INTRODUCTION
The Korean National Health Insurance (KNHI) system has offered health care coverage to the entire population since 1989, providing coverage for inpatient and outpatient services, prescription drugs, and dental care [
1]; nonetheless, many essential dental services, such as preventive care, dental examinations, orthodontics, and restorative treatment (e.g., dental prosthetics and implants) are excluded. The rate of KNHI coverage for dental health is around 30%–35%, and the low coverage provided by the KNHI is a major barrier affecting access to dental care that may lead individuals to make large out-of-pocket payments for uncovered services [
23].
Periodontitis is an inflammatory chronic disease in which periodontal tissue is destroyed due to dental plaque that forms on the tooth surface and the reaction of the host to the plaque. The inflammatory response elicited by the biofilm leads to gingival bleeding, pocket formation, and attachment and bone loss, and may require the extraction of permanent teeth [
45]. According to the National Health and Nutrition Examination Survey, the prevalence of severe periodontitis was 27.7% among adults aged over 19 years in 2013 [
6]. In addition, gingivitis and periodontal diseases have ranked among the top 10 diseases in terms of coverage for outpatient care over the years. Although regular dental checkups, scaling, and consistent supportive periodontal therapy even after undergoing periodontal treatment have been strongly emphasized as measures to decrease the incidence of tooth loss and periodontal disease, many Koreans who require dental scaling or preventive dental care are not receiving sufficient care [
7]. In particular, people with low socioeconomic status, as defined by income, level of education, and/or residential area, have been found to have more prevalent and more severe periodontal disease [
58910].
As a result of these conditions, growing interest in improving access to care and periodontal health outcomes has recently emerged. In July 2013, the Korean government extended dental care benefits under the KNHI to cover preventive scaling (once-yearly plaque and calculus removal) for adults ages 20 and older, which presented an important opportunity to reduce the barriers to access to dental care for all adults, irrespective of socioeconomic background and/or residential location. Copayments were reduced to lower the financial barriers impeding access to periodontal care.
The above political decision utilized the KNHI system to increase access to dental services by substantially lowering cost sharing at the point of service. This policy was expected to stimulate adults' access to and use of preventive care by expanding public health insurance.
Economic theory suggests that demand increases when health insurance reduces the relative cost of health care [
1112]. Studies have analyzed the impacts of social health insurance in the US and reported that expanding the coverage of dental benefits reduced dental unmet needs and increased utilization of dental services. For instance, the Massachusetts health care reform expanded comprehensive dental benefits for adults with incomes at or below 100% of the poverty line. Long and Stockley [
13] evaluated the impact of the health reform in Massachusetts by estimating dental care use in the state's nonelderly population. According to this analysis, the proportion of Massachusetts adults reporting that they were not able to obtain necessary dental care due to financial reasons declined, and the use of dental services increased after the health reform in comparison with the control population in other states. Additionally, in studies of low-income children, those who had State Children's Health Insurance Program (SCHIP) or Medicaid coverage were less likely to report experiencing access difficulties for dental care and more likely to have visited a dentist within 6 or 12 months compared with their uninsured counterparts. These results indicated that public dental care delivery systems such as SCHIP or Medicaid improved low-income children's access to dental care [
141516].
Given this empirical evidence, we hypothesized that Korea's recent policy of expanding dental benefit coverage to include scaling would lead to individuals experiencing fewer financial difficulties in accessing dental care, allowing them to use more dental services. However, to our knowledge, no research to date has explored this question, especially at the national level.
In light of the above considerations, the aim of this paper was to explore how the implementation of this policy affected unmet dental care needs and dental care utilization among adults at the national level. This is the first population-based investigation of this issue. The results of this study may yield further insight into solving problems related to the accessibility of dental care under the KNHI system.
MATERIALS AND METHODS
Data source and study population
The Korea National Health and Nutrition Examination Survey (KNHANES) was used for this study. The KNHANES, which has a cross-sectional design and is conducted by the Korea Centers for Disease Control and Prevention and the Korean Ministry of Health, has continuously collected a variety of health-related information, including health status, access to health services, and use of health services, from nationally representative samples of the Korean civilian non-institutionalized population aged 1 year or older since 1998.
This study included KNHANES data from the KNHANES V (2010, 2012) and the KNHANES VI (2014). KNHANES V (2011) and KNHANES VI (2013) were excluded due to the absence of oral examination information and dental coverage policy for scaling being implemented in the middle of the year, respectively. Thus, we obtained pre-policy information from the 2010 and 2012 waves of the KNHANES V and post-policy information from the 2014 wave of the KNHANES VI.
Our sample (n=24,566) was restricted to adults aged 20–64 years. Adults who were over 65 years old (n=10,739) were excluded as we expected the effect of the policy implementation to be greatest for non-elderly adults. We excluded 406 adults receiving Medical Aid Program and 103 pregnant women. Observations (n=524) with incomplete data for survey weight in both the health interview and the health examination used in this study were excluded. The sample used for the final analysis consisted of 12,794 study subjects with health insurance under the KNHI.
