1. Valenti M, Valenti A. Retrospective survival analysis of 261 lithium disilicate crowns in a private general practice. Quintessence Int. 2009; 40:573–579.
2. Gehrt M, Wolfart S, Rafai N, Reich S, Edelhoff D. Clinical results of lithium-disilicate crowns after up to 9 years of service. Clin Oral Investig. 2013; 17:275–284.

3. Herrguth M, Wichmann M, Reich S. The aesthetics of all-ceramic veneered and monolithic CAD/CAM crowns. J Oral Rehabil. 2005; 32:747–752.

4. Bengazi F, Wennström JL, Lekholm U. Recession of the soft tissue margin at oral implants. A 2-year longitudinal prospective study. Clin Oral Implants Res. 1996; 7:303–310.

5. Bressan E, Paniz G, Lops D, Corazza B, Romeo E, Favero G. Influence of abutment material on the gingival color of implant-supported all-ceramic restorations: a prospective multicenter study. Clin Oral Implants Res. 2011; 22:631–637.

6. Ekfeldt A, Fürst B, Carlsson GE. Zirconia abutments for single-tooth implant restorations: a retrospective and clinical follow-up study. Clin Oral Implants Res. 2011; 22:1308–1314.

7. Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005; 25:113–119.
8. Guess PC, Zavanelli RA, Silva NR, Bonfante EA, Coelho PG, Thompson VP. Monolithic CAD/CAM lithium disilicate versus veneered Y-TZP crowns: comparison of failure modes and reliability after fatigue. Int J Prosthodont. 2010; 23:434–442.
9. Van Dooren E, Calamita M, Calgaro M, Coachman C, Ferencz JL, Pinho C, et al. Mechanical, biological and clinical aspects of zirconia implants. Eur J Esthet Dent. 2012; 7:396–417.
10. Wittneben JG, Wright RF, Weber HP, Gallucci GO. A systematic review of the clinical performance of CAD/CAM single-tooth restorations. Int J Prosthodont. 2009; 22:466–471.
11. Grundke K, Bogumil T, Werner C, Janke A, Pöschel K, Jacobasch HJ. Liquid-fluid contact angle measurements on hydrophilic cellulosic materials. Colloids Surf A Physicochem Eng Asp. 1996; 116:79–91.

12. de Groot P, Deck L. Surface profiling by frequency-domain analysis of white light interferograms. Proc SPIE. 1994; 2248:101–104.
13. Rajaraman R, Rounds DE, Yen SP, Rembaum A. A scanning electron microscope study of cell adhesion and spreading
in vitro
. Exp Cell Res. 1974; 88:327–339.

14. Duval JL, Letort M, Sigot-Luizard MF. Comparative assessment of cell/substratum static adhesion using an
in vitro organ culture method and computerized analysis system. Biomaterials. 1988; 9:155–161.

15. Sigot-Luizard MF, Lanfranchi M, Duval JL, Benslimane S, Sigot M, Guidoin RG, et al. The cytocompatibility of compound polyester-protein surfaces using an
in vitro technique. In Vitro Cell Dev Biol. 1986; 22:234–240.

16. Abramoff MD, Magalhães PJ, Ram SJ. Image processing with ImageJ. Biophotonics Int. 2004; 11:36–42.
17. Josset Y. Oum’Hamed Z, Zarrinpour A, Lorenzato M, Adnet JJ, Laurent-Maquin D.
In vitro reactions of human osteoblasts in culture with zirconia and alumina ceramics. J Biomed Mater Res. 1999; 47:481–493.

18. Covacci V, Bruzzese N, Maccauro G, Andreassi C, Ricci GA, Piconi C, et al.
In vitro evaluation of the mutagenic and carcinogenic power of high purity zirconia ceramic. Biomaterials. 1999; 20:371–376.

19. Warashina H, Sakano S, Kitamura S, Yamauchi KI, Yamaguchi J, Ishiguro N, et al. Biological reaction to alumina, zirconia, titanium and polyethylene particles implanted onto murine calvaria. Biomaterials. 2003; 24:3655–3661.

20. van Brakel R, Meijer GJ, Verhoeven JW, Jansen J, de Putter C, Cune MS. Soft tissue response to zirconia and titanium implant abutments: an
in vivo within-subject comparison. J Clin Periodontol. 2012; 39:995–1001.

21. De Sanctis M, Baldini N, Vignoletti F. Soft tissue management around teeth and implants. J Parodontol Implantol Oral. 2010; 29:245–269.
22. Rimondini L, Cerroni L, Carrassi A, Torricelli P. Bacterial colonization of zirconia ceramic surfaces: an in vitro and in vivo study. Int J Oral Maxillofac Implants. 2002; 17:793–798.
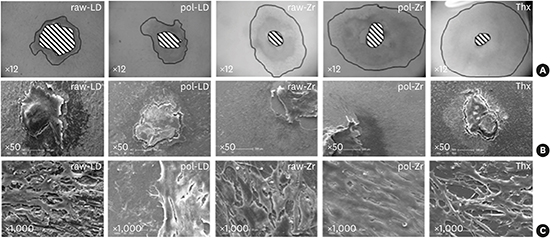
23. Brunot-Gohin C, Duval JL, Azogui EE, Jannetta R, Pezron I, Laurent-Maquin D, et al. Soft tissue adhesion of polished versus glazed lithium disilicate ceramic for dental applications. Dent Mater. 2013; 29:e205–12.

24. Müller C, Lüders A, Hoth-Hannig W, Hannig M, Ziegler C. Initial bioadhesion on dental materials as a function of contact time, pH, surface wettability, and isoelectric point. Langmuir. 2010; 26:4136–4141.

25. Bolortuya G, Ebihara A, Ichinose S, Watanabe S, Anjo T, Kokuzawa C, et al. Effects of dentin surface modifications treated with Er:YAG and Nd:YAG laser irradiation on fibroblast cell adhesion. Photomed Laser Surg. 2012; 30:63–70.

26. Duval JL, Dinis T, Vidal G, Vigneron P, Kaplan DL, Egles C. Organotypic culture to assess cell adhesion, growth and alignment of different organs on silk fibroin. J Tissue Eng Regen Med. Forthcoming. 2014.

27. Messer RL, Lockwood PE, Wataha JC, Lewis JB, Norris S, Bouillaguet S.
In vitro cytotoxicity of traditional versus contemporary dental ceramics. J Prosthet Dent. 2003; 90:452–458.

28. Brackett MG, Lockwood PE, Messer RL, Lewis JB, Bouillaguet S, Wataha JC.
In vitro cytotoxic response to lithium disilicate dental ceramics. Dent Mater. 2008; 24:450–456.
29. Scarano A, Piattelli M, Caputi S, Favero GA, Piattelli A. Bacterial adhesion on commercially pure titanium and zirconium oxide disks: an
in vivo human study. J Periodontol. 2004; 75:292–296.

30. Rompen E, Raepsaet N, Domken O, Touati B, Van Dooren E. Soft tissue stability at the facial aspect of gingivally converging abutments in the esthetic zone: a pilot clinical study. J Prosthet Dent. 2007; 97:S119–25.









 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download