INTRODUCTION
Lack of interdental papilla, which can arise from many causes, creates esthetic problems that concern clinicians and patients alike. The degree of interdental papilla fill is influenced by various embrasure dimensions such as the vertical distance between the contact point position and the bone crest, the horizontal interdental distance, and the facio-lingual thickness of the papilla base [
12]. In the presence of the diastema between teeth, the interdental papilla may be absent, since no contact point exists. Hence, it has been suggested that a new contact point can be created between two adjacent teeth by orthodontic approximation with bodily movement [
34]. Lowering the contact point position by “stripping” off the proximal surfaces of the adjacent teeth has also been favored to improve papilla fill after closure of the diastema [
5]. Furthermore, it has been claimed that the papilla height level could move coronally by creeping of the proximal gingiva as well as by squeezing the gingival volume in the proximal embrasure space during orthodontic closure of the diastema [
346]. With respect to the direction of orthodontic movements, it has been suggested that the palatal movement and intrusive movement of the teeth could increase the height of interdental papilla [
7]. In fact, orthodontic approximation of maxillary incisors with an interproximal gap due to pathologic tooth movement was found to significantly enhance the level of the interdental papilla, as well as the interproximal bone level [
8]. In contrast, the height of interdental papilla decreased after orthodontic closure of the diastema [
7]. Hence, it is not clear whether the papilla height was increased or not by orthodontic approximation of teeth with diastemas.
Facio-lingual thickness of the papilla has been suggested to play an important role in supporting the papilla height level [
9]. In addition, the probability of a complete papilla fill was significantly affected by the facio-lingual dimension of the papilla base [
2]. However, information regarding the alteration of the facio-lingual dimensions of the papilla base during orthodontic closure of the diastema is not available in the literature.
The aim of this study was to evaluate alterations of papilla dimensions after orthodontic closure of the diastema between maxillary central incisors.
MATERIALS AND METHODS
Subject sample
Subjects for this study were consecutively selected from the pool of patients who had been treated during the period between January 1994 and May 2014 at the Department of Orthodontics, Chonbuk National University Dental Hospital, Jeonju, South Korea. For inclusion in the study, the subject should have (i) a visible diastema between the maxillary central incisors that was closed by orthodontic approximation, (ii) no clinically visible gingival inflammation and periodontal bone loss at the maxillary central incisors, (iii) no medication history related to gingival enlargement, (iv) no apparent extrusion and/or severe buccal tipping of the maxillary central incisors, and (v) study models and clinical photographs taken before the initiation of orthodontic treatment and at the follow-up examinations after completion of orthodontic closure of the diastema. Maxillary central incisors were mainly subjected to orthodontic bodily movement so that the diastema between the teeth could be closed. To retain stability of the moved teeth and to prevent a relapse of tooth movement afterwards, the teeth were passively splinted with a 0.7 mm twist flex wire (Remanium® wire, Dentaurum, Ispringen, Germany).
Approval of the original study protocol was obtained from the Ethics Committee at the Chonbuk National University Hospital (IRB #CUH 2015-09-017-001). The study was performed in accordance with the 1975 Declaration of Helsinki, which was revised in 2013.
Photographic assessments
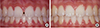
Photographs focusing on the proximal embrasure between maxillary central incisors were taken before the orthodontic treatment and at the follow-up examination (
Figure 1A and B). The following variables were assessed on the digitized images with the use of the measuring tool available in a software program (Photoshop CS6, Adobe, USA). The ratio between the clinical crown height in the photograph and that in the study model was calculated, and it was used for calibration of the linear measurements in the individual photograph [
210] (
Figure 2A).
Figure 1
Clinical photographs of a 13-year-old female patient. (A) Before orthodontic closure of the diastema between maxillary central incisors; (B) At the follow-up examination after closure of the diastema.
