This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
The purpose of the present study was to evaluate the effect of root planing on the reduction of probing pocket depth and the gain of clinical attachment depending on the pattern of bone resorption (vertical versus horizontal bone loss) in the interproximal aspect of premolar teeth that showed an initial probing pocket depth of 4-6 mm.
Methods
In this study, we analyzed 68 teeth (15 from the maxilla and 53 from the mandible) from 32 patients with chronic periodontitis (17 men and 15 women; mean age, 53.6 years). The probing pocket depth and clinical attachment level at all six sites around each tooth were recorded before treatment to establish a baseline value, and then three months and six months after root planing.
Results
The reduction in interdental pocket depth was 1.1 mm in teeth that experienced horizontal bone loss and 0.7 mm in teeth that experienced vertical bone loss. Interdental attachment was increased by 1.0 mm in teeth with horizontal bone loss and by 0.7 mm in teeth with vertical bone loss. The reduction of probing pocket depth and the gain of clinical attachment occurred regardless of defect patterns three and six months after root planing.
Conclusions
The reduction of pocket depth and gain in the clinical attachment level were significantly larger in horizontally patterned interproximal bone defects than in vertical bone defects.
Keywords: Alveolar bone loss, Periodontal pocket, Root planing
INTRODUCTION
Periodontitis is an inflammatory disease caused by a subset of the bacteria present in dental plaque that attack vulnerable periodontal tissue, leading to periodontal pocket depth formation, gingival recession, loss of connective tissue attachment, and progressive destruction of the alveolar bone and periodontal ligament accompanied by a wide range of symptoms [
1,
2,
3]. The radiographic pattern of bone loss surrounding infected teeth manifests either horizontally or vertically [
4].
The initial treatment of periodontitis involves controlling its causes, reducing the bacterial load on the supragingival and subgingival surfaces through nonsurgical periodontal treatment (root planing), drug treatment if needed, and reinforcing oral hygiene education [
5]. These nonsurgical treatments are considered the gold standard for controlling periodontitis [
6]. A long-term observational study reported that attachment loss increased by 0.05-0.3 mm yearly in patients who did not undergo periodontal treatment [
7].
According to Heitz-Mayfield et al. [
1] and Lindhe et al. [
8], the critical probing depth represents a threshold value of the probing depth value, above which the outcome of therapy will result in attachment gain and below which the outcome of therapy will result in clinical attachment loss. According to Lindhe et al. [
8], the critical probing depth of root planing is 2.9±0.3 mm; if the pocket depth is greater than this, gain of clinical attachment is optimally achieved through treatment with root planing. If the pocket depth is greater than 4.2±0.2 mm, clinical attachment gain does occur through surgical treatment. If it is deeper than 5.4 mm, the gain of clinical attachment level is greater with periodontal surgery than with root planing. Moreover, according to Heitz-Mayfield et al. [
1], root planing is generally preferable when the pocket depth is 1-3 mm, although periodontal surgery is superior in terms of pocket depth reduction. However, root planing is superior in terms of gain of clinical attachment level when the pocket depth is 4-6 mm, and periodontal surgery is superior overall when the pocket depth is >6 mm.
Clinically, the response to periodontal treatment of teeth with periodontitis that have similar pocket depths differs depending on the pattern of bone loss. Bone loss can be categorized as horizontal or vertical. Vertical bone loss is evaluated based on the slope angle between the root and bone wall using radiographs. According to Linares et al. [
9], an angle less than 25° is narrow and an angle greater than 37° degrees is wide. Highly predictable results can be estimated in the regenerative treatment of cases with a slope angle of 25°-37°, when the slope angle is estimated from pretreatment radiographs. According to Steffensen and Weber [
10], most defects with an angle <45° showed a greater extent of bone acquisition. Furthermore, according to Lang [
11], when the defect angle is <45° in a single root, the mean bone acquisition was 1.22 mm after Widman flap surgery without bone resection, whereas only 0.05 mm of bone was acquired when the angle was between 45° and 90°. That is, when the defect angle was more acute, the results were better. Therefore, the defect angle corresponding to vertical loss was fixed at 25°-37° in the present study, and pocket depth and clinical attachment level were evaluated after treatment. Moreover, since defect shapes are classified based on radiographic images, this study focused on interdental bone. Only single-rooted premolars were used in this experiment in order to exclude the effect of treatment on the furcation area.
Although several studies [
12,
13] have described gains of clinical attachment level after root planing according to pocket depth, few have reported gains of clinical attachment level after root planing according to the pattern of interdental bone resorption. The purpose of the present study was to compare the effect of root planing on the reduction of probing pocket depth and the gain of clinical attachment depending on the pattern of bone resorption (vertical versus horizontal bone loss) in the interproximal aspects of premolar teeth that showed an initial probing pocket depth of 4-6 mm.
MATERIALS AND METHODS
Study design
Sixty-eight teeth were included from 32 patients (17 men and 15 women; mean age, 53.6 years) who visited Pusan National University Dental Hospital for periodontal treatment between March 2014 and April 2014 and were diagnosed with chronic periodontitis. The inclusion criteria were as follows: (1) chronic periodontitis, (2) horizontal/vertical bone loss in different quadrants (contralateral pattern), (3) pocket depth of 4-6 mm, (4) premolars, and (5) the presence of adjacent teeth and normal occlusion with opposing dentition.
The exclusion criteria were as follows: (1) systemic disease, (2) smoking, (3) prior periodontal treatment, (4) pregnancy, (5) alcohol or drug addiction, and (6) lack of cooperativeness or failure to maintain good oral hygiene.
The study protocol was approved by the Institutional Review Board (IRB # PNUDH-2014-012), Pusan National University Dental Hospital, Yangsan, Korea. All patients received a detailed description of the proposed study protocol and provided written informed consent to participate in the study.
Study methods
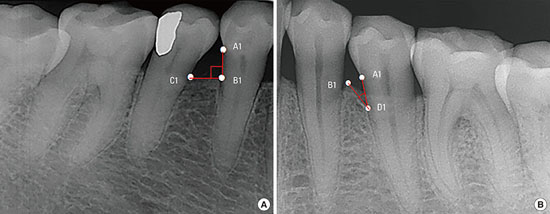
A clinical examination was conducted. Each tooth was divided into six parts (mesiobuccal, midbuccal, distobuccal, mesiolingual, midlingual, and distolingual), and the pocket depth and clinical attachment level were measured. Probing pocket depths and attachment levels were measured by a single experienced periodontist using a periodontal probe (Periodontal probe PFG-W, OSUNG Co., Gimpo, Korea). Bone loss at interdental sites was categorized as horizontal or vertical. The classification of a defect as involving horizontal or vertical bone loss was determined by the slope angle between the root and the interdental bone wall on radiographs. If the slope angle between the root and interdental bone wall was 90°±10° on radiographs, the defect was designated as horizontal bone loss, whereas if the angle of bone loss was between 25°-37°, the defect was designated as vertical bone loss (
Figure 1).
Figure 1
Bone loss at interdental sites was categorized as horizontal or vertical bone loss. (A) If the slope angle between the root and interdental bone wall was 90°±10° on radiographs, the defect was designated as horizontal bone loss. (B) If the angle of bone loss was between 25° and 37°, the defect was designated as vertical bone loss. A1, CEJ; B1, the top of the crest; C1, the top of the proximal bone crest of the adjacent tooth; D1, the bottom of the bone defect.

