Abstract
Purpose
The purpose of this study was to analyze the expression of inducible nitric oxide synthases (iNOS), tissue inhibitors of metalloproteinase (TIMP)-3, and TIMP-4 in the gingival tissues of periodontal patients with or without type 2 diabetes mellitus (DM).
Methods
Depending on the patient's systemic condition and clinical criteria of the gingiva, each gingival sample was classified into one of three groups. Sixteen clinically, systemically healthy patients (group 1), 16 periodontal patients (group 2), and 16 periodontal patients with DM (group 3) were included. Tissue samples in each group were collected, prepared, and analyzed by western blotting. Quantification of the relative amount of TIMP-3, TIMP-4, and iNOS was performed.
Results
The expression levels of iNOS and TIMP-3 both increased in group 1, group 2, and group 3 in increasing order, and were significantly higher in both group 2 and group 3 as compared to group 1 (P<0.05). The expression levels of TIMP-4 increased in the same order, but significantly increased in group 2 as compared to group 1, in group 3 as compared to group 1, and group 3 as compared to group 2 (P<0.05).
Inflammatory and immune responses to oral microorganisms are the preconditions of periodontitis. These responses protect gingival tissues against local microbial invasion and prevent microorganisms and/or microorganism-derived toxic substances from spreading into the tissues. Some toxic substances can damage host cells and tissues and others stimulate inflammatory, cellular, or humoral immune systems, which can damage peripheral tissues. The pathogens that are implicated in periodontitis are mainly anaerobic, gram-negative organisms, and (inflammatory) irritants such as lipopolysaccharide (LPS), referred to as putative periodontal pathogens [1]. Nitric oxide (NO) is a free radical and an important cellular signaling molecule involved in many physiological and pathological processes [2]. NO may act as a cytotoxic molecule against the invading microorganism and may be related to both harmful and beneficial effects on the general pathogenesis of tissues [3]. While excessive NO production is associated with tissue injury, NO produced by the endothelium is believed to play a protective role in the micro-vasculature [4]. Reher et al. [5] analyzed the association between severity of chronic periodontitis and NO levels in saliva and reported that its severity was related to salivary concentration and that NO might serve as a potential biologic marker for chronic periodontitis. In addition, Batista et al. [3] reported in a quantitative study that the presence of NO is an important medium in human periodontal disease. NO is synthesized from L-arginine by enzymes named NO synthases (NOS). Two of the three different NOS isoforms are endothelial NOS and brain or neuronal NOS and they produce a low concentration of NO for a short duration, while inducible NOS (iNOS) produces a high concentration of NO for a long period and the expression of iNOS is stimulated by bacterial products and cytokines such as interleukin (IL)-1 and tumor necrosis factor (TNF)-α [6].
Tissue inhibitors of metalloproteinases (TIMPs) were first identified in 1975 and described as proteins that might serve as potent inhibitors of collagenase in the culture medium of human fibroblasts and in human serum [7]. Since then, three new TIMPs have been discovered and designated as TIMP-2, TIMP-3, and TIMP-4, respectively. TIMPs are natural inhibitors of the matrix metalloproteinase (MMP) found in most tissues and inhibit the proteolytic activity of MMPs. A disturbance of the balance between TIMPs and MMPs might contribute to disease progress. However, TIMP-3 is the only member of the TIMP family that is found exclusively in the extracellular matrix (ECM) and regulated in a cell cycle-dependent fashion in certain cell types, and it may serve as a marker for terminal differentiation. On the other hand, TIMP-4 may function in a tissue-specific fashion in ECM hemostasis [8]. TIMP-3 expression is inducible, whereas TIMP-4 shows the most restricted pattern of expression [9].
Type 2 diabetes mellitus (DM) is a metabolic disease and is characterized by hyperglycemia. Type 2 DM comprises about 85-90% of diabetic cases, and advanced glycation end products excessively produced under diabetic conditions may promote inflammatory mediators. There is a biological correlation between type 2 diabetes and periodontal disease, and polymorphonuclear leukocyte deficiency, altered pathologic capacity of bacteria, and altered collagen metabolism of diabetic environment may cause severe periodontitis.