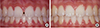
Figure 2
Photographic (A) and study model assessments (B and C). CCH, clinical crown height; PH, papilla height; REF, reference line; PBW, papilla base width; CCW, clinical crown width; DW, diastema width; PBT, papilla base thickness.

• Clinical crown height (CCH): the distance between the most apical gingival margin and the incisal edge of the crown of the right maxillary central incisor measured to the nearest 0.1 mm.
• Papilla height (PH): the distance from the top of the papilla between maxillary central incisors to a line connecting the most apical level of the gingival margin of the two teeth, measured to the nearest 0.1 mm [
11].
Further, the degree of
papilla fill between central incisors was determined at the follow-up examinations using the scoring system of the Papilla Index [
12].
Study model assessments
The following variables were measured to the nearest 0.1 mm on diagnostic casts obtained before orthodontic treatment and at follow-up examinations with the use of calipers (Digimatic caliper, Mitutoyo Corporation, Kawasaki, Japan; Iwanson Spring Caliper, Hu-Friedy Chicago, Chicago, IL, USA) (
Figure 2B and C).
• Clinical crown height (CCH): the distance between the most apical gingival margin and the incisal edge of the crown of the right maxillary central incisor measured to the nearest 0.1 mm.
• Clinical crown width (CCW): the widest mesio-distal dimension of the crown of the right maxillary central incisor measured to the nearest 0.1 mm.
• Papilla base thickness (PBT): measured as the distance between the facial and lingual mid-point of lines connecting the facial/lingual levels of the most apical gingival margins at the maxillary central incisors.
• Papilla base width (PBW): measured as the length of a line connecting the most apical level of gingival margins at the maxillary central incisors.
• Diastema width (DW): the length of the horizontal gap between maxillary central incisors measured by the number of Tofflemire matrix bands with a thickness of 38 μm (Water Pik Inc., Fort Collins, CO, USA) that could be inserted into the diastema.
One calibrated examiner (JJ), who had been trained in calibration and was not involved in the treatment of the patients, performed all assessments included in the study.
Error in the methods
The validity of the assessments was examined by a comparison of CCH assessments in 15 patients, measured on photographs and on diagnostic casts. The mean difference between the two measurements was 0.02 mm (SD 0.12). In 87% of the paired assessments (13/15), the difference was less than 0.1 mm.
Intra-examiner reproducibility of photographic and study model assessments was determined by repeated measurements in 15 randomly selected patients with a 2-week interval. Intraclass correlation coefficients calculated for consistency and absolute agreement of a single rater were well over 0.9 for all the tested variables. The mean difference was 0.01 mm (SD 0.10) for CCH, 0.05 mm (SD 0.06) for CCW, 0.02 mm (SD 0.03) for DW, and 0.04 mm (SD 0.13) for PBT measured on the study models, and 0.07 mm (SD 0.15) for PH measured on the photographs.
Data analysis
Hypotheses to be tested in this study were as follows: (1) “Do PH and PBT increase or decrease after orthodontic closure of the diastema?”, (2) “Do relationships exist between various papilla dimensions before the orthodontic treatment and those at the follow-up examinations after closure of the diastema?”, and (3) “Do the PH, PBT, and PBW before orthodontic treatment influence the alterations of PH and PBT?”.
The primary outcome of the study was the alteration of PH and PBT after orthodontic closure of the diastema. Mean values, standard deviations, ranges, 95% confidence intervals, and the distributions of the variables were calculated for data description with the subject as a statistical unit. Correlations between the papilla dimensions before orthodontic treatment and those at the follow-up examinations were analyzed. Data analyses were performed with the use of a statistical software program (SPSS 22, IBM Corp., Armonk, NY, USA). Alterations of the PH and PBT after orthodontic closure of the diastema were analyzed with a paired t-test after testing normality of the data with the Kolmogorov-Smirnov test. The influence of age, sex, follow-up period, CCW/CCH ratio, PH, DW, and PBT before orthodontic treatment on the alterations of the PH and PBT after closure of the diastema was analyzed with univariate regression analysis. To analyze the potential influences of 3-dimensional papilla dimensions before orthodontic treatment on the alterations of PH and PBT, a multiple regression model was formulated including the PH, PBT, and PBW before the orthodontic treatment as predictor variables. A P-value <0.05 was considered to be statistically significant in all analyses.