Nonsurgical periodontal treatment (root planing)
After the clinical examination, supragingival scaling was performed in all teeth included in the study, and the subjects received oral hygiene instructions. Subgingival curettage and root planing were performed under local anesthesia with an ultrasonic instrument and/or a hand instrument in the quadrant that included the subject tooth, preferentially after an interval of two weeks. Supportive treatment and clinical examinations were performed three and six months after root planing.
Measuring clinical indices
Probing pocket depth and clinical attachment level were measured at the time of root planing, as well as three and six months after treatment.
Probing pocket depth and attachment level on the mesiobuccal, midbuccal, distobuccal, mesiolingual, midlingual and distolingual sites of each tooth were measured using a constant-force periodontal probe with 1-mm markings. The values were rounded up to the nearest millimeter.
Statistical analysis
After root planing, the average changes in each clinical index of each tooth overall and at the buccal/labial and lingual/palatal interdental areas were determined. Additionally, the changes in each measurement between the first visit and after treatment were determined.
Statistical analysis was performed using SPSS (version 20 for Windows; SPSS Inc., Chicago, IL, USA), and the paired t-test and the Student's t-test were used to compare the changes in the two experimental groups. P <0.05 were considered to indicate statistical significance.
RESULTS
This study evaluated 68 teeth from 32 patients who were diagnosed with chronic periodontitis, evenly divided between teeth with horizontal and vertical bone loss defects. Fifteen defects were in the maxilla and 53 defects were in the mandible. Pre-treatment interdental pocket depth and clinical attachment level varied between the groups, but total pocket depth and clinical attachment level were not significantly different between the groups (
Table 1).
Table 1
Comparison of the average initial probing pocket depth (PD) and clinical attachment level (CAL) (mm) between groups.

