This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
The purpose of this report was to describe the clinical and microbiological characteristics of two rare cases of necrotizing stomatitis, and the outcomes of a non-invasive treatment protocol applied in both cases.
Methods
We report two cases of necrotizing stomatitis in a rare location in the hard palate of a 40-year-old woman and a 28-year-old man. Neither had a relevant medical history and both presented with highly painful ulceration in the palate and gingival margin that was accompanied by suppuration and necrosis. 3% hydrogen peroxide was applied to the lesions using sterile swabs, and antibiotic and anti-inflammatory treatment was prescribed to both patients in addition to two daily oral rinses of 0.2% chlorhexidine.
Results
In both cases, radiological examination ruled out bone involvement, and exfoliative cytology revealed a large inflammatory component and the presence of forms compatible with fusobacteria and spirochetes. There was a rapid response to treatment and a major improvement was observed after 48 hours, with almost complete resolution of the ulcerated lesions and detachment of necrotic areas with partial decapitation of gingival papillae.
Conclusions
Necrotizing periodontal lesions can hinder periodontal probing and the mechanical removal of plaque in some cases due to the extreme pain suffered by the patients. We present a non-invasive treatment approach that can manage these situations effectively.
Keywords: Histology, Microbiology, Necrotizing stomatitis, Necrotizing ulcerative gingivitis
INTRODUCTION
Necrotizing periodontal diseases are the most severe inflammatory periodontal disorders caused by bacterial plaque [
1]. They are classified according to their extent, as necrotizing ulcerative gingivitis, periodontitis, or stomatitis, the most extensive and rare form, in which the affected area extends beyond the mucogingival junction to other parts of the oral cavity, such as the tongue, cheeks or palate [
2]. It has been suggested that these clinical forms are different stages of the same process [
3].
Necrotizing periodontal diseases are now rare in developed countries, being more frequent in young adults [
4]. The prevalence of necrotizing gingivitis, the most common presentation, varies over a wide range from 6.7% in Chilean students [
5] to 0.001% in young Danish soldiers, and is commonly associated with immunodeficiency [
1]. The onset of symptoms is usually abrupt and there is a tendency toward recurrence.
These diseases are clinically characterized by punched-out, ulcerated, and necrotic lesions that may be covered by a pseudomembrane of necrotic remains. The ulcerations are extremely painful and can preclude periodontal examination or other oral handling. Spontaneous bleeding typically results from the exposure of connective tissue. Other possible clinical features include the presence of oral malodor, adenopathies, fever, and/or general discomfort [
6].
Reported predisposing factors for necrotizing periodontal disease are Caucasian race, young age, a change in life habits, psychological tension, malnutrition, prolonged stress with insufficient rest, smoking, and alcohol consumption, which are all related to poor oral hygiene [
2].
Here, we report two atypical cases of necrotizing stomatitis, describing the clinical and microbiological data, treatment approach, and successful outcomes.
CASE DESCRIPTION
Case 1
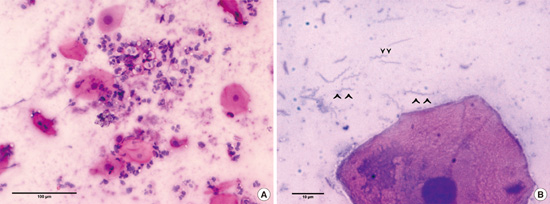
A 40-year-old woman attended the School of Dentistry of the University of Granada with a 24-hour history of general discomfort, intense oral pain and halitosis. She was a non-smoker and had no medical history of interest. The results of a recent routine biochemical blood analysis had been normal but she reported experiencing work-related stress. It was not the first time she had experienced an outbreak of this type. Clinical examination revealed a fibrin-covered ulcer with an erythematous base, 1.2 cm in diameter, in the palatal rugae. Five palatal gingival papillae were also affected by ulceration, corresponding to three upper incisors and their gingival margins.
All areas showed a necrotic appearance and visible suppuration. The lesions were extremely painful, hindering periodontal probing (
Figure 1A).
 | Figure 1(A) Clinical photograph of the lesions presented in case 1 at the time of examination. (B) Clinical photograph of the lesions presented in case 1 after 48 hours. 
|
Case 2
A 28-year-old man with no relevant medical history attended the School of Dentistry of the University of Granada reporting strong oral pain after a weekend of abundant alcohol and tobacco consumption and lack of rest. Clinical examination revealed multiple ulcers covered with a grayish pseudomembrane in the palatal rugae, papillary necrosis at teeth 21 and 22, and ulceration throughout the gingival margin and gingival papillae of the second quadrant (
Figure 2A). Periodontal probing was not possible due to the intense pain.
 | Figure 2(A) Clinical photograph of the lesions presented in case 2 at the time of examination. (B) Clinical photograph of the lesions presented in case 2 after 48 hours. 