Although iNOS, TIMP-3, and TIMP-4 expression can be found in different diseases, it has not been reported that TIMP-3 and TIMP-4 are expressed in certain specific cells or tissues. However, it is suggested that TIMPs are associated with the immune response and NO is generated by immune cells as part of the human immune response. While periodontitis and DM exhibit impaired immune processes, no study has yet reported on the expression of iNOS, TIMP-3, or TIMP-4 in human gingival tissues. Therefore, the purpose of this study is to analyze the expression of iNOS, TIMP-3, and TIMP-4 in the gingival tissues of periodontal patients with or without type 2 DM.
Samples were obtained from patients undergoing periodontal surgery or extraction and comprised junctional and crevicular epithelium and connective tissue. The samples included 16 cases diagnosed as periodontally healthy (group 1), 16 cases with chronic moderate periodontitis (group 2), and 16 cases with chronic moderate periodontitis with DM (group 3). The patients of group 1 and group 2 were systemically healthy. This study was approved by the Ethical Committee of Clinical Experiments, Kyungpook National University Hospital (No. 74005-418).
The diagnosis of chronic periodontitis was established on the basis of clinical and radiographic criteria. The patients with chronic periodontitis had more than one periodontal pocket with a depth of ≥5 mm, with at least one pocket having ≥5 mm loss of attachment and all gingival samples were obtained from the teeth with a probing depth of ≥5 mm, swelling of the marginal gingiva, and bleeding corresponding to gingival sulcus bleeding indexes above 3 according to Muhlemann and Son [10]. The patients in group 3 were diagnosed with diabetes when their fasting plasma glucose exceeded 126 mg/dL or two-hour postprandial glucose exceeded 200 mg/dL [11]. Following surgery, excised tissue specimens were immediately placed in liquid nitrogen and subsequently frozen at -70℃.
For western blotting, frozen tissues were broken down mechanically using a homogenizer in radio immunoprecipitation assay lysis buffer (10 mM ethylenediaminetetraacetic acid, 0.15 M NaCl) with 1:30 diluted protease inhibitor cocktail (Roche, Mannheim, Germany) [12]. The lysates were centrifuged at 12,000 g for 15 minutes at 4℃. Protein concentrations of supernatant liquid were quantitatively analyzed by a Bradford protein assay (Quick Start, Bio-Rad Laboratories Inc., Hercules, CA, USA) using bovine serum albumin as a standard.
The lysates were boiled for 3 minutes in sodium dodecyl sulfate (SDS) sample buffer (1 M Tris-Cl [pH 6.8], 40% glycerol, 8% SDS, 2% mercaptoethanol, 0.002% bromophenol blue). The prepared samples were separated by 15% SDS-polyacrylamide gels using gel electrophoresis, which maintains the polypeptides in a denatured state, and were transferred to a polyvinylidene diflouride membrane to make the proteins accessible to antibody detection.
Blocking of the membranes was subsequently achieved in Tris-buffered saline (TBS) with a minute percentage of detergent such as Tween 20 containing 5% powdered milk for 1 hour. The membranes were then incubated with polyclonal anti-iNOS antibody and anti-TIMP-3 and anti-TIMP-4 antibodies (diluted 1:1,000 in TBS, Santa Cruz Biotechnology Inc., Santa Cruz, CA, USA) for 1.5 hours at room temperature.
The membranes were washed in TBS with Tween 20 three times for 10 minutes and incubated with a horseradish peroxidase linked goat antirabbit secondary antibody for anti-iNOS antibody, anti-TIMP-3 and anti-TIMP-4 antibodies (diluted 1: 2,000 in TBS) for 1 hour at room temperature. After that, rinsing was performed three times for 10 minutes with Tween 20. The membranes were developed with an ECL Plus development kit (Amsterdam, Beckinghamshire, UK).
The quantitative analysis of iNOS, TIMP-3, and TIMP-4 expression and β-actin (Abcam plc, Cambridge, UK) was performed using a densitometer (Image Gauge V 3.46, Koshin Graphic Systems, Fuji Photo Film Co., Tokyo, Japan). After normalization in each sample, the relative levels of iNOS, TIMP-3, and TIMP-4 were expressed as a ratio of iNOS, TIMP-3, and TIMP-4/β-actin, and the differences among the groups were compared.
All data were presented as mean±standard deviation and the results were statistically analyzed. The iNOS, TIMP-3, and TIMP-4 levels were compared using one way analysis of variance and the Kruskal-Wallis test followed by Tukey's and Dunnett's tests. A P-value<0.05 was considered to be statistically significant.
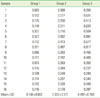