|
Site |
Defect |
Mean |
SD |
Sample size |
P-value |
|
Total |
Vertical |
PD |
3.63 |
0.41 |
34 |
0.085 |
|
CAL |
3.76 |
0.05 |
0.049 |
|
Horizontal |
PD |
3.82 |
0.48 |
34 |
0.085 |
|
CAL |
4.06 |
0.05 |
0.049 |
|
Interdental |
Vertical |
PD |
4.34 |
0.47 |
34 |
0.002 |
|
CAL |
4.46 |
0.56 |
0.003 |
|
Horizontal |
PD |
4.74 |
0.55 |
34 |
0.002 |
|
CAL |
4.94 |
0.74 |
0.003 |
Probing pocket depth
In both groups of teeth, pocket depth was found to be significantly decreased three and six months after the first visit. However, the pocket depth did not decrease significantly between three and six months. After treatment, a greater decrease in pocket depth was observed in teeth with horizontal bone loss than in teeth with vertical bone loss (
Table 2).
Table 2
Comparison of the changes in probing depth between treatment and three and six months of follow-up.

|
Defect |
Site |
n |
Baseline to three months |
Three months to six months |
Baseline to six months |
|
Mean±SD |
P-value |
Mean±SD |
P-value |
Mean±SD |
P-value |
|
Horizontal |
Interdental PDC |
68 |
0.67±0.3 |
<0.001 |
0.04±0.24 |
0.285 |
0.72±0.36 |
<0.001 |
|
Total PDC |
204 |
1.07±0.83 |
<0.001 |
0.16±0.54 |
0.075 |
1.24±0.95 |
<0.001 |
|
Vertical |
Interdental PDC |
68 |
0.41±0.42 |
<0.001 |
0.07±0.3 |
0.186 |
0.48±0.42 |
<0.001 |
|
Total PDC |
204 |
0.71±0.69 |
<0.001 |
0.02±0.64 |
0.832 |
0.72±0.75 |
<0.001 |
|
Horizontal |
Interdental PDCD |
68 |
1.07±0.83 |
<0.006 |
0.16±0.59 |
0.164 |
1.24±0.95 |
<0.001 |
|
Total PDCD |
204 |
0.67±0.79 |
<0.001 |
0.04±0.56 |
0.659 |
0.72±0.90 |
<0.006 |
|
Vertical |
Interdental PDCD |
68 |
0.71±0.69 |
<0.006 |
0.02±0.64 |
0.164 |
0.72±0.75 |
<0.001 |
|
Total PDCD |
204 |
0.41±0.82 |
<0.001 |
0.07±0.57 |
0.659 |
0.48±0.84 |
<0.006 |
Furthermore, a significant decrease in interdental pocket depth was observed both three and six months after treatment, with a greater decrease observed in teeth with horizontal bone loss than in those with vertical bone loss. Both groups of teeth showed statistically significant differences (P<0.01) in total pocket depth both three and six months after the first visit. However, no significant difference was observed between three and six months after treatment.
Clinical attachment level
The attachment level at all sides of the teeth showed a statistically significant gain three and six months after root planing, but did not show a statistically significant difference between three and six months. Both three and six months after root planing, a significantly greater gain of clinical attachment level was observed for horizontal than for vertical bone loss (
P<0.01). Similar results were observed for the interdental attachment level at the buccal/labial and palatal/lingual interfaces (
Table 3). Similar results were also observed for total and interdental attachment levels.
Table 3
Comparison of the changes in clinical attachment level between treatment and three to six months of follow-up.

