1. Grunder U. The inlay-graft technique to create papillae between implants. J Esthet Dent. 1997; 9:165–168.

2. Choquet V, Hermans M, Adriaenssens P, Daelemans P, Tarnow DP, Malevez C. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001; 72:1364–1371.

3. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000; 71:546–549.

4. Tarnow DP, Eskow RN. Considerations for single-unit esthetic implant restorations. Compend Contin Educ Dent. 1995; 16:778–784.
5. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992; 63:995–996.

6. Cho HS, Jang HS, Kim DK, Park JC, Kim HJ, Choi SH, et al. The effects of interproximal distance between roots on the existence of interdental papillae according to the distance from the contact point to the alveolar crest. J Periodontol. 2006; 77:1651–1657.

7. Chen MC, Liao YF, Chan CP, Ku YC, Pan WL, Tu YK. Factors influencing the presence of interproximal dental papillae between maxillary anterior teeth. J Periodontol. 2010; 81:318–324.

8. Kim JH, Cho YJ, Lee JY, Kim SJ, Choi JI. An analysis on the factors responsible for relative position of interproximal papilla in healthy subjects. J Periodontal Implant Sci. 2013; 43:160–167.

9. Chang LC. The association between embrasure morphology and central papilla recession. J Clin Periodontol. 2007; 34:432–436.

10. Chang LC. Assessment of parameters affecting the presence of the central papilla using a non-invasive radiographic method. J Periodontol. 2008; 79:603–609.

11. Beagle JR. Surgical reconstruction of the interdental papilla: case report. Int J Periodontics Restorative Dent. 1992; 12:145–151.
12. Jemt T. Regeneration of gingival papillae after single-implant treatment. Int J Periodontics Restorative Dent. 1997; 17:326–333.
13. Nemcovsky CE. Interproximal papilla augmentation procedure: a novel surgical approach and clinical evaluation of 10 consecutive procedures. Int J Periodontics Restorative Dent. 2001; 21:553–559.
14. Lee EK, Herr Y, Kwon YH, Shin SI, Lee DY, Chung JH. I-shaped incisions for papilla reconstruction in second stage implant surgery. J Periodontal Implant Sci. 2010; 40:139–143.

15. Nemcovsky CE, Moses O, Artzi Z. Interproximal papillae reconstruction in maxillary implants. J Periodontol. 2000; 71:308–314.

16. Becker W, Gabitov I, Stepanov M, Kois J, Smidt A, Becker BE. Minimally invasive treatment for papillae deficiencies in the esthetic zone: a pilot study. Clin Implant Dent Relat Res. 2010; 12:1–8.

17. Necas J, Bartosikova L, Brauner P, Kolar J. Hyaluronic acid (hyaluronan): a review. Vet Med (Praha). 2008; 53:397–411.

18. Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964; 22:121–135.

19. Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963; 21:533–551.

20. Mansouri SS, Ghasemi M, Salmani Z, Shams N. Clinical application of hyaluronic acid gel for reconstruction of interdental papilla at the esthetic zone. J Islam Dent Assoc Iran. 2013; 25:152–157.





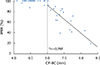
 , Black triangle area (mm2);
, Black triangle area (mm2);  , Black triangle height (mm);
, Black triangle height (mm);  , Black triangle width (mm).
, Black triangle width (mm).





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download