RESULTS
Sixty patients (36 females/24 males) were consecutively selected for this study. The mean age was 19 years (range, 10–46 years), and the average follow-up period was 28 months (range, 6–209 months) (
Table 1).
Table 1
Description of the patient samples
|
Variable |
Outcome assessment |
|
No. of patients |
60 |
|
Mean age (range:yr) |
19 (10-46) |
|
Sex ratio (male/female) |
24/36 |
|
Mean follow-up (range:mon) |
28 (6-209) |
|
Mean diastema width before orthodontic treatment (range:mm) |
1.1 (0.3-3.0) |
PH decreased by 0.80 mm and PBT increased after orthodontic closure of the diastema (
P<0.01). However, CCH assessed on the study models did not change (
P=0.32) (
Table 2). In terms of frequency, PH was decreased in 82% of the patients (49/60), and PBT was increased in 85% of the patients (47/55) after closure of the diastema. Five sites with an artifact in the study model were excluded from PBT assessment on the study models. On photographic assessment, all 60 proximal sites (100%) were judged as having a “complete” papilla fill (Papilla Index Score 3) at the follow-up examinations [
12].
Table 2
Alterations of the papilla height, clinical crown height, and papilla base thickness after orthodontic closure of the diastema

|
Variable |
Before orthodontic treatment |
At follow-up examination |
Difference |
95 % confidence interval |
P-value |
|
Photographic assessment |
|
|
|
|
|
|
Papilla height |
5.52±0.86 |
4.71±0.93 |
-0.80±0.84 |
-1.03/-0.58 |
0.000 |
|
Study model assessment |
|
|
|
|
|
|
Clinical crown height |
9.85±0.84 |
9.89±0.85 |
0.04±0.29 |
-0.04/0.11 |
0.320 |
|
Papilla base thickness |
8.38±0.67 |
8.91±0.60 |
0.52±0.56 |
0.36/0.67 |
0.001 |
The correlation analysis between the papilla dimensions before orthodontic treatment and those at follow-up examinations revealed that the PH and PBT before the orthodontic treatment were significantly correlated (Pearson’s
r=0.534,
P<0.001). In univariate regression analysis, the PH (
P=0.002) and PBT (
P=0.047), among independent variables—that is, age, sex, follow-up period, CCW/CCH ratio, and the PH, PBT, DW dimensions before the orthodontic treatment—significantly influenced the alteration of PH (
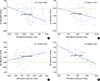
Figure 3A and B).
Figure 3
Relationships between the papilla dimensions assessed before orthodontic treatment and the alterations of papilla height and papilla base thickness after orthodontic closure of the diastema. (A) Papilla height versus papilla height alteration; (B) Papilla base thickness versus papilla height alteration; (C) Diastema width versus papilla base thickness alteration; (D) Papilla base thickness versus papilla base thickness alteration. PH, papilla height; PBT, papilla base thickness; DW, diastema width.
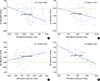
With respect to the alteration of PBT, the DW (
P=0.045) and PBT (
P<0.001) before the orthodontic treatment were found to be significant influential factors in the univariate regression analysis (
Figure 3C and D).
The multiple regression model that was formulated to explore the potential effects of the PH, PBT, and PBW before orthodontic treatment on the alteration of PH did not reach statistical significance (
P=0.06). However, it was found that 27% of the variance in the alteration of PBT could be explained by the PH, PBT, and PBW before the orthodontic treatment. Among the three independent variables, only the PBT (
P<0.001) significantly influenced the outcome, while the PBW and PH did not significantly influence the outcome (
Table 3).