|
Defect |
Site |
n |
Baseline to three months |
Three months to six months |
Baseline to six months |
|
Mean±SD |
P-value |
Mean±SD |
P-value |
Mean±SD |
P-value |
|
Horizontal |
Interdental CAL |
68 |
0.70±0.36 |
<0.001 |
0.05±0.24 |
0.244 |
0.75±0.38 |
<0.001 |
|
Total CAL |
204 |
1.02±0.61 |
<0.001 |
0.16±0.53 |
0.086 |
1.18±0.68 |
<0.001 |
|
Vertical |
Interdental CAL |
68 |
0.39±0.38 |
<0.001 |
0.06±0.31 |
0.239 |
0.46±0.39 |
<0.001 |
|
Total CAL |
204 |
0.72±0.51 |
<0.001 |
0.02±0.47 |
0.856 |
0.74±0.46 |
<0.001 |
|
Horizontal |
Interdental CALD |
68 |
1.02±0.92 |
<0.039 |
0.16±0.61 |
0.172 |
1.18±1.01 |
<0.005 |
|
Total CALD |
204 |
0.70±0.81 |
<0.001 |
0.05±0.55 |
0.791 |
0.75±0.88 |
<0.001 |
|
Vertical |
Interdental CALD |
68 |
0.72±0.71 |
<0.039 |
0.02±0.64 |
0.172 |
0.74±0.77 |
<0.005 |
|
Total CALD |
204 |
0.39±0.78 |
<0.001 |
0.06±0.57 |
0.791 |
0.46±0.81 |
<0.001 |
DISCUSSION
In this study, the outcome of periodontal treatment was compared between different quadrants in each person, by limiting the sample to a single-root premolar with a pocket depth of 4-6 mm pocket depth and determining the clinical attachment level after root planing depending on the pattern of interdental bone resorption. Reduction of pocket depth was statistically significant (P<0.01) three and six months after root planing in areas of both horizontal and vertical bone loss. Moreover, the gain of clinical attachment level was statistically significant (P<0.01). Of note, greater reduction of pocket depth and gain of clinical attachment level were observed in teeth with horizontal bone loss than in teeth with vertical bone loss.
Although a significant reduction of pocket depth and gain of clinical attachment level were observed three and six months after root planing and supportive periodontal therapy, no statistically significant pocket depth reduction or gain of clinical attachment level occurred in the period from three to six months.
Tunkel et al. [
14], Torfason et al. [
15], and Hallmon and Rees [
16] found no significant differences between the results of non-surgical periodontal therapy depending on whether a hand instrument or ultrasound scaler was used; thus, this study excluded the effect of the instrument used in root planing. Moreover, Badersten et al. [
17] showed that the number of root planing sessions did not significantly affect the reduction of pocket depth or gain of clinical attachment level; thus, in this study, probing pocket depth and gain of clinical attachment level were measured after root planing was performed once.
The average reduction of interdental probing pocket depth was 1.1 mm in teeth with horizontal bone loss and 0.7 mm in teeth with vertical bone loss, which is similar to the results reported by Lang [
11]. According to Lang [
11], after motivating patients to follow oral hygiene instructions for one month and performing subgingival scaling and root planing, regions with a pocket depth of 4-6 mm showed a 1 mm decrease, while regions with a pocket depth of 7-12 mm showed a 2 mm decrease. Of this reduction, 50% was due to gingival recession followed by the relief of gingival swelling, while the other 50% was due to gain of clinical attachment level followed by tightening of soft tissue at the base of the lesion. Moreover, Lindhe et al. [
12], and Badersten et al. [
17,
18] have reported similar findings. However, the gain of clinical attachment level was greater in the study by Pihlstrom et al. [
19]. Lindhe et al. [
12] showed that a single-root tooth with an initial pocket depth of 4-6 mm showed a 0.7±0.4 mm gain of clinical attachment level 12 months after root planing therapy, while Pihlstrom et al. [
19] reported a 0.34-mm gain.
Overall, cases teeth horizontal bone loss showed a greater reduction of pocket depth and gain of clinical attachment level than those with vertical bone loss.
Our results were most similar to those of Lang et al. [
11], but differed from the results of other studies [
11,
12,
171819] that did not differentiate between horizontal and vertical bone loss, instead focusing only on pocket depth. In particular, the interdental area showed the greatest reduction of pocket depth and gain of clinical attachment level compared to the tooth overall, possibly because of the inclusion of 3 mm of pocket depth in the mid-buccal and mid-lingual area due to the focus on interdental bone loss. Moreover, a single clinician performed all the measurements, which may have been another reason for this result.
This study found that a greater reduction of pocket depth and gain of clinical attachment level was observed in teeth with horizontal bone loss than in those with vertical bone loss.
The sample of teeth included in this study was chosen considering radiographic bone loss and pocket depth alone. In order to confirm the factors that affect the outcomes of root planing, a more systemic study is necessary. Such a study would include a larger sample of teeth, classify them as maxillary and mandibular teeth, compare single-root teeth and multiple-root teeth, and determine treatment effects depending on the initial pocket depth.
ACKNOWLEDGEMENTS
This study was supported by a clinical research grant, Pusan National University Dental Hospital (2016).
References
1. Heitz-Mayfield LJ, Trombelli L, Heitz F, Needleman I, Moles D. A systematic review of the effect of surgical debridement vs. non-surgical debridement for the treatment of chronic periodontitis. J Clin Periodontol. 2002; 29:Suppl 3. 92–102.

