Abstract
Purpose
The aim of this study was to measure the peri-implant bone length surrounding implants that penetrate the sinus membrane at the posterior maxilla and to evaluate the survival rate of these implants.
Methods
Treatment records and orthopantomographs of 39 patients were reviewed and analyzed. The patients had partial edentulism at the posterior maxilla and limited vertical bone height below the maxillary sinus. Implants were inserted into the posterior maxilla, penetrating the sinus membrane. Four months after implant insertion, provisional resin restorations were temporarily cemented to the abutments and used for one month. Then, a final impression was taken at the abutment level, and final cement-retained restorations were delivered with mutually protected occlusion. The complications from the implant surgery were examined, the number of failed implants was counted, and the survival rate was calculated. The peri-implant bone lengths were measured using radiographs. The changes in initial and final peri-implant bone lengths were statistically analyzed.
Results
Nasal bleeding occurred after implant surgery in three patients. No other complications were found. There were no failures of the investigated implants, resulting in a survival rate of 100%. Significantly more bone gain around the implants (estimated difference=-0.6 mm, P=0.025) occurred when the initial residual bone height was less than 5 mm compared to the >5 mm groups. No significant change in peri-implant bone length was detected when the initial residual bone height was 5 mm or larger.
Implant-supported restoration at the edentulous posterior maxilla is often difficult because of insufficient bone volume [1,2]. The gold standard implant operation involves inserting implants into sinuses augmented by autogenous bone [1,3]. This operation and other substitutes have exhibited good implant survival; however, a recent meta-analysis estimated an annual implant failure rate of 3.5% [4,5]. That is, the three-year implant survival rate was 90.1% at the elevated sinuses [5]. This survival rate is lower than the general implant survival rate of over 95%. Furthermore, considering the variables of cost, healing time, and complications like postoperative pain, swelling, and graft failure, selecting an augmentation procedure may be complicated [3,4,6].
Short implants have been suggested as an alternative to sinus lift procedures [1-3,7-9]. Some randomized controlled trials have indicated that short implants of about 5 or 6 mm in length have comparable survival to longer implants inserted in augmented maxillary sinuses [2,7-9]. Unfortunately, these studies were limited by short observation periods of less than one year. Advantages of short implants over longer implants requiring sinus floor elevation include a less technically demanding operation, lower expense, fewer surgical procedures, and fewer complications [1,3]. Despite these advantages, perforation of the sinus membrane at the posterior maxilla is often unavoidable even with short 5 mm implants and a residual bone height of 3 mm, which is generally needed to stabilize the implant [10].
Membrane perforation is the most frequent complication of sinus floor elevation [5]. Previous studies have suggested that sinus membrane perforation has a negative effect on implant survival; however, other authors discovered no difference in implant survival [11-17]. Dentists and patients would have an easier and more comfortable way of restoring function at the posterior maxilla if implants penetrating the Schneiderian membrane were to show comparable survival results to those installed in augmented sinuses. Unfortunately, there has been no study evaluating such treatment options.
This retrospective study evaluated the survival rate of implants penetrating the sinus membrane at the posterior maxilla, measured the peri-implant bone length, and surveyed the complications from the penetrating implant surgery.
Treatment records and orthopantomographs of the selected patients were reviewed and analyzed in this retrospective study, which was approved by the Institutional Review Board of Seoul National University School of Dentistry (No. S-D20120022). The total number of patients in the sample was 39 (26 males and 13 females) ranging in age from 21 to 80 years (mean age, 60.0±12.4 years). The patients had partial edentulism at the posterior maxilla (premolars and molars) with limited vertical bone height below the maxillary sinus, requiring one to three dental implants. The 39 patients were treated in a private practice between October 2007 and November 2011. One experienced surgeon performed all of the operations, including implant surgery and prosthodontic procedures. Patients with at least 5 mm of bone width at the implant sites were included in this study, while those with a condition that generally contraindicated implant surgery, such as uncontrolled diabetes, pregnancy, history of radiation therapy in the head and neck region, a heavy smoking habit, or severe periodontitis were excluded.
After Betadine application at the implant sites and infiltration anesthesia (2% lidocaine with epinephrine 1:100,000), crestal incision was performed, and the flap was elevated. Screw-shaped implants with microthreads and tapered tops (Deep Implant System Inc., Seoul, Korea) were used in this study. The implants, which were 1 to 5 mm longer than the vertical bone height below the maxillary sinus, were inserted into the posterior maxilla, penetrating the sinus membrane. The final drill diameter was 0.3 mm smaller than that of the installed implants. The implants were placed 0.5 mm supracrestally to prevent the fixtures from sinking into the sinuses (Fig. 1). Cover screws were connected with the implant fixtures, and the flaps were sutured. After four months, the implants were exposed, and the abutments were connected with 25 Ncm tightening torque according to the manufacturer's recommendations. All of the implants used in this study had an internal connection design that stabilized the abutment with an abutment screw and friction between the abutment and implant fixture (Fig. 1). Provisional resin restorations were temporarily cemented to the abutments and used for one month. After one month, the provisional restorations were removed, and the abutments were retightened with the recommended torque of 25 Ncm. A final impression was taken at the abutment level using an impression cap and a polyvinylsiloxane material (Examix, GC Co., Tokyo, Japan). The final gold or metal-ceramic cement-retained restorations were delivered with occlusal contacts in centric and without eccentric contacts (mutually protected occlusion).
This study included only patients who received such an implant restoration procedure and had orthopantomographs taken from the time of surgery and at the last follow-up. Complications from the implant operation were identified from patients' treatment records. The number of failed implants was counted, and the survival rate was calculated. The peri-implant bone length, which was defined in this investigation as the vertical bone height of the bone surrounding the inserted implant below the maxillary sinus, was measured using the orthopantomographs and a proportional expression shown in Fig. 2.
Descriptive statistics were expressed as a frequency and percentage, and mean and standard deviation, as appropriate. As part of a bivariate analysis, differences between the initial and final peri-implant bone length were analyzed using a paired t-test according to three groups of initial bone lengths (2.7 to 4.99 mm / 5 to 7.99 mm / ≥8.0 mm).