The gingival tissue from the patients of the normally healthy group, chronic periodontitis group, and chronic periodontitis with type 2 DM group showed the expression of iNOS corresponding to a molecular weight of 130 kDa in all samples. One representative band of iNOS is shown in Fig. 1. The expression levels of iNOS were increased in group 1, group 2, and group 3 in increasing order. The quantification of iNOS expression is shown in Table 1 and summarized as a graph in Fig. 2. The quantification of the density and areas of the expressed iNOS band in all three groups is performed using a densitometer. The mean normalized value of iNOS expression relative to its β-actin value was 0.107±0.091 in group 1, 0.504±0.166 in group 2, and 0.604±0.234 in group 3. More increased iNOS levels were observed in group 2 than group 1, in group 3 than group 1, and in group 3 than group 2. There were statistically significant differences both between group 1 and group 2 and between group 1 and group 3 (P<0.05). However, there was no significant difference between group 2 and group 3.
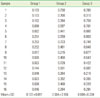
The gingival tissue from the patients of the normally healthy group, chronic periodontitis group, and chronic periodontitis with type 2 DM group showed the expression of TIMP-3 corresponding to a molecular weight of 21 kDa in all of the samples. One representative band of TIMP-3 is shown in Fig. 3. The expression levels of TIMP-3 were increased in group 1, group 2 and group 3 in increasing order. The quantification of TIMP-3 expression is shown in Table 2 and summarized as a graph in Fig. 4. The quantification of the density and areas of the expressed TIMP-3 band in all three groups was performed using a densitometer. The mean normalized value of TIMP-3 expression relative to its β-actin was 0.103±0.060 in group 1, 0.261±0.104 in group 2, and 0.375±0.153 in group 3. More increased TIMP-3 levels were observed in group 2 than group 1, in group 3 than group 1, and in group 3 than group 2. There was a significant difference both between group 1 and group 2 and between group 1 and group 3 (P<0.05). However, there were no significant differences between group 2 and group 3.
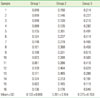
The gingival tissue from the patients of the normally healthy group, chronic periodontitis group, and chronic periodontitis with type 2 DM group showed TIMP-4 expression corresponding to a molecular weight of 21 kDa in all of the samples. One representative band of TIMP-4 is shown in Fig. 5. The expression levels of TIMP-4 were increased in group 1, group 2, and group 3 in increasing order. The quantification of TIMP-4 expression is shown in Table 3 and summarized as a graph in Fig. 6. The quantification of the density and areas of the expressed TIMP-4 band in all three groups is performed using a densitometer. The mean normalized value of TIMP-4 expression relative to its β-actin value was 0.168±0.082 in group 1, 0.333±0.1071 in group 2, and 0.497±0.193 in group 3. More increased TIMP-4 levels were observed in group 2 than group 1, in group 3 than group 1, and in group 3 than group 2. All of the groups showed significant differences from each other (P<0.05).
In periodontitis, bacteria activate the host immune system and inflammatory mediators continuously cause tissue destruction. Alveolar bone loss results from tissue destruction, and although various cytokines and mediators are concerned in these processes, the interactions are still obscure.
The activation of iNOS generates a large amount of NO for a long period, and this process is concerned with the immune reactions in various inflammatory diseases [13]. NO production, which is induced by iNOS, is important for antimicrobial activity in defense mechanisms [14,15], but at the same time it plays a role in periodontitis and tissue destruction. In some studies, a large amount of NO has been shown to inhibit osteoblastic or osteoclastic activity in inflammatory diseases involved with cytokines [16,17], so these processes are not linear but very complex. It has been shown that inhibition of iNOS reduced the bone destruction in an experimental periodontal animal model [18,19], and the number of iNOS positive cells is more elevated in tissues with periodontal disease than in clinically normal gingival tissues. However, Lin et al. [20] reported that macrophages synthesizing iNOS were distributed in the osteolytic area and NO might aggravate bone loss by modulating MMP-1 synthesis. Alayan et al. [21] reported that a lack of alveolar bone resorption was seen in infected animals due to high concentrations of NO after iNOS induction by Porphyromonas gingivalis LPS with its inhibitory effects on osteoclasts. They suggested the difference in the study design, which was the observation period and the method of alveolar bone loss measurement, to be a potential cause of the conflicting results.
