Abstract
Purpose
The receptor activator of nuclear factor kappa B (RANK)/RANK ligand (RANKL)/osteoprotegerin (OPG) system plays a significant role in osteoclastogenesis, activation of osteoclasts, and regulation of bone resorption. This study aimed to evaluate the use of the salivary soluble RANKL (sRANKL)/OPG ratio as a diagnostic marker for periodontitis in nonsmokers.
Methods
Twenty-five patients with chronic periodontitis and 25 individuals with a healthy periodontium were enrolled in this study. Samples containing 5 mL of unstimulated saliva were obtained from each subject. Salivary sRANKL and OPG concentrations were determined using a standard enzyme-linked immunosorbent assay. Statistical analysis was performed using SPSS ver. 18.0.
Results
The levels of sRANKL and OPG were detectable in all of the samples. Positive relationships were found between the plaque index and clinical attachment level and both the salivary concentration of sRANKL and the salivary sRANKL/OPG ratio (P<0.05). The salivary concentration of sRANKL and the sRANKL/OPG ratio were significantly higher in the periodontitis group than in the healthy group (P=0.004 and P=0.001, respectively). In contrast, the OPG concentration showed no significant differences between the groups (P=0.455).
Periodontitis is an inflammatory disease that results in the loss of supporting bone in addition to mucosal inflammation [1].
In periodontics, clinical parameters such as the probing pocket depth (PPD), clinical attachment level (CAL), plaque index (PI), bleeding index (BI), and radiographic alveolar bone loss are inadequate for the detection of active diseased sites, quantitative monitoring of response to therapy, or measurement of the amount of susceptibility to disease progression in the future. A rapid and simple diagnostic test that can provide a reliable assessment of periodontal disease would be beneficial for both clinicians and patients [2].
There are many biochemical signals in affected tissues produced during the three biological phases of inflammation, destruction of connective tissue, and involvement of alveolar bone, which leads to clinical signs of the disease. These biomarkers are detectable in the gingival crevicular fluid (GCF) and whole saliva of patients with periodontitis [3].
Qualitative and quantitative changes in these biomarkers have been found useful in the diagnosis and treatment of periodontal diseases, and a combination of two or more markers may result in a more exact evaluation of patients with periodontitis [4]. However, periodontal clinical examination is necessary and cannot be substituted by any other means in periodontal diagnostics.
Compared with GCF, collection of saliva as a diagnostic fluid for analyzing oral diseases is more convenient and noninvasive, and there is a sufficient amount of saliva for assessment of biomarkers of periodontal disease and health at the subject level. Thus, saliva as a mirror of oral and systemic health is a very valuable source for finding useful information [5]. Moreover, salivary diagnostic tests can aid in screening large populations [2].
Bone resorption by osteoclasts is one of the main symptoms of periodontal diseases. Osteoclastogenesis, in particular, is controlled by three members of the tumor necrosis factor (TNF) and TNF receptor superfamily, receptor activator of nuclear factor kappa B ligand (RANKL), receptor activator of nuclear factor kappa B (RANK), and osteoprotegerin (OPG) [6]. RANKL is produced by osteoblasts and bone marrow stromal cells [7], fibroblasts [8], activated T cells, B cells [9]. Moreover, it binds directly to RANK on the surface of preosteoclasts and osteoclasts. RANKL sets up the differentiation of osteoclast progenitors and the activation of mature osteoclasts [10]. This ligand may be found in the mRANKL form, which is cell membrane-bound, or in a soluble (secreted) form, expressed by activated T cells [11].
OPG is a glycoprotein with 401 amino acids, secreted primarily by osteoblasts and bone marrow stromal cells. In addition to acting as a decoy receptor for RANKL, OPG is a competitive inhibitor of osteoclast differentiation and activity [12].
It is reported that the RANKL/OPG system plays a significant role in the pathogenesis of bone and mineral metabolism diseases, such as rheumatoid arthritis, postmenopausal osteoporosis, Paget disease, and bone malignancies, such as multiple myeloma [13]. Some studies have analyzed the concentrations of soluble RANKL (sRANKL) and OPG in the GCF of patients with periodontitis and healthy individuals. They indicated that patients with periodontitis have a higher RANKL/OPG ratio in GCF, suggesting a role for RANKL and OPG in alveolar bone destruction [14-17]. Few studies have assessed concentrations of salivary sRANKL or OPG [18-21], and to our knowledge only one study evaluated both salivary sRANKL and OPG concentrations in patients with periodontitis compared with those in healthy controls [22]. This study aimed to evaluate the use of the salivary sRANKL/OPG ratio as a diagnostic marker for periodontitis in nonsmokers.