|
Complementary tests
Panoramic X-ray examination of the patients ruled out maxillary bone involvement in both cases (
Figure 3A and B). Several exfoliative cytology specimens were obtained from necrotic palatal gingival papillae using sterile swabs. Samples from both cases were stained with hematoxylin-eosin to evaluate cytological features and the presence of bacteria. Histological analysis evidenced acute inflammatory cells and polymicrobial microbiota with a wide variety of bacterial morphotypes and forms compatible with spirochetes and fusobacteria (
Figure 4A and B). Following Mombelli’s technique [
7], blotting paper tips (No. 30) were inserted in the gingival sulcus for microbiological culture of the crevicular fluid in regenerated Schaedler broth supplemented with hemin and vitamin K. The isolation and identification procedures yielded no conclusive results.
 | Figure 3(A) Panoramic X-ray of the patient in case 1. (B) Panoramic X-ray of the patient in case 2. 
|
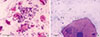 | Figure 4(A) Histologic image from exfoliative cytology showing acute inflammatory cells along with desquamated epithelial cells in case 1. (B) Histologic image from exfoliative cytology showing forms compatible with spirochetes and fusiform bacteria in case 2. 
|
Treatment and outcomes
After the two cases were diagnosed with necrotizing stomatitis and written informed consent was obtained, 3% hydrogen peroxide was gently applied to the lesions using sterile swabs, for debridement of the necrotic areas. Both patients were prescribed oral 875/125 mg amoxicillin/clavulanic acid and 600 mg ibuprofen every 8 hours and oral rinses with 0.2% chlorhexidine every 12 hours. Both cases showed a rapid response to treatment, and a major improvement in symptoms was observed at 48 hours, with almost complete resolution of the ulcerated areas, which were covered by a layer of fibrin, and the detachment of necrotic areas with partial decapitation of gingival papillae (
Figure 1B and
2B). Patients were recommended to return to their normal oral hygiene habits as soon as possible.
DISCUSSION
Necrotizing periodontal diseases have an acute onset and require urgent treatment; they all share similar characteristics but differ in their extent. This report describes two cases of an atypical presentation of necrotizing stomatitis, the most extensive form, associated with work-related stress in one case and with alcohol and tobacco abuse and lack of sleep in the other, which are all traditional risk factors for necrotizing disease because of the resulting downregulation of the host immune response. Most cases of necrotizing stomatitis reported in the literature are associated with systemic factors such as AIDS, chemotherapy or tumor growth [
8910]. In contrast, the presenting patients did not have any significant systemic disease or treatment that could be associated with the disease.
Horning and Cohen described seven stages of necrotizing periodontal disease according to the oral regions affected, ranging from necrosis of the tip of the papilla (stage 1) to necrosis that perforates the skin of the cheek (stage 7) [
2]. This classification accords with the general view that this disease advances in a vestibular direction. The present cases could be considered to be stage 5 of Horning and Cohen (necrotizing stomatitis) because they showed a palatine progression and even approached the midline, where the palatal masticatory mucosa is affected instead of vestibular alveolar mucosa. However, unlike in other published cases [
8], no bone destruction was observed in either patient; this is notable because bone destruction is expected in necrotizing stomatitis, which is considered to be a progression of necrotizing periodontitis.
Microbiological analysis of subgingival plaque samples provided no conclusive results, while the histological study revealed forms compatible with spirochetes and fusobacteria in the inflammatory infiltrate [
1]. Microbiological data are not considered to provide diagnostic information because of the wide heterogeneity of the flora that participate in this process; the classic association of fusiform bacilli with spirochetes has no etiologic implications and may result from a secondary growth [
4].
As in the present patients, necrotizing stomatitis is often associated with intense, disabling pain that makes food or liquid intake difficult and becomes extreme during periodontal probing or scaling and root planning procedures [
1]. Due to the impossibility of mechanical debridement because of the pain, we adopted a more conservative approach in both cases, with the application of hydrogen peroxide and prescription of oral rinses of chlorhexidine to prevent plaque formation over the debrided lesions. We also prescribed antibiotics and anti-inflammatory drugs against the infection and symptoms, although amoxicillin/clavulanic acid was used instead of metronidazole, which is considered the first choice antibiotic in these cases. Amoxicillin/clavulanic acid is a broad-spectrum antibiotic that is also effective in necrotizing periodontal diseases, which have a great variety of microbial species involved in their etiology [
11]. Both patients showed an excellent response within 48 hours of treatment.
Together with the rarity and severity of the lesions, we would also like to highlight that an alternative treatment protocol, consisting of local hydrogen peroxide and chlorhexidine rinses along with broad-spectrum antibiotics, was applied with successful outcomes. This approach could be considered as a suitable option when mechanical debridement is not possible. We have been unable to identify recent studies on necrotizing periodontal disease. Most literature on necrotizing periodontal disease is over 20 years old, indicating the limited current scientific evidence available.