70 µg/L and 5.56 ± 2.39 µg/L, respectively. AUClast of the reference and test formulations were 28.52 ± 17.33 µg·h/L and 29.10 ± 21.04 µg·h/L, respectively. Other calculated pharmacokinetic parameters are summarized in Table 1. Individual concentration-time profiles for each formulation were presented in Figure 2, and individual Cmax and AUClast were compared between the formulations in Figure 3.
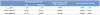
The values of the log-transformed Cmax and AUClast were compared between the reference and test formulations; the geometric mean ratios (90% CIs) of Cmax and AUClast were 0.9652 (0.8302–1.1223) and 0.9891 (0.8541–1.1455), respectively. The 90% CI values were within the range of 0.80 – 1.25 and were accordant with the bioequivalence criteria (Table 2).
Both the reference and test formulations were well tolerated with no serious adverse events reported; there were no clinically relevant findings in the evaluation of tolerability.
The Cmax and AUClast of simvastatin after a single oral administration of the reference and test formulations were comparable and both formulations of simvastatin were well tolerated in all subjects who completed the study.
Simvastatin is marketed as various formulations and in various strengths in Korea. While simvastatin is available as 10 mg to 40 mg tablets, a starting dose of 20 mg is recommended for patients with hypercholesterolemia, coronary vessel disease and who are at low risk of developing coronary events. Meanwhile, it was reported that a daily dose of simvastatin 40 mg efficiently reduced serum LDL by 41%, reduced serum triglyceride by 18%, and increased serum HDL by 12%.[4] Therefore, two tablets of simvastatin 20 mg (i.e. a total of 40 mg) were used to assess the bioequivalence of the two formulations in the current study.
Since simvastatin is a prodrug that is hydrolyzed to its active form, it is customary to measure the concentrations of simvastatin and its metabolite simvastatin β-hydroxyacid for bioequivalence studies.[56] However, in the current study, only simvastatin concentrations were measured and compared between the two formulations. The guidance outlined by the Ministry of Food and Drug Safety of Korea does not require the measurement and comparison of active metabolites, and the European Medicines Agency (EMA) guideline on the investigation of bioequivalence suggests that the assessment of bioequivalence for parent compound is recommended for inactive prodrugs.[7] Also, the U.S. FDA indicated in the Draft Guidance for Industry that for the bioequivalence studies, measurement of only the parent drug release from the dosage form is generally recommended and that the rationale for this recommendation is that the concentration-time profiles of the parent form is more sensitive to changes in formulation performance than the metabolites.[89]
Meanwhile, although these regulatory guidelines targeted on the bioequivalence of the parent drug, it is possible that the plasma concentrations of simvastatin are not proportionally related to the concentrations of active simvastatin β-hydroxyacid metabolites. However, according to a previous study that measured the AUC of simvastatin metabolites after oral administration of a radiolabeled dose of simvastatin, the AUC of active inhibitors (simvastatin metabolites) generally increased in linear correlation with increasing oral simvastatin doses over the range of 5 to 120 mg in healthy volunteers.[910] Also, another literature reported that the increment of simvastatin from 5 to 120 mg increases the pharmacological activity in a linear pattern.[9] Hence, the measurement of simvastatin concentration without measuring its active metabolite would not limit the bioequivalence evaluation.
In the current study, the mean values of t½ were reported to be 6.42 h (reference) and 5.97 h (test), which indicates that the pharmacokinetic sampling time of up to 24 hours post dose, approximately four times the half-life, was adequate in this study.
In previous studies, the inter-subject CVs were 52~53% for simvastatin Cmax and 48~76% for simvastatin AUC.[511] Considering these large inter-subject variabilities, the intra-subject CVs for Cmax and AUC were assumed to be approximately 30% in the current study. With this information, a sample size of 32 subjects was required to attain the 80% power at a 5% significance level, assuming a mean ratio (test/reference) of Cmax or AUC of 1 and a 30% intra-subject CV for Cmax or AUC. Therefore, a total of 34 subjects were deemed as an adequate sample size based on the dropout rate of 5%.[12]
Double peaks of the simvastatin concentration were reported in this study, which was consistent with the findings from other bioequivalence studies of simvastatin.[56] The individual plots (Fig. 2, 3) show that there are considerable individual variations in the plasma concentrations of simvastatin, and this may have resulted in the double peaks in the mean concentration-time profile in part.
In conclusion, the two formulations of the simvastatin 20 mg tablets exhibited comparable pharmacokinetic profiles and the 90% CIs were within the acceptable range of bioequivalence criteria. These two formulations, therefore, are expected to be administered to patients interchangeably without pharmacokinetic or tolerability concerns.
Figures and Tables
 | Figure 1Mean plasma simvastatin concentration versus time profile of the reference and test formulations after a single oral administration of simvastatin 40 mg (20 mg × 2 tablets) in linear (left) and semi-logarithmic (right) scale. |
 | Figure 2Individual plasma simvastatin concentration versus time profile of the reference (upper) and test formulations (lower) after a single oral administration in linear scale. |
 | Figure 3Comparison of the individual Cmax (upper) and AUClast (lower) between the reference and test formulations after a single oral administration. |
Table 1
Pharmacokinetic parameters of simvastatin 40 mg (20 mg tablet × 2 tablets) after a single oral administration of the reference and test formulations
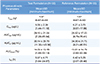
All values are expressed as mean ± standard deviation, except of Tmax values expressed as median (minimum-maximum). Tmax, time to reach Cmax; Cmax, peak plasma concentration of simvastatin; AUClast, area under the plasma concentration-time curve from time zero to last measurable time; AUCinf, AUC from time zero to infinity; AUCextra (%), percentage of AUC from the last measurable time to infinity; t½, elimination half-life.
Table 2
Comparison of Cmax, AUClast and AUCinf of simvastatin after a single oral administration of the 2 reference tablets and 2 test tablets
References
1. Plosker GL, McTavish D. Simvastatin. A reappraisal of its pharmacology and therapeutic efficacy in hypercholesterolaemia. Drugs. 1995; 50:334–363.
2. Vickers S, Duncan CA, Chen IW, Rosegay A, Duggan DE. Metabolic disposition studies on simvastatin, a cholesterol-lowering prodrug. Drug Metab Dispos. 1990; 18:138–145.
3. Mauro VF, MacDonald JL. Simvastatin: a review of its pharmacology and clinical use. DICP. 1991; 25:257–264.

