Abstract
Purpose
Methods
Results
Figures and Tables
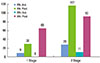
Figure 1
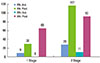
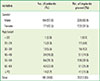
Table 1
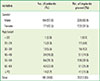
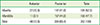
Table 2
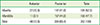
| Anterior | Posterior | Total | |
|---|---|---|---|
| Maxilla | 37 (10.5) | 147 (41.8) | 184 (52.3) |
| Mandible | 11 (3.1) | 157 (44.6) | 168 (47.7) |
| Total | 48 (13.6) | 304 (86.4) | 352 (100) |
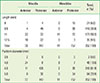
Table 3
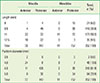
Table 4

Journal List > J Periodontal Implant Sci > v.44(1) > 1082451
| Anterior | Posterior | Total | |
|---|---|---|---|
| Maxilla | 37 (10.5) | 147 (41.8) | 184 (52.3) |
| Mandible | 11 (3.1) | 157 (44.6) | 168 (47.7) |
| Total | 48 (13.6) | 304 (86.4) | 352 (100) |

Seung-Il Shin 
https://orcid.org/http://orcid.org/0000-0001-8762-6169
Jeong-Ho Yun 
https://orcid.org/http://orcid.org/0000-0003-3929-4467
Sung-Geun Kim 
https://orcid.org/http://orcid.org/0000-0002-4698-5306
Byoungkyou Park 
https://orcid.org/http://orcid.org/0000-0003-1342-1413
Yeek Herr 
https://orcid.org/http://orcid.org/0000-0001-9243-7119
Jong-Hyuk Chung 
https://orcid.org/http://orcid.org/0000-0002-2678-1525