This case-control, cross-sectional study was performed from March 2012 to April 2013 in the Department of Periodontics, College of Dentistry at Qazvin University of Medical Sciences. In this study, 25 patients with chronic periodontitis and 25 subjects with a healthy periodontium, all of whom visited the periodontology department at Qazvin University of Medical Sciences, were selected from approximately 200 subjects and enrolled in the study. The individuals completed personal, medical, and dental history questionnaires, and written consent was obtained. The study was approved by the Ethical Committee of Qazvin University of Medical Sciences (No. 576).
Inclusion criteria of the study were age over 18 years, good general health, and a minimum of 18 teeth. Exclusion criteria included history of periodontal therapy during the past 2 years; history of alcoholism and smoking; liver, kidney or salivary gland dysfunction; infectious diseases; inflammatory bowel disease; rheumatoid arthritis; granulomatous diseases; diabetes; or undergoing or having undergone organ transplant or cancer therapy. In addition, use of glucocorticoids, cyclo-oxygenase inhibitors, bisphosphonates, antibiotics or immunosuppressant medication during the past 6 months; pregnancy or lactation; need for antibiotics for infective endocarditis prophylaxis during dental procedures; acute illness symptoms (i.e., fever, sore throat, body aches, or diarrhea); orthodontic appliances; or presence of an oral mucosal inflammatory condition (e.g., aphthous stomatitis, lichen planus, leukoplakia, or oral cancer) were also considered to be exclusion criteria.
Clinical measurements were performed by an expert periodontist at 4 points per tooth using a University of North Carolina probe. The subjects of the test group had a diagnosis of generalized moderate to severe chronic periodontitis based on the criteria defined by the American Academy of Periodontology [23]. This diagnosis was established due to radiographic assessment and clinical parameters, including PI [24], PPD, CAL, and BI [25]. Periodontally diseased individuals had to have at least 5 teeth with CAL ≥3 mm and PPD >5 mm distributed among at least two quadrants.
The control group included subjects with no symptoms or history of periodontitis and no evidence of bone loss. Bleeding on probing was found in <10% of sites and all of them had a periodontal probing depth ≤3 mm.
Unstimulated whole expectorated saliva (5 mL) was collected from each subject between 10 AM and 12 PM according to a modification of the method described by Navazesh [26]. The patients were asked to swallow saliva first, and then allow the saliva to drain passively for five minutes over the lower lip into a sterile tube. The collected saliva was immediately placed on ice prior to freezing at -80℃. The samples were defrosted and analyzed within 6 months of collection.
Each saliva sample (500 µL) was pipetted into a clean microcap tube and clarified by centrifugation at 10,000 g for 5 minutes. The supernatant was transferred to clean microcap tubes and used immediately for an enzyme linked immunosorbent assay (ELISA). Concentrations of sRANKL and OPG were determined using a human sRANKL ELISA Kit (Cat.No. E0646Hu; Bioassay Technology Laboratory, Shanghai, China) and a human OPG ELISA Kit (Cat.No. E1558Hu; Bioassay Technology Laboratory) according to the manufacturer's instructions. The results of the sRANKL and OPG assays were expressed as pg/mL for concentrations. All of the laboratory tests were performed in the immunology department of Qazvin University of Medical Sciences.
Statistical analysis was performed using IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA). Demographic and clinical variables were compared among the groups using Fisher exact test. Comparisons of indices and analyses between test and control groups were performed using independent t-test and Mann-Whitney U tests. The correlations between the salivary and periodontal parameters were evaluated using Spearman correlation analysis. A P-value <0.05 was considered statistically significant.
A total of 50 participants (28 females and 22 males), aged 22 to 62 years, were enrolled in this study. There were 25 healthy subjects (11 females and 14 males, aged 24 to 50 years) and 25 patients with chronic periodontitis (14 females and 11 males, aged 22 to 62 years). The demographic and clinical characteristics and ELISA findings of the groups are shown in Table 1. As expected, all of the periodontal indices were significantly higher in the periodontitis group than in the healthy group. Pearson correlation analysis showed positive relationships between PI and both the sRANKL concentration and sRANKL/OPG ratio (P=0.008 and P=0.005, respectively). Also, positive correlations were found between the CAL and both the sRANKL concentration and sRANKL/OPG ratio (P=0.047 and P=0.015, respectively).
The salivary levels of sRANKL, OPG, and sRANKL/OPG are shown in