In the present study, immunoblotting analysis of human periodontal diseases showed a significant increase in the expression of iNOS in group 2 in relation to clinically healthy group 1. Group 3 with DM and chronic periodontitis showed higher expression of iNOS than group 2 with periodontitis only, but did not show a significant result. Hence, it seemed that iNOS expression did not play a major role in the increased severity of periodontitis in patients with DM. Since group 2 and group 3 had clinically moderate periodontal status, it was thought that the level of iNOS expression did not differ significantly. However, there have been reports of an increased level of proinflammatory markers such as TNF-α, NO, and the increased induction of iNOS expression in other organs in humans with type 2 DM [22-24]. Furthermore, Kashyap et al. [25] reported that impaired NOS activity may play an important role in the insulin resistance in type 2 DM patients. As appeared in the results of the present study, it was obvious that the level of iNOS expression was increased based on the source of infection in the inflammatory periodontium of healthy patients and diabetic patients. These results corresponded with other previous reports that compared periodontal tissue with clinically healthy tissue [3,26]. It could be attributed to the increased expression of nitrosative stress that greater severity of periodontitis was generally observed in diabetic patients than in medically healthy patients regardless of the presence of similar local factors such as plaque deposition, teeth arrangement, occlusal relationship, and similar genetic traits. Although the increased level of iNOS expression in diabetic periodontal patients did not show a significant result, it was thought that the patients of group 2 and group 3 had similar periodontal conditions and the diabetic patients of group 3 might express a similar periodontal status despite a decrease in local or genetic factors due to increased nitrosative factors. Because only the result of tissue destruction might be reflected in this experiment, a further longitudinal study was required on the duration of inflammation, amount of NO, and time at which the tissue destruction occurs.
Nishikawa et al. [27] also proposed a scheme for the involvement of nitrosative stress and TNF-α in periodontitis under diabetic conditions. They suggested that the increased expression of TNF-α in diabetic conditions directly triggered aggravation of periodontal disease and indirectly caused aggravation of periodontal disease by stimulation of iNOS expression. TNF-α is produced chiefly by activated macrophages, although it can be produced by other cell types as well, such as CD4+ lymphocytes and NK cells. Macrophages can be activated by TNF-α to produce NO, which is derived by iNOS enzymes, and polymorphonuclear neutrophil leukocytes also can release NO and other reactive oxygen species [28]. Increased expression of TNF-α under diabetic conditions may stimulate iNOS expression whereas polymorphonuclear neutrophil leukocytes deficiency under the diabetic condition may reduce the protective function by decreased iNOS production. These relationships may also explain the difference between group 2 and group 3.
Therefore, further study may be required to develop a model to analyze the severity of disease and expression of inflammatory mediators in diseased sites in which inhibitors of iNOS and/or TNF-α are applied, especially in diabetic patients.
ECM is the extracellular part of human tissue. MMPs are able to degrade all kinds of ECM proteins, and the role of MMPs is also important for controlled remodeling of the ECM in periodontal disease. TIMPs basically bind to MMPs and the activation of MMPs is regulated by TIMPs, which are a specific group of endogenous proteins. Thus, the balance between MMPs and TIMPs may maintain tissue remodeling and metabolism. It is the increase of certain mediators under inflammatory conditions that causes disequilibration, resulting in periodontal destruction.
Garlet et al. [29] reported that the gingival tissues from the patients of chronic or aggressive periodontitis showed a stronger mRNA expression of TIMP-1, TIMP-2, and TIMP-3 than those from periodontally healthy patients, and TIMP-3 and TIMP-1 expression was more intense in chronic periodontitis than in aggressive periodontitis. Another study reported that TIMP-3 mRNA levels were similar in diseased and healthy gingival tissues, and the gene expression level of TIMP-4 was significantly higher in periodontitis-affected tissues than in normal gingival tissues [30]. They emphasized the correlation between TIMP-3 and TNF-α converting enzyme (TACE) and suggested that TIMP-4 gene expression was considered an adaptive phenomenon to react to periodontal destruction of ECMs by MMPs. Also, Nakasone et al. [31] reported that inflammatory cells, including lymphocytes, plasma cells, and macrophages, expressed faint expression for TIMP-3 in inflammatory tissues, but TIMP-4 was up-regulated by inflammation. Meanwhile, Claudino et al. [32] reported that TIMP-3 mRNA was found to be higher in diseased gingival tissues than in healthy ones and suggested that TIMPs effectively counteracted MMPs and were associated with the attenuation of disease severity.