2. Socransky SS, Haffajee AD. The bacterial etiology of destructive periodontal disease: current concepts. J Periodontol. 1992; 63:322–331.

3. Renvert S, Persson GR. A systematic review on the use of residual probing depth, bleeding on probing and furcation status following initial periodontal therapy to predict further attachment and tooth loss. J Clin Periodontol. 2002; 29:Suppl 3. 82–89.

4. Papapanou PN, Wennström JL. The angular bony defect as indicator of further alveolar bone loss. J Clin Periodontol. 1991; 18:317–322.

5. Van der Weijden GA, Timmerman MF. A systematic review on the clinical efficacy of subgingival debridement in the treatment of chronic periodontitis. J Clin Periodontol. 2002; 29:Suppl 3. 55–71.

6. Ishikawa I, Baehni P. Nonsurgical periodontal therapy--where do we stand now? Periodontol 2000. 2004; 36:9–13.

7. Brown LJ, Löe H. Prevalence, extent, severity and progression of periodontal disease. Periodontol 2000. 1993; 2:57–71.

8. Lindhe J, Socransky SS, Nyman S, Haffajee A, Westfelt E. “Critical probing depths” in periodontal therapy. J Clin Periodontol. 1982; 9:323–336.

9. Liñares A, Cortellini P, Lang NP, Suvan J, Tonetti MS. European Research Group on Periodontology (ErgoPerio). European Research Group on Periodontology ErgoPerio Guided tissue regeneration/deproteinized bovine bone mineral or papilla preservation flaps alone for treatment of intrabony defects. II: radiographic predictors and outcomes. J Clin Periodontol. 2006; 33:351–358.

10. Steffensen B, Webert HP. Relationship between the radiographic periodontal defect angle and healing after treatment. J Periodontol. 1989; 60:248–254.

11. Lang NP. Focus on intrabony defects-conservative therapy. Periodontol 2000. 2000; 22:51–58.
12. Lindhe J, Westfelt E, Nyman S, Socransky SS, Heijl L, Bratthall G. Healing following surgical/non-surgical treatment of periodontal disease. A clinical study. J Clin Periodontol. 1982; 9:115–128.

13. Badersten A, Nilvéus R, Egelberg J. Effect of nonsurgical periodontal therapy. I. Moderately advanced periodontitis. J Clin Periodontol. 1981; 8:57–72.

14. Tunkel J, Heinecke A, Flemmig TF. A systematic review of efficacy of machine-driven and manual subgingival debridement in the treatment of chronic periodontitis. J Clin Periodontol. 2002; 29:Suppl 3. 72–81.

15. Torfason T, Kiger R, Selvig KA, Egelberg J. Clinical improvement of gingival conditions following ultrasonic versus hand instrumentation of periodontal pockets. J Clin Periodontol. 1979; 6:165–176.

16. Hallmon WW, Rees TD. Local anti-infective therapy: mechanical and physical approaches. A systematic review. Ann Periodontol. 2003; 8:99–114.

17. Badersten A, Nilveus R, Egelberg J. Effect of nonsurgical periodontal therapy. III. Single versus repeated instrumentation. J Clin Periodontol. 1984; 11:114–124.

18. Badersten A, Nilveus R, Egelberg J. Effect of nonsurgical periodontal therapy. II. Severely advanced periodontitis. J Clin Periodontol. 1984; 11:63–76.

19. Pihlstrom BL, Oliphant TH, McHugh RB. Molar and nonmolar teeth compared over 6 1/2 years following two methods of periodontal therapy. J Periodontol. 1984; 55:499–504.









 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download