A generalized linear mixed model was applied to assess the association of factors related to the change in peri-implant bone length determined by multiple observations of each patient. The mixed procedure with compound symmetric covariance structure in the SAS statistical software was used for this purpose [18]. The final model included all of the measurements: three groups of initial bone lengths, type of teeth (premolar/molar), diameter and length of implants, position in the dental arch (right/left), usage of the implant (single crown/splint), and length of the follow-up period. The statistical software SAS ver. 9.3 (SAS Institute Inc., Cary, NC, USA) was used for the analysis, and a type-one error rate of 0.05 was applied to determine the statistical significance.
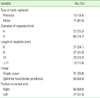
The general features of 87 implants from 39 patients are described in Table 1. The mean number of implants per patient was 2.4 (standard deviation [SD], 1.3) with a range of 1 to 6. Implants with a 4 mm (25.3%) or 5 mm (74.4%) diameter and with an 8 mm or longer length were placed at the site of premolars (18.4%) or molars (81.6%), positioned in either the right (69%) or left side (31%) of the dental arch. The mean follow-up period was 17.9 months (SD, 10.8 months), and the bone length at the time of implant placement ranged from 2.63 mm to 11.32 mm, with a mean of 6.99 mm (SD, 2.08 mm) (Table 2). None of the investigated implants failed; thus, the survival rate was 100%. Three patients experienced nasal bleeding after implant surgery (7.7%). There were no other complications such as postoperative pain or swelling.
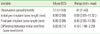
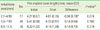
The mean peri-implant bone length at final follow-up was 6.95 mm (SD, 2.06 mm), and the mean difference between the initial and final bone lengths was 0.05 mm (SD, 0.71 mm) (Table 2). A paired t-test revealed a marginally significant gain in bone length (estimate of bone loss=-0.34 mm, P=0.074) after implant placement at sites in the smallest initial bone length group (2.7 to 4.99 mm), and no significant differences in bone length were observed in the other groups (Table 3). According to the generalized linear mixed model, the change in the bone length in the 2.7 to 4.99 mm group was significantly different from the other groups (P=0.025) after adjustment for multiple observations, positions of teeth, and other related factors (Table 4). The smallest initial bone length group (2.7 to 4.99 mm group) showed bone length changes significantly different than those of the two larger initial bone length groups (parameter estimate=-0.60 mm, P=0.025), and the premolar group had larger differences compared to the molar group (estimate=0.45 mm, P=0.029). Other factors, including the diameter and length of implants, position in the dental arch (right/left), usage of the implant (single crown/splint), and length of the follow-up period, were not associated with the change in bone length (P>0.05).
The results of this study carry some important implications. First, all of the perforated cases survived with almost no complications during the follow-up period, which is a better or equivalent result compared to previous reports [4,15]. These results suggest that patients with limited bone height at the posterior maxilla may be safely treated with implant placement that penetrates the sinus membrane. The results also imply that such an implant insertion technique may be more desirable for patients than implant placement plus sinus floor elevation due to a less technically demanding operation, lower expense, fewer surgical procedures, and fewer complications. This retrospective study has a basic limitation of a lower level of evidence than prospective cohort studies. Irregular follow-up periods ranging from 2 to 43 months and a small sample size may also be limitations. Further studies with a detailed prospective design based on a larger sample are required to obtain stronger evidence.
Second, the possible gain in peri-implant bone length (estimated mean bone loss=-0.34 mm, P=0.074) in the group with 2.7 to 4.99 mm initial bone lengths was observed. Furthermore, a significant difference in bone length change was found between the smallest initial bone length group and the two larger groups (estimated difference=-0.60 mm, P=0.025). The two larger groups had insignificant loss of bone length (estimated mean bone loss=0.14 mm, P>0.05). A bone modeling and remodeling mechanism by microstrain can explain the results of this study [19]. Bone strain that ranges between 1,500 and 3,000 microstrains induces bone formation while strain between 50 and 1,500 microstrains results in equal amounts of bone formation and resorption [19]. Patients with posterior maxillary bone vertical height less than 5 mm are thought to experience 1,500 to 3,000 microstrains under its occlusal load, which likely caused the bone gain seen in this study. Conversely, posterior maxillary bone with a vertical height of 5 mm or larger may be too thick to face the microstrain needed for bone formation. Further studies are needed to clarify the relationship between bone microstrain and bone response at the posterior maxilla under its occlusal load.
Considering the bone length measured in this study, almost no decrease in the marginal bone level was found around the investigated implants. According to Karabuda et al. [15], the mean marginal bone resorption was larger than the result in this study. The previous study investigated the resorption of the marginal bone surrounding implants with different designs than those used in this study [15]. Implant design may affect implant survival when placed at the posterior maxilla with limited vertical bone height and low bone quality. Microthreads appear to be necessary to ensure more threads are engaged with the bone. A tapered design at the bone crestal area seems to prevent sinking of the implant into the maxillary sinus under the occlusal load. The connection between a fixture and an abutment using screw and friction mechanics has a large effect on force distribution to the surrounding bone [20,21]. Further studies are required to compare implant designs and their influence on survival of the implants inserted into bone of limited quantity and quality.
In conclusion, this retrospective study suggests that implants penetrating the maxillary sinus membrane may be functional under an occlusal load at the posterior maxilla with limited vertical bone height. Although long-term prospective and randomized controlled studies are needed, patients with atrophic posterior maxillae below maxillary sinuses may be safely and easily treated with implant placement that pierces the membrane, a procedure which has the advantages of being less technically demanding, requiring fewer surgical procedures, and resulting in fewer complications.
Figures and Tables
Figure 1
A schematic diagram of implant surgery. The black arrow-heads indicate the Schneiderian membrane, and the white arrowheads represent the periosteum. Note that the inserted implants have penetrated the sinus membrane, leaving the apical portion in the maxillary sinus. The top of the implant was positioned about 0.5 mm supracrestally. The cross-sectioned diagram of the implant at the second molar area shows the screw- and friction-retained connection at the interface between the fixture and abutment.

