1. Albrektsson T, Zarb GA. Current interpretations of the osseointegrated response: clinical significance. Int J Prosthodont. 1993; 6:95–105.
2. Lioubavina-Hack N, Lang NP, Karring T. Significance of primary stability for osseointegration of dental implants. Clin Oral Implants Res. 2006; 17:244–250.

3. Bayarchimeg D, Namgoong H, Kim BK, Kim MD, Kim S, Kim TI, et al. Evaluation of the correlation between insertion torque and primary stability of dental implants using a block bone test. J Periodontal Implant Sci. 2013; 43:30–36.

4. Hong J, Lim YJ, Park SO. Quantitative biomechanical analysis of the influence of the cortical bone and implant length on primary stability. Clin Oral Implants Res. 2012; 23:1193–1197.

5. Javed F, Almas K. Osseointegration of dental implants in patients undergoing bisphosphonate treatment: a literature review. J Periodontol. 2010; 81:479–484.

6. Javed F, Romanos GE. Impact of diabetes mellitus and glycemic control on the osseointegration of dental implants: a systematic literature review. J Periodontol. 2009; 80:1719–1730.

7. Roze J, Babu S, Saffarzadeh A, Gayet-Delacroix M, Hoornaert A, Layrolle P. Correlating implant stability to bone structure. Clin Oral Implants Res. 2009; 20:1140–1145.

8. Tabassum A, Meijer GJ, Wolke JG, Jansen JA. Influence of the surgical technique and surface roughness on the primary stability of an implant in artificial bone with a density equivalent to maxillary bone: a laboratory study. Clin Oral Implants Res. 2009; 20:327–332.

9. Tabassum A, Meijer GJ, Wolke JG, Jansen JA. Influence of surgical technique and surface roughness on the primary stability of an implant in artificial bone with different cortical thickness: a laboratory study. Clin Oral Implants Res. 2010; 21:213–220.

10. Seong WJ, Kim HC, Jeong S, DeVeau DL, Aparicio C, Li Y, et al. Ex vivo mechanical properties of dental implant bone cement used to rescue initially unstable dental implants: a rabbit study. Int J Oral Maxillofac Implants. 2011; 26:826–836.
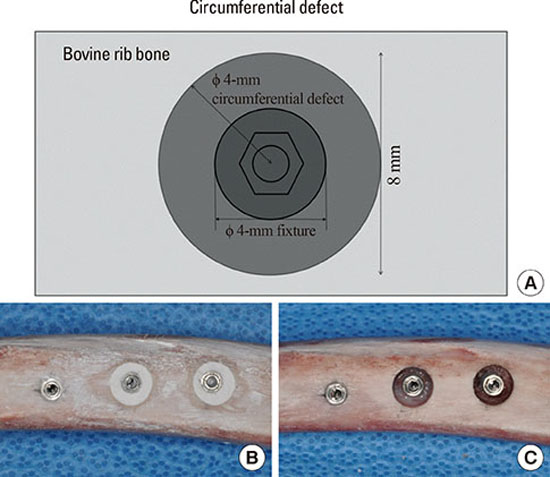
11. Shin SY, Shin SI, Kye SB, Hong J, Paeng JY, Chang SW, et al. The effects of defect type and depth, and measurement direction on the implant stability quotient (ISQ) value. J Oral Implantol. 2014; Jun. 26. [Epub].
http://dx.doi.org/10.1563/aaid-joi-D-13-00331.

12. Park JH, Choi CG, Jeon SR, Rhim SC, Kim CJ, Roh SW. Radiographic analysis of instrumented posterolateral fusion mass using mixture of local autologous bone and b-TCP (PolyBone(R)) in a lumbar spinal fusion surgery. J Korean Neurosurg Soc. 2011; 49:267–272.

13. Park JH, Roh SW. Anterior cervical interbody fusion using polyetheretherketone cage filled with autologous and synthetic bone graft substrates for cervical spondylosis: comparative analysis between PolyBone® and iliac bone. Neurol Med Chir (Tokyo). 2013; 53:85–90.

14. Park YH, Kim SG, Lee JW, Yoon YH. Obliteration of temporal dorsal bulla in guinea pigs using different types of calcium phosphate. Int J Pediatr Otorhinolaryngol. 2011; 75:1176–1180.

15. Abbah SA, Lam CX, Hutmacher DW, Goh JC, Wong HK. Biological performance of a polycaprolactone-based scaffold used as fusion cage device in a large animal model of spinal reconstructive surgery. Biomaterials. 2009; 30:5086–5093.

16. Byun HY, Wang HL. Sandwich bone augmentation using recombinant human platelet-derived growth factor and beta-tricalcium phosphate alloplast: case report. Int J Periodontics Restorative Dent. 2008; 28:83–87.
17. Cha JK, Park JC, Jung UW, Kim CS, Cho KS, Choi SH. Case series of maxillary sinus augmentation with biphasic calcium phosphate: a clinical and radiographic study. J Periodontal Implant Sci. 2011; 41:98–104.

18. Elahi MM, Vanduzer S, Spears J, Gibson J, Mitra A. Frontal sinus obliteration with beta-tricalcium phosphate. J Craniofac Surg. 2004; 15:967–970.
19. Kishimoto M, Kanemaru S, Yamashita M, Nakamura T, Tamura Y, Tamaki H, et al. Cranial bone regeneration using a composite scaffold of Beta-tricalcium phosphate, collagen, and autologous bone fragments. Laryngoscope. 2006; 116:212–216.

20. Suba Z, Takacs D, Matusovits D, Barabas J, Fazekas A, Szabo G. Maxillary sinus floor grafting with beta-tricalcium phosphate in humans: density and microarchitecture of the newly formed bone. Clin Oral Implants Res. 2006; 17:102–108.

21. Sennerby L, Meredith N. Implant stability measurements using resonance frequency analysis: biological and biomechanical aspects and clinical implications. Periodontol 2000. 2008; 47:51–66.

22. Ivanoff CJ, Sennerby L, Lekholm U. Influence of initial implant mobility on the integration of titanium implants. An experimental study in rabbits. Clin Oral Implants Res. 1996; 7:120–127.

23. Morris HF, Ochi S, Orenstein IH, Petrazzuolo V. AICRG, Part V: Factors influencing implant stability at placement and their influence on survival of Ankylos implants. J Oral Implantol. 2004; 30:162–170.

24. Herr Y. Atlas of periodontology-based implantology I. Seoul: Yenang Inc.;2012.
25. Fischer K, Stenberg T, Hedin M, Sennerby L. Five-year results from a randomized, controlled trial on early and delayed loading of implants supporting full-arch prosthesis in the edentulous maxilla. Clin Oral Implants Res. 2008; 19:433–441.

26. Valderrama P, Oates TW, Jones AA, Simpson J, Schoolfield JD, Cochran DL. Evaluation of two different resonance frequency devices to detect implant stability: a clinical trial. J Periodontol. 2007; 78:262–272.

27. Veltri M, Balleri P, Ferrari M. Influence of transducer orientation on Osstell stability measurements of osseointegrated implants. Clin Implant Dent Relat Res. 2007; 9:60–64.









 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download