In our study, the expressions of TIMP-3 and TIMP-4 were higher in group 2 than in group 1. In other words, TIMP-3 and TIMP-4 levels in diseased sites were higher than in healthy sites. It is thought that the level of TIMPs adjusts to maintain a balance with the increased level of MMPs induced in the inflammatory response, and TIMP-3 and TIMP-4 might also be regulators of inflammatory cytokines. Typical well known mediators such as TNF-α and IL-1β trigger tissue destruction by generating proteases among which MMPs are the most important [33], while TIMPs are the principal inhibitors. As periodontitis is generally a type of chronic disease, the process of periodontitis has a progressive period and resting period, and most tissue destruction occurs during the progressive period. It is thought that during this period, the activity of MMPs is prominent, and TIMPs can increase accordingly. Garlet et al. [34] reported that increased levels of IL-4 and IL-10 were correlated with a higher expression of TIMPs and osteoprotegerin (OPG). Claudino et al. [32] reported that the anti-inflammatory cytokine IL-10 induced the expression of TIMPs and OPG, which were inhibitors of MMPs and receptor activator of nuclear factor kappa-B ligand systems, respectively. It has been reported that IL-4, IL-10, and OPG serve to inhibit bone resorption in periodontal disease [35]. Consequently, TIMPs seem to be regarded as favorable stimulators in the pathogenesis of periodontal disease.
Interestingly, the levels of TIMP-3 in group 2 and group 3 did differ significantly. TIMP-3 was found to be a strong inhibitor of TACE among other TIMPs [36] and TACE. Diabetic conditions can increase the expression of markers of systemic inflammation and Monroy et al. [37] showed that insulin-resistant conditions were associated with the increased level of TACE activity and such conditions were correlated with the down-regulation of TIMP-3 in human skeletal muscle. They suggested that the down-regulation of TIMP-3 leads to an increased level of TACE. It can also increase the TNF-α effect, resulting in the increased severity of the inflammatory process. Cardellini et al. [38] suggested that metabolic-dependent reduction of TIMP-3 expression might increase the activity of inflammatory enzymes, which play a role in atherothrombosis. It is thought that since group 3 is under both inflammatory and diabetic conditions, group 1 and group 2 showed a significant difference while group 2 and group 3 did not. Therefore, the altered TIMP-3 level associated with TACE in periodontitis accompanied by DM might explain periodontal severity.
Koskivirta et al. [39] reported that T lymphocytes and monocytes/macrophages produced TIMP-4 in human cultured cells and TIMP-4 was immunohistochemically localized to inflammatory cells in human cardiovascular structures, mainly macrophages and CD3+ T lymphocytes. They also mentioned that higher blood pressure of coronary arteries probably stimulated MMP expression, thereby increasing TIMP-4 expression to inhibit inappropriate remodeling of the arterial wall. In diabetic conditions in which neutrophils are inefficient in their microbial response, macrophages and lymphocytes form a greater part of the immune response, and it is thought that induced MMP secretion by monocytes/macrophages constitutively increases TIMP-4 production. TIMP-4 is a highly regulated inflammatory mediator and modulator of immune response under diabetic condition.
In conclusion, this study demonstrated that iNOS, TIMP-3, and TIMP-4 might be involved in the progression of periodontal inflammation associated with type 2 DM. Although mechanical and chemical therapeutic strategies for the treatment of periodontitis are known, the application of molecular biology to understanding inflammatory and metabolic disease is under ongoing study. Therefore, it is thought that further study of these factors can be applied practically for the diagnosis and control of periodontitis in diabetics.
Figures and Tables
Figure 1
Pattern of inducible nitric oxide synthases (iNOS) expression of 4 representative samples in western blot analysis. The expression levels of iNOS were normalized to β-actin in all individuals from each group. Group 1: healthy periodontal tissue from systemically healthy patient, Group 2: diseased periodontal tissue from patient with chronic periodontitis, Group 3: diseased periodontal tissue from patient with chronic periodontitis and diabetes mellitus.