Figure 2
A radiograph and schematic diagram of the method for measuring peri-implant bone length. The bottom portions of the inserted implants (black arrowheads) are observed in the maxillary sinus on this radiograph (A). The white arrowheads indicate the inferior border of the maxillary sinus. Magnified ratios had to be considered for measurements on the radiographs because they were orthopantomographic images. The real bone length was calculated as follows (B). m, d, and f on the schematic figure indicate the measured lengths on the orthopantomograph. M and D are the real lengths that we want to know, and F is the real length of the inserted implant that is already known. The bone lengths of the mesial and distal sides are calculated through the following proportional expressions: f:F=m:M and f:F=d:D. The peri-implant bone length was a mean value of the mesial and distal bone lengths around the implant; that is, L (peri-implant bone length)=(M+D)/2.

ACKNOWLEDGEMENTS
This work was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (No. 2011-0007662).
References
1. Esposito M, Grusovin MG, Rees J, Karasoulos D, Felice P, Alissa R, et al. Effectiveness of sinus lift procedures for dental implant rehabilitation: a Cochrane systematic review. Eur J Oral Implantol. 2010. 3:7–26.
2. Esposito M, Pellegrino G, Pistilli R, Felice P. Rehabilitation of postrior atrophic edentulous jaws: prostheses supported by 5 mm short implants or by longer implants in augmented bone? One-year results from a pilot randomised clinical trial. Eur J Oral Implantol. 2011. 4:21–30.
3. Felice P, Soardi E, Pellegrino G, Pistilli R, Marchetti C, Gessaroli M, et al. Treatment of the atrophic edentulous maxilla: short implants versus bone augmentation for placing longer implants: five-month post-loading results of a pilot randomised controlled trial. Eur J Oral Implantol. 2011. 4:191–202.
4. Nkenke E, Stelzle F. Clinical outcomes of sinus floor augmentation for implant placement using autogenous bone or bone substitutes: a systematic review. Clin Oral Implants Res. 2009. 20:Suppl 4. 124–133.

