1. Salvi GE, Aglietta M, Eick S, Sculean A, Lang NP, Ramseier CA. Reversibility of experimental peri-implant mucositis compared with experimental gingivitis in humans. Clin Oral Implants Res. 2012; 23:182–190.

2. Heitz-Mayfield LJ, Lang NP. Comparative biology of chronic and aggressive periodontitis vs. peri-implantitis. Periodontol 2000. 2010; 53:167–181.

3. Zitzmann NU, Berglundh T. Definition and prevalence of peri-implant diseases. J Clin Periodontol. 2008; 35:286–291.

4. Van Steenberghe D, Klinge B, Lindén U, Quirynen M, Herrmann I, Garpland C. Periodontal indices around natural and titanium abutments: a longitudinal multicenter study. J Periodontol. 1993; 64:538–541.

5. Lang NP, Mombelli A, Tonetti MS, Brägger U, Hämmerle CH. Clinical trials on therapies for peri-implant infections. Ann Periodontol. 1997; 2:343–356.

6. Roos-Jansåker AM, Lindahl C, Renvert H, Renvert S. Nine- to fourteen-year follow-up of implant treatment. Part I: implant loss and associations to various factors. J Clin Periodontol. 2006; 33:283–289.

7. Serino G, Ström C. Peri-implantitis in partially edentulous patients: association with inadequate plaque control. Clin Oral Implants Res. 2009; 20:169–174.

8. Ferreira SD, Silva GL, Cortelli JR, Costa JE, Costa FO. Prevalence and risk variables for peri-implant disease in Brazilian subjects. J Clin Periodontol. 2006; 33:929–935.

9. Schou S, Holmstrup P, Hjørting-Hansen E, Lang NP. Plaque-induced marginal tissue reactions of osseointegrated oral implants: a review of the literature. Clin Oral Implants Res. 1992; 3:149–161.

10. Lindquist LW, Carlsson GE, Jemt T. A prospective 15-year follow-up study of mandibular fixed prostheses supported by osseointegrated implants. Clinical results and marginal bone loss. Clin Oral Implants Res. 1996; 7:329–336.

11. Axelsson P, Lindhe J, Nyström B. On the prevention of caries and periodontal disease. Results of a 15-year longitudinal study in adults. J Clin Periodontol. 1991; 18:182–189.

12. Duncan JP, Taylor TD, Kosis DL. A simple toothbrush modification for easier implant-supported prosthesis hygiene. J Prosthodont. 1998; 7:49–50.

13. Vandekerckhove B, Quirynen M, Warren PR, Strate J, van Steenberghe D. The safety and efficacy of a powered toothbrush on soft tissues in patients with implant-supported fixed prostheses. Clin Oral Investig. 2004; 8:206–210.

14. Sicilia A, Arregui I, Gallego M, Cabezas B, Cuesta S. A systematic review of powered vs manual toothbrushes in periodontal cause-related therapy. J Clin Periodontol. 2002; 29:Suppl 3. 39–54.

15. Wolff L, Kim A, Nunn M, Bakdash B, Hinrichs J. Effectiveness of a sonic toothbrush in maintenance of dental implants. A prospective study. J Clin Periodontol. 1998; 25:821–828.

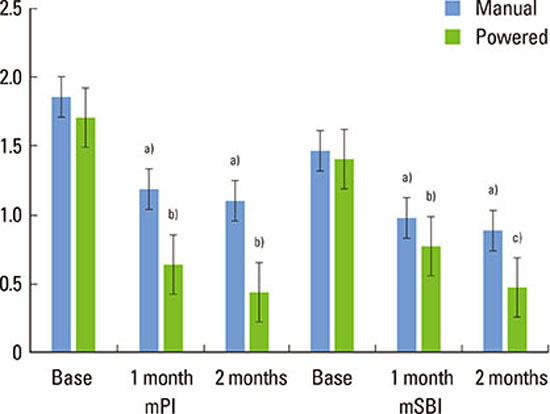
16. Swierkot K, Brusius M, Leismann D, Nonnenmacher C, Nüsing R, Lubbe D, et al. Manual versus sonic-powered toothbrushing for plaque reduction in patients with dental implants: an explanatory randomised controlled trial. Eur J Oral Implantol. 2013; 6:133–144.
17. Bass CC. An effective method of personal oral hygiene. J La State Med Soc. 1954; 106:57–73.

18. Mombelli A, van Oosten MA, Schurch E Jr, Land NP. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol. 1987; 2:145–151.

19. Assaf AV, Tagliaferro EP, Meneghim Mde C, Tengan C, Pereira AC, Ambrosano GM, et al. A new approach for interexaminer reliability data analysis on dental caries calibration. J Appl Oral Sci. 2007; 15:480–485.

20. Kim HY. Statistical notes for clinical researchers: Evaluation of measurement error 1: using intraclass correlation coefficients. Restor Dent Endod. 2013; 38:98–102.

21. Ainamo J, Xie Q, Ainamo A, Kallio P. Assessment of the effect of an oscillating/rotating electric toothbrush on oral health. A 12-month longitudinal study. J Clin Periodontol. 1997; 24:28–33.

22. van der Weijden GA, Timmerman MF, Reijerse E, Danser MM, Mantel MS, Nijboer A, et al. The long-term effect of an oscillating/rotating electric toothbrush on gingivitis. An 8-month clinical study. J Clin Periodontol. 1994; 21:139–145.

23. Yoshie H, Kobayashi T, Tai H, Galicia JC. The role of genetic polymorphisms in periodontitis. Periodontol 2000. 2007; 43:102–132.

24. Michalowicz BS, Diehl SR, Gunsolley JC, Sparks BS, Brooks CN, Koertge TE, et al. Evidence of a substantial genetic basis for risk of adult periodontitis. J Periodontol. 2000; 71:1699–1707.

25. Yaacob M, Worthington HV, Deacon SA, Deery C, Walmsley AD, Robinson PG, et al. Powered versus manual toothbrushing for oral health. Cochrane Database Syst Rev. 2014; 6:CD002281.

26. Grender J, Williams K, Walters P, Klukowska M, Reick H. Plaque removal efficacy of oscillating-rotating power toothbrushes: review of six comparative clinical trials. Am J Dent. 2013; 26:68–74.
27. Verma S, Bhat KM. Acceptability of powered toothbrushes for elderly individuals. J Public Health Dent. 2004; 64:115–117.









 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download