Definitions of variables
We generated 2 binary outcomes measuring access to dental care, assessing whether adults had unmet dental care needs and/or visited a dentist for preventive care in the past year.
The self-reporting of unmet dental care needs identified adults who needed but did not receive dental care (yes/no), as a measure of overall barriers to accessing dental care [
17]. The dental visit measure was a self-reported measure of whether each respondent had at least 1 visit for preventive care, including scaling, sealant, and fluoride varnish (yes/no), as a measure of preventive dental care utilization.
The independent variable of primary interest in the analysis was a dummy variable for the policy change. It operationalized a division between 2 time frames relative to the policy implementation: pre-policy (2010, 2012) and post-policy (2014). Additional covariates were included based on the theoretical framework proposed by Andersen and Davidson in 1997 [
18], detailing a multiple-pronged approach to understanding dental service utilization. Therein the authors presented a causal ordering of dental care utilization within an integrated framework. The framework guiding this study posits that the probability of dental service use is influenced by a multitude of factors relating to a predisposition to use services (for example, age, sex, education, and marital status); factors that support or impede use (for example, income, type of health insurance, and distance to care); factors affecting individuals' need for health care (measurable values concerning health and illnesses); and factors relating to cognition (for example, dental knowledge and opinions) and expectations (for example, rewards and costs). Based on this framework, this study considered covariates such as gender, age, household income, education level, residence area, geographical accessibility (density of dental practitioners per 100,000 population), chewing difficulty, smoking, and the presence of a periodontal pocket (defined as a community periodontal index [
19] greater than or equal to code 3; ≥4 mm).
Statistical analysis
Our analysis of the study sample incorporated sampling weights to obtain nationally representative estimations. The results were adjusted to account for the KNHANES complex sample survey design involving stratified multistage sampling, including primary sampling units (PSU), strata (Kstrata), and the sample weights that were provided.
The distribution of characteristics in the study participants was analyzed according to age group, gender, household income, and education level in the pre-policy (2010, 2012) and post-policy (2014) period data. We compared access to dental care before and after policy implementation as measured in terms of unmet dental care needs and preventive dental care utilization rates over the study period, using the χ2 test for a complex sample.
The overall effect of policy implementation was estimated while controlling for a wide range of covariates. We acknowledge that it would have been ideal to measure the change in dental care access as a result of policy implementation. In general, when the dependent variable is a binary variable, the error term violates the assumptions of homogeneity and the normal distribution; therefore, estimates were based on the probit model, which has the same probability distributions of error terms and hypothesizes a normal distribution with a covariance of zero [
20]. Since the coefficient estimated from the probit model is difficult to analyze directly, the marginal effect was calculated. The marginal effect of the probit model is the same as the sign of β
, but because it differs by a value of
x, the estimation of the marginal effect also changes [
20]. In this study, the marginal effect was calculated when the value changed from 0 to 1 for the independent variable, which was a dummy variable.
We also conducted a subgroup analysis, which allowed us to estimate models to identify the extent to which the policy affected individuals depending on their household income and education level. Income was defined as the average monthly household income adjusted for the number of family members in the household (household income divided by number of family members) and categorized in terms of household income quartiles (low, lower-middle, upper-middle, and upper). We generated 2 income groups: a low-income group, including the low and lower-middle quartiles, and a high-income group, including the upper-middle and upper quartiles.
The participants were classified by education according to the level of school they had graduated from (elementary school graduation or less, middle school graduation, high school graduation, and college graduation or above). Education was dichotomized into a low-education group (including elementary school graduation or less and middle school) and a high-education group (including high school graduation and college graduation or above). This study was granted an exemption by the Institutional Review Board of Korea University, Korea.
All statistical tests were conducted using STATA version 13 (Stata Corp., College Station, TX, USA). Statistical significance was set at the 5% level.
DISCUSSION
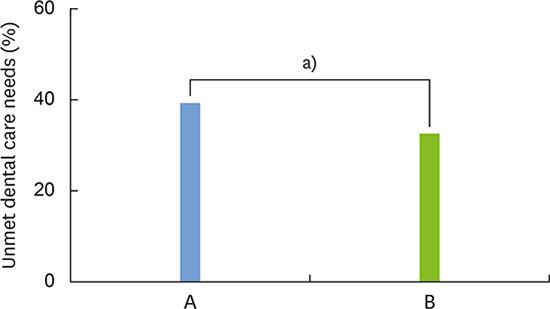
In the present study, the effect of expanding the accessibility of dental care was analyzed in order to investigate whether the scaling coverage expansion met its objective of improving access to dental care utilization, and whether the results corresponded to the purpose of the policy.