5. Pjetursson BE, Tan WC, Zwahlen M, Lang NP. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol. 2008. 35:8 Suppl. 216–240.

6. Esposito M, Grusovin MG, Rees J, Karasoulos D, Felice P, Alissa R, et al. Interventions for replacing missing teeth: augmentation procedures of the maxillary sinus. Cochrane Database Syst Rev. 2010. (3):CD008397.

7. Felice P, Pistilli R, Piattelli M, Soardi E, Corvino V, Esposito M. Posterior atrophic jaws rehabilitated with prostheses supported by 5×5 mm implants with a novel nanostructured calcium-incorporated titanium surface or by longer implants in augmented bone. Preliminary results from a randomised controlled trial. Eur J Oral Implantol. 2012. 5:149–161.
8. Felice P, Checchi V, Pistilli R, Scarano A, Pellegrino G, Esposito M. Bone augmentation versus 5-mm dental implants in posterior atrophic jaws. Four-month post-loading results from a randomised controlled clinical trial. Eur J Oral Implantol. 2009. 2:267–281.
9. Esposito M, Cannizzaro G, Soardi E, Pistilli R, Piattelli M, Corvino V, et al. Posterior atrophic jaws rehabilitated with prostheses supported by 6 mm-long, 4 mm-wide implants or by longer implants in augmented bone. Preliminary results from a pilot randomised controlled trial. Eur J Oral Implantol. 2012. 5:19–33.
10. Cosci F, Luccioli M. A new sinus lift technique in conjunction with placement of 265 implants: a 6-year retrospective study. Implant Dent. 2000. 9:363–368.

11. Khoury F. Augmentation of the sinus floor with mandibular bone block and simultaneous implantation: a 6-year clinical investigation. Int J Oral Maxillofac Implants. 1999. 14:557–564.
12. Proussaefs P, Lozada J, Kim J, Rohrer MD. Repair of the perforated sinus membrane with a resorbable collagen membrane: a human study. Int J Oral Maxillofac Implants. 2004. 19:413–420.
13. Vina-Almunia J, Penarrocha-Diago M, Penarrocha-Diago M. Influence of perforation of the sinus membrane on the survival rate of implants placed after direct sinus lift. Literature update. Med Oral Patol Oral Cir Bucal. 2009. 14:E133–E136.
14. Ardekian L, Oved-Peleg E, Mactei EE, Peled M. The clinical significance of sinus membrane perforation during augmentation of the maxillary sinus. J Oral Maxillofac Surg. 2006. 64:277–282.

15. Karabuda C, Arisan V, Ozyuvaci H. Effects of sinus membrane perforations on the success of dental implants placed in the augmented sinus. J Periodontol. 2006. 77:1991–1997.

16. Shlomi B, Horowitz I, Kahn A, Dobriyan A, Chaushu G. The effect of sinus membrane perforation and repair with Lambone on the outcome of maxillary sinus floor augmentation: a radiographic assessment. Int J Oral Maxillofac Implants. 2004. 19:559–562.
17. Schwartz-Arad D, Herzberg R, Dolev E. The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. J Periodontol. 2004. 75:511–516.

18. Littell RC, Milliken GA, Stroup WW, Wolfinger RD. SAS system for mixed models. 1996. Cary: SAS Institute Inc..
19. Frost HM. Wolff's law and bone's structural adaptations to mechanical usage: an overview for clinicians. Angle Orthod. 1994. 64:175–188.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download