Figure 2
Graph showing average amounts and standard deviation (ratio of inducible nitric oxide synthases [iNOS]/β-actin) in groups 1, 2, and 3. The levels of iNOS of the diseased gingiva were higher than those of healthy gingiva. a)Significant difference between group 1 and group 2 (P<0.05). b)Significant difference between group 1 and group 3 (P<0.05).

Figure 3
Pattern of tissue inhibitors of metalloproteinase (TIMP)-3 expression of 4 representative samples in western blot analysis. The expression levels of TIMP-3 were normalized to β-actin in all individuals from each group. Group 1: healthy periodontal tissue from systemically healthy patient, Group 2: diseased periodontal tissue from patient with chronic periodontitis, Group 3: diseased periodontal tissue from patient with chronic periodontitis and diabetes mellitus.

Figure 4
Graph showing averages and standard deviations (ratio of tissue inhibitors of metalloproteinase [TIMP]-3/β-actin) in groups 1, 2, and 3. The levels of TIMP-3 in the diseased gingiva were higher than those in the healthy gingiva. a)Significant difference between group 1 and group 2 (P<0.05). b)Significant difference between group 1 and group 3 (P<0.05).
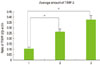
Figure 5
Pattern of tissue inhibitors of metalloproteinase (TIMP)-4 expression of 4 representative samples by western blot analysis. The expression levels of TIMP-4 were normalized to β-actin in all individuals from each group. Group 1: healthy periodontal tissue from systemically healthy patient, Group 2: diseased periodontal tissue from patient with chronic periodontitis, Group 3: diseased periodontal tissue from patient with chronic periodontitis and diabetes mellitus.