After the policy took effect, the prevalence of unmet dental care needs decreased by almost 6.1%, and the likelihood of preventive dental care utilization in the past year increased by 14.0%. These results correspond to the studies [
1416] of the newly introduced SCHIP program in which the dental care use rate of children from low-income families increased and the likelihood of unmet dental care largely decreased; in those studies, insurance enrollees had a higher utilization rate of dental care service, and their unmet dental needs fell compared to those who did not have coverage. In addition, an empirical study [
21] that examined the effect of coverage expansion for dental care as part of health care policy aimed at low-income individuals suggested a consistent conclusion. The study estimated that if a state provided adults dental coverage under Medicaid, the probability of its enrollees having an annual dental visit was 16%–22% greater than that of enrollees in states that do not provide dental coverage.
Our subgroup analysis that examined the effect of the policy by stratifying according to income level revealed that a significant effect for unmet needs for dental care and preventive dental visits was observed only in the high-income group, thus suggesting that the policy effect was limited only to high-income households. This contradicts the results reported by Chen et al. [
22], Wagstaff [
23], and Giedion et al. [
24], who found that coverage expansion aimed at reducing individuals' medical expenses was more effective for the poor. In general, it has been recognized since the 1960s that low-income individuals have more missing teeth with a higher prevalence and severity of periodontal diseases [
11]. Epidemiological studies have suggested that income is associated with disparities in preventive dental care and regular checkup rates, and that low-income individuals are more likely to visit providers for emergency or temporary care than their higher-income counterparts [
5825]. A study by Lee et al. [
7] concluded that more people need periodontal scaling among those with lower levels of income in Korea. Based on current evidence, the high prevalence of periodontitis in the low-income group is a predictable phenomenon. Therefore, it is necessary to examine more carefully why the effect of the policy was greater in the high-income group in this study. Further investigation is required to uncover the reasons why access to preventive dental care among the low-income group did not significantly change after the introduction of the policy.
The tendency for the effects of the policy to be manifested only in the high-income group can be understood in the same way that the results of the analysis according to education level are. The likelihood of visiting a dentist for preventive care including simple dental scaling, sealant, and fluoride varnish increased by 9.6% in the low education group, and by 18.3% in the high education group. The rate of using preventive dental care doubled in the higher-education group compared to that in the lower-education group. Moreover, unmet dental care decreased after the coverage expansion only in the high-education group. The subjects in this study were limited to adults between 20 and 64 years of age, and the proportion of people who had completed a high school or college-level education was high. The range of subjects for analysis was limited to those enrolled in the KNHI. However, the effect of the scaling coverage expansion policy still showed a significant gap based on education levels, which has significant implications for further policy development.
Although various studies have documented that expansions in services included in public health insurance certainly facilitate the use of dental care services [
141621], dental visits for preventive services may still vary depending on individual characteristics or the knowledge level of individuals. Enabling factors such as income can affect the use of available, cost-effective preventive dental care services, but so can the knowledge level of patients and other factors [
18]. Thus, the effect of any such policy can vary depending on individuals' income and education levels. In particular, the acquisition of information and technology skills through education has a strong influence on the perceptive capacity of individuals [
2627], which is related to their use of medical services. Therefore, even if health insurance coverage expands to include dental scaling, individuals with less education may lack the requisite knowledge about prevention and the management of periodontal care to choose to use such services, or may not be able to recognize the need for such services. As a result, the rate of accessing dental care may demonstrate a gap in this population segment. Thus, even if the needs for treatment, maintenance, and management of oral disease are high, the policy effect may be relatively small in those individuals due to their lack of prior knowledge about the implementation of the policy or of available channels for acquiring such information.
The study has the following limitations: First, the data used from the KNHANES did not completely offset the measurement errors that arose from the differences in the measurements taken each year, even though it is preferable to use stable data in which such measurement errors are minimized.
Second, our ability to estimate the cause-and-effect relationship between the policy change and the outcomes was limited, and the 2 compared populations were not the same. Change over the course of time, which would be irrelevant for understanding the effect of the policy, was not controlled, and no fundamental solution was suggested for the endogeneity problem. Thus, it would be necessary to conduct a follow-up policy effect study based on a quasi-experimental design, such as difference-in-difference methodology or an interrupted time-series analysis.
Finally, this study did not consider whether the dental health insurance coverage expansion improved health outcomes. Therefore, a policy evaluation study is required in the future in order to investigate whether the prevalence of periodontal diseases decreased—in other words, if the governmental policy objectives were met based on an empirical evaluation of the policy and its longer-term health effects.
In conclusion, the coverage expansion for scaling demonstrated to have a significant association with decreasing unmet dental care needs and increasing dental care utilization. However, as shown in this study, the effect of the policy was greater in individuals with higher levels of income or education. That is, the policy benefited only some groups, in contrast with the policy objective of benefiting all participants in the KNHI system. In future policy design and implementation, it is necessary to develop a policy that addresses factors affecting the rate of access to dental care service while expanding dental care coverage to relieve the associated financial burden of care.










 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download