1. Garg AK, Quinones CR. Augmentation of the maxillary sinus: a surgical technique. Pract Periodontics Aesthet Dent. 1997; 9:211–219.
2. Wallace SS, Froum SJ. Effect of maxillary sinus augmentation on the survival of endosseous dental implants: a systematic review. Ann Periodontol. 2003; 8:328–343.

3. Hong SB, Kim JS, Shin SI, Han JY, Herr Y, Chung JH. Clinical treatment of postoperative infection following sinus augmentation. J Periodontal Implant Sci. 2010; 40:144–149.

4. Flanagan D. Arterial supply of maxillary sinus and potential for bleeding complication during lateral approach sinus elevation. Implant Dent. 2005; 14:336–338.

5. Rosano G, Taschieri S, Gaudy JF, Del Fabbro M. Maxillary sinus vascularization: a cadaveric study. J Craniofac Surg. 2009; 20:940–943.
6. Rosano G, Taschieri S, Gaudy JF, Weinstein T, Del Fabbro M. Maxillary sinus vascular anatomy and its relation to sinus lift surgery. Clin Oral Implants Res. 2011; 22:711–715.

7. Gaudy JF. Anatomie clinique. Rueil-Malmaison Cedex: Editions CdP;2003.
8. Solar P, Geyerhofer U, Traxler H, Windisch A, Ulm C, Watzek G. Blood supply to the maxillary sinus relevant to sinus floor elevation procedures. Clin Oral Implants Res. 1999; 10:34–44.

9. Traxler H, Windisch A, Geyerhofer U, Surd R, Solar P, Firbas W. Arterial blood supply of the maxillary sinus. Clin Anat. 1999; 12:417–421.

10. Elian N, Wallace S, Cho SC, Jalbout ZN, Froum S. Distribution of the maxillary artery as it relates to sinus floor augmentation. Int J Oral Maxillofac Implants. 2005; 20:784–787.
11. Guncu GN, Yildirim YD, Wang HL, Tozum TF. Location of posterior superior alveolar artery and evaluation of maxillary sinus anatomy with computerized tomography: a clinical study. Clin Oral Implants Res. 2011; 22:1164–1167.

12. Mardinger O, Abba M, Hirshberg A, Schwartz-Arad D. Prevalence, diameter and course of the maxillary intraosseous vascular canal with relation to sinus augmentation procedure: a radiographic study. Int J Oral Maxillofac Surg. 2007; 36:735–738.

13. Mardinger O, Namani-Sadan N, Chaushu G, Schwartz-Arad D. Morphologic changes of the nasopalatine canal related to dental implantation: a radiologic study in different degrees of absorbed maxillae. J Periodontol. 2008; 79:1659–1662.

14. Hur MS, Kim JK, Hu KS, Bae HE, Park HS, Kim HJ. Clinical implications of the topography and distribution of the posterior superior alveolar artery. J Craniofac Surg. 2009; 20:551–554.

15. Jung J, Yim JH, Kwon YD, Al-Nawas B, Kim GT, Choi BJ, et al. A radiographic study of the position and prevalence of the maxillary arterial endosseous anastomosis using cone beam computed tomography. Int J Oral Maxillofac Implants. 2011; 26:1273–1278.
16. Lofthag-Hansen S, Grondahl K, Ekestubbe A. Cone-beam CT for preoperative implant planning in the posterior mandible: visibility of anatomic landmarks. Clin Implant Dent Relat Res. 2009; 11:246–255.

17. Park YB, Jeon HS, Shim JS, Lee KW, Moon HS. Analysis of the anatomy of the maxillary sinus septum using 3-dimensional computed tomography. J Oral Maxillofac Surg. 2011; 69:1070–1078.

18. Neugebauer J, Ritter L, Mischkowski RA, Dreiseidler T, Scherer P, Ketterle M, et al. Evaluation of maxillary sinus anatomy by cone-beam CT prior to sinus floor elevation. Int J Oral Maxillofac Implants. 2010; 25:258–265.
19. Monsour PA, Dudhia R. Implant radiography and radiology. Aust Dent J. 2008; 53:Suppl 1. S11–S25.

20. Maestre-Ferrín L, Galan-Gil S, Carrillo-García C, Penarrocha-Diago M. Radiographic findings in the maxillary sinus: comparison of panoramic radiography with computed tomography. Int J Oral Maxillofac Implants. 2011; 26:341–346.
21. Yang SM, Park SI, Kye SB, Shin SY. Computed tomographic assessment of maxillary sinus wall thickness in edentulous patients. J Oral Rehabil. 2012; 39:421–428.

22. Ella B, Sedarat C, Noble Rda C, Normand E, Lauverjat Y, Siberchicot F, et al. Vascular connections of the lateral wall of the sinus: surgical effect in sinus augmentation. Int J Oral Maxillofac Implants. 2008; 23:1047–1052.
23. Lekholm U. Patient selection and preparation. In : Branemark PI, Zarb GA, Albrektsson T, editors. Tissue-integrated prostheses: osseointegration in clinical dentistry. Chicago: Quintessence;1985. p. 199–209.
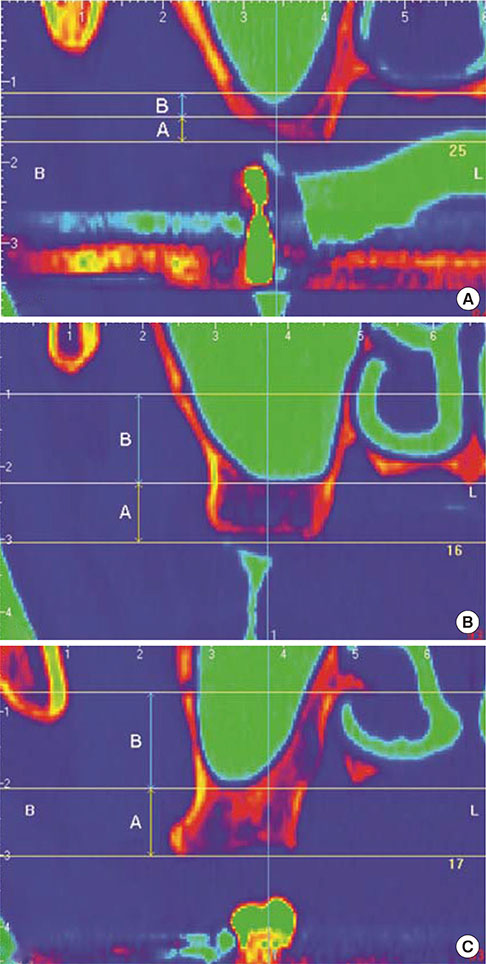
24. Kang SJ, Shin SI, Herr Y, Kwon YH, Kim GT, Chung JH. Anatomical structures in the maxillary sinus related to lateral sinus elevation: a cone beam computed tomographic analysis. Clin Oral Implants Res. 2013; 24:Suppl A100. 75–81.








 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download