Table 3
Multiple regression analysis with the alteration of papilla base thickness after orthodontic closure of the maxillary midline diastema as the dependent variable (mean change 0.5 mm)

|
Independent Variablesa) (Adjusted R2: 0.27) |
F-value: 7.634 |
P-value of the model: 0.000 |
|
Estimate |
SE of estimate |
P-value |
|
Intercept |
3.756 |
1.069 |
0.001 |
|
PBT |
-0.481 |
0.117 |
0.000 |
|
PBW |
0.080 |
0.086 |
0.353 |
|
PH |
0.009 |
0.096 |
0.925 |
DISCUSSION
After orthodontic closure of the maxillary midline diastema, PH decreased by 0.8 mm apically, but PBT increased by 0.5 mm in the facio-lingual direction. It has been claimed that orthodontic approximation of two adjacent teeth with diastema would increase PH coronally by squeezing the papilla volume in the proximal area [
346]. However, the results of the clinical studies assessing the PH change after orthodontic closure of diastema were contradictory. In corroboration of the current study results, the heights of the interdental papillae reduced following closure of the diastema in young patients between 13 and 16 years of age [
7]. In contrast, it has been reported that orthodontic approximation of two adjacent teeth with diastema in adult periodontitis patients significantly enhanced the levels of the interdental papilla [
8]. However, patients were reported to have a certain degree of extrusion and labial inclination due to pathologic tooth migration as a result of periodontal disease. There is a possibility of orthodontic palatal and intrusive movements that may affect the clinical crown height, and consequently the papilla level as well, since the papilla level was measured as the distance from the incisal margin of the two adjacent target teeth to the corresponding tips of interdental papillae [
7]. However, the present study included only periodontally healthy young patients, and excluded patients who showed severe extrusion or labial tipping of the maxillary anterior teeth. Furthermore, to minimize the effect of possible intrusion during orthodontic treatment, PH was measured as the distance between the papilla tip level and the reference line connecting the mid-facial gingival margins of two maxillary central incisors [
11] (
Figure 2A). In fact, CCH, which could be influenced by the palatal and intrusive movements, did not change during the orthodontic treatment (
P=0.32) (
Table 2).
With respect to the measurements of PH, the proportion of the papilla level in relation to CCH was used to indirectly assess the PH changes after orthodontic closure of the diastema in the clinical photographs [
7], and the distance between the incisal edge and the papilla tip was measured directly in the patients with an electronic caliper [
8]. In the current study, since the exact location of the papilla tip was not visible in most study models, indirect photographic assessment was utilized to assess alterations of PH. It has been shown that carefully taken photographs and study models could provide accurate measurements in comparison to the direct clinical measures of keratinized gingiva [
10]. To minimize potential errors in the assessments, the CCH in each photograph was calibrated to that measured on the study model taken on the same date. The mean difference in the CCH between the two measurements was 0.02 mm (SD 0.12). Hence, the results of this study could be considered reliable, with this level of accuracy of the methods.
Incomplete papilla fill, resulting in a “black triangle” in the proximal embrasure between the teeth, is a concern from an esthetic perspective, particularly in the visible anterior teeth region. Hence, the degree of papilla fill is a critical assessment in the judgment of the esthetic outcome [
13]. Even though PH was statistically significantly decreased after orthodontic closure of the diastema in the present study (0.8 mm;
P<0.001), all 60 patients were judged to have a complete papilla fill between maxillary central incisors after closure of the diastema. Hence, a complete papilla fill seemed to have been achieved by the creation of a new proximal contact between the maxillary central incisors, and possibly with a relatively short distance between the contact point and the bone crest in the proximal area [
2]. The 0.8 mm difference in PH after orthodontic closure of the diastema may not be as critical for laypeople as it is for dentists in appreciation of the papilla appearance. The laypersons did not perceive a significant difference in attractiveness even when evaluating the maximum 2 mm deviation in the papilla level [
14].