Figure 6
Graph showing averages and standard deviations (ratio of tissue inhibitors of metalloproteinase [TIMP]-4/β-actin) in groups 1, 2, and 3. The levels of TIMP-4 of the diseased gingiva were higher than those of healthy gingiva. a)Significant difference between group 1 and group 2 (P<0.05). b)Significant difference between group 1 and group 3 (P<0.05). c)Significant difference between group 2 and group 3 (P<0.05).

ACKNOWLEDGEMENTS
This research was supported by the Kyungpook National University Research Fund (2012).
References
1. Eley BM, Cox SW. Proteolytic and hydrolytic enzymes from putative periodontal pathogens: characterization, molecular genetics, effects on host defenses and tissues and detection in gingival crevice fluid. Periodontol 2000. 2003. 31:105–124.

2. Hou YC, Janczuk A, Wang PG. Current trends in the development of nitric oxide donors. Curr Pharm Des. 1999. 5:417–441.
3. Batista AC, Silva TA, Chun JH, Lara VS. Nitric oxide synthesis and severity of human periodontal disease. Oral Dis. 2002. 8:254–260.

4. Abramson SB, Amin AR, Clancy RM, Attur M. The role of nitric oxide in tissue destruction. Best Pract Res Clin Rheumatol. 2001. 15:831–845.

5. Reher VG, Zenobio EG, Costa FO, Reher P, Soares RV. Nitric oxide levels in saliva increase with severity of chronic periodontitis. J Oral Sci. 2007. 49:271–276.

6. Kendall HK, Marshall RI, Bartold PM. Nitric oxide and tissue destruction. Oral Dis. 2001. 7:2–10.

7. Bauer EA, Stricklin GP, Jeffrey JJ, Eisen AZ. Collagenase production by human skin fibroblasts. Biochem Biophys Res Commun. 1975. 64:232–240.

8. Gomez DE, Alonso DF, Yoshiji H, Thorgeirsson UP. Tissue inhibitors of metalloproteinases: structure, regulation and biological functions. Eur J Cell Biol. 1997. 74:111–122.
9. Young DA, Phillips BW, Lundy C, Nuttall RK, Hogan A, Schultz GA, et al. Identification of an initiator-like element essential for the expression of the tissue inhibitor of metalloproteinases-4 (Timp-4) gene. Biochem J. 2002. 364(Pt 1):89–99.

10. Muhlemann HR, Son S. Gingival sulcus bleeding: a leading symptom in initial gingivitis. Helv Odontol Acta. 1971. 15:107–113.
11. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003. 26:Suppl 1. S5–S20.
12. Cho JY, Xing S, Liu X, Buckwalter TL, Hwa L, Sferra TJ, et al. Expression and activity of human Na+/I- symporter in human glioma cells by adenovirus-mediated gene delivery. Gene Ther. 2000. 7:740–749.

13. Stefanovic-Racic M, Stadler J, Evans CH. Nitric oxide and arthritis. Arthritis Rheum. 1993. 36:1036–1044.

14. Allaker RP, Silva Mendez LS, Hardie JM, Benjamin N. Antimicrobial effect of acidified nitrite on periodontal bacteria. Oral Microbiol Immunol. 2001. 16:253–256.

15. Gyurko R, Boustany G, Huang PL, Kantarci A, Van Dyke TE, Genco CA, et al. Mice lacking inducible nitric oxide synthase demonstrate impaired killing of Porphyromonas gingivalis. Infect Immun. 2003. 71:4917–4924.

16. Ralston SH, Todd D, Helfrich M, Benjamin N, Grabowski PS. Human osteoblast-like cells produce nitric oxide and express inducible nitric oxide synthase. Endocrinology. 1994. 135:330–336.

17. van't Hof RJ, Ralston SH. Cytokine-induced nitric oxide inhibits bone resorption by inducing apoptosis of osteoclast progenitors and suppressing osteoclast activity. J Bone Miner Res. 1997. 12:1797–1804.
18. Lohinai Z, Benedek P, Feher E, Gyorfi A, Rosivall L, Fazekas A, et al. Protective effects of mercaptoethylguanidine, a selective inhibitor of inducible nitric oxide synthase, in ligature-induced periodontitis in the rat. Br J Pharmacol. 1998. 123:353–360.

19. Leitão RF, Ribeiro RA, Chaves HV, Rocha FA, Lima V, Brito GA. Nitric oxide synthase inhibition prevents alveolar bone resorption in experimental periodontitis in rats. J Periodontol. 2005. 76:956–963.

20. Lin SK, Kok SH, Kuo MY, Lee MS, Wang CC, Lan WH, et al. Nitric oxide promotes infectious bone resorption by enhancing cytokine-stimulated interstitial collagenase synthesis in osteoblasts. J Bone Miner Res. 2003. 18:39–46.

21. Alayan J, Ivanovski S, Gemmell E, Ford P, Hamlet S, Farah CS. Deficiency of iNOS contributes to Porphyromonas gingivalis-induced tissue damage. Oral Microbiol Immunol. 2006. 21:360–365.

22. Takahashi Y, Nakano T, Wakabayashi I. Increased induction of inducible nitric oxide synthase expression in aortae of type 2 diabetes rats. J Pharmacol Sci. 2008. 107:190–200.