4. Schachter M. Chemical, pharmacokinetic and pharmacodynamic properties of statins: an update. Fundam Clin Pharmacol. 2005; 19:117–125.

5. Najib NM, Idkaidek N, Adel A, Admour I, Astigarraga RE, Nucci GD, et al. Pharmacokinetics and bioequivalence evaluation of two simvastatin 40 mg tablets (Simvast and Zocor) in healthy human volunteers. Biopharm Drug Dispos. 2003; 24:183–189.

6. Tseng CM, Huang CC, Ho MC, Chen YA, Shieh YH, Chen IK. Bioequivalence assessment of two simvastatin tablets in healthy Taiwanese volunteers. J Food Drug Anal. 2007; 15:15–19.

7. Guideline on the Investigation of Bioequivalence. Novermber 1 2016. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500003011.
8. FDA Guidance for Industry: Bioavailability and Bioequivalence Studies for Orally Administered Drug Products - General Considerations. CDER/FDA: Washington;2003. 03. Novermber 1 2016. http://www.fda.gov/ohrms/dockets/ac/03/briefing/3995B1_07_GFI-BioAvail-BioEquiv.pdf.
9. Midha KK, Rawson MJ, Hubbard JW. The role of metabolites in bioequivalence. Pharm Res. 2004; 21:1331–1344.

10. Mauro VF. Clinical pharmacokinetics and practical applications of simvastatin. Clin Pharmacokinet. 1993; 24:195–202.

11. Yun H, Kang W, Kwon K. Evaluation of the bioequivalence of simvastatin 20 mg tablets in healthy volunteers. Korean J Clin Pharm. 2005; 15:41–45.
12. Chow SC, Wang H. On sample size calculation in bioequivalence trials. J Pharmacokinet Pharmacodyn. 2001; 28:155–169.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download