In addition to PH, which is considered to be an important factor from an esthetic perspective, facio-lingual thickness of the papilla base (PBT) was evaluated in the current study. The PBT dimension was emphasized in relation to the papilla height and fill [
21516]. These findings were based on the observation of a positive relationship between tissue thickness and height of periodontal tissue [
17] as well as peri-implant mucosa [
918]. In the current study, PBT increased by 0.5 mm after orthodontic closure of the diastema (
P<0.001), and 82% of the 55 sites showed an increase in the PBT dimension. Besides, the PBT change after orthodontic closure of the diastema was greater when the diastema width before the orthodontic treatment was greater. Based on the results, the “squeezing” force generated during orthodontic closure of the diastema seemed to push the papilla in the mesio-distal direction and not in the apico-coronal direction. Hence, PBT increased, but PH decreased after orthodontic closure of the diastema.
The alterations of PH and PBT after orthodontic closure of the diastema were negatively influenced by the PBT before the treatment. This means that the greater the PBT before orthodontic treatment, the more the PH and PBT decreased. In contrast, the lesser the PBT before orthodontic treatment, the more the PH and PBT increased. Hence, the final PH and PBT dimensions after closure of the diastema appeared to converge toward a certain dimension, that is, biologic width. Based on the above-mentioned findings from the present study, it seemed that the primary dimensions before orthodontic treatment, especially the PBT dimension, significantly affected the alteration of the PH and PBT after orthodontic closure of the diastema.
The vertical dimension of the soft tissues at the proximal sites, that is, the papilla height between an implant and a tooth in the maxillary anterior region, was greater in individuals with a thick gingival/periodontal biotype in comparison to those with a thin biotype [
18]. In line with this finding, it was reported that the shape of the teeth had a significant impact on the interdental papilla score in the patients with pathologic tooth migration [
8]. In the present study, the CCW/CCH ratio did not influence the alterations of PH or PBT after orthodontic closure of the diastema, but, interestingly, the correlation analysis between the papilla dimensions before orthodontic treatment revealed that PH was significantly correlated with PBT (
P<0.001, Pearson’s
r=0.534). However, all patients in the present study were periodontally healthy and were found to have a complete papilla fill after orthodontic closure of the diastema.
In order to better understand the role of the dimensional factors constituting the papilla embrasure space in the alteration of PH and PBT after orthodontic closure of the diastema, we formulated a multivariate model including the 3-dimensional papilla dimensions, that is, PH, PBT, and PBW before the orthodontic treatment as predictors [
19]. Among the 3-dimensional papilla dimensions, only the PBT before treatment influenced the alterations of PBT after orthodontic closure of the diastema. Hence, one has to evaluate the PBT dimension before the orthodontic treatment as a potential factor for esthetic appreciation since PBT was reported to affect the papilla height and fill in the literature.
The limitations of this study were that the amount of the diastema closed by orthodontic approximation was limited (mean 1.1 mm, range, 0.3–3.0 mm), since the patients were selected from an esthetic point of view, and hard tissue assessment was not made in relation to its role in supporting the overlying soft tissues [
8]. The present study mainly focused on the evaluation of various papilla dimensions before orthodontic treatment in relation to the alterations of PH and PBT after orthodontic closure of the diastema. However, there may be additional factors, for example, tooth positions in relation to extrusion and buccal tipping, or directions and degree of orthodontic approximation force, which should be evaluated as potential factors influencing the alterations of PH and PBT after orthodontic closure of the diastema.
In conclusion, PH decreased but PBT increased after orthodontic closure of the diastema. The papilla dimensions before orthodontic treatment influenced the alterations of PH and PBT after closure of the diastema. The PBT increased more when the diastema width before the orthodontic treatment was greater.







 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download