23. Pereira FO, Frode TS, Medeiros YS. Evaluation of tumour necrosis factor alpha, interleukin-2 soluble receptor, nitric oxide metabolites, and lipids as inflammatory markers in type 2 diabetes mellitus. Mediators Inflamm. 2006. 2006:39062.

24. Nagareddy PR, McNeill JH, MacLeod KM. Chronic inhibition of inducible nitric oxide synthase ameliorates cardiovascular abnormalities in streptozotocin diabetic rats. Eur J Pharmacol. 2009. 611:53–59.

25. Kashyap SR, Roman LJ, Lamont J, Masters BS, Bajaj M, Suraamornkul S, et al. Insulin resistance is associated with impaired nitric oxide synthase activity in skeletal muscle of type 2 diabetic subjects. J Clin Endocrinol Metab. 2005. 90:1100–1105.

26. Lappin DF, Kjeldsen M, Sander L, Kinane DF. Inducible nitric oxide synthase expression in periodontitis. J Periodontal Res. 2000. 35:369–373.

27. Nishikawa T, Naruse K, Kobayashi Y, Miyajima S, Mizutani M, Kikuchi T, et al. Involvement of nitrosative stress in experimental periodontitis in diabetic rats. J Clin Periodontol. 2012. 39:342–349.

28. Garlet GP, Cardoso CR, Campanelli AP, Ferreira BR, Avila-Campos MJ, Cunha FQ, et al. The dual role of p55 tumour necrosis factor-alpha receptor in Actinobacillus actinomycetemcomitans-induced experimental periodontitis: host protection and tissue destruction. Clin Exp Immunol. 2007. 147:128–138.

29. Garlet GP, Martins W Jr, Fonseca BA, Ferreira BR, Silva JS. Matrix metalloproteinases, their physiological inhibitors and osteoclast factors are differentially regulated by the cytokine profile in human periodontal disease. J Clin Periodontol. 2004. 31:671–679.

30. Kubota T, Itagaki M, Hoshino C, Nagata M, Morozumi T, Kobayashi T, et al. Altered gene expression levels of matrix metalloproteinases and their inhibitors in periodontitis-affected gingival tissue. J Periodontol. 2008. 79:166–173.

31. Nakasone N, Kubota T, Hoshino C, Nohno K, Itagaki M, Shimizu T, et al. Differential gene and protein expression of tissue inhibitors of metalloproteinases (TIMP)-3 and TIMP-4 in gingival tissues from drug induced gingival overgrowth. Arch Oral Biol. 2009. 54:634–641.

32. Claudino M, Trombone AP, Cardoso CR, Ferreira SB Jr, Martins W Jr, Assis GF, et al. The broad effects of the functional IL-10 promoter-592 polymorphism: modulation of IL-10, TIMP-3, and OPG expression and their association with periodontal disease outcome. J Leukoc Biol. 2008. 84:1565–1573.

34. Garlet GP, Cardoso CR, Silva TA, Ferreira BR, Avila-Campos MJ, Cunha FQ, et al. Cytokine pattern determines the progression of experimental periodontal disease induced by Actinobacillus actinomycetemcomitans through the modulation of MMPs, RANKL, and their physiological inhibitors. Oral Microbiol Immunol. 2006. 21:12–20.

35. Cochran DL. Inflammation and bone loss in periodontal disease. J Periodontol. 2008. 79:8 Suppl. 1569–1576.

36. Amour A, Slocombe PM, Webster A, Butler M, Knight CG, Smith BJ, et al. TNF-alpha converting enzyme (TACE) is inhibited by TIMP-3. FEBS Lett. 1998. 435:39–44.
37. Monroy A, Kamath S, Chavez AO, Centonze VE, Veerasamy M, Barrentine A, et al. Impaired regulation of the TNF-alpha converting enzyme/tissue inhibitor of metalloproteinase 3 proteolytic system in skeletal muscle of obese type 2 diabetic patients: a new mechanism of insulin resistance in humans. Diabetologia. 2009. 52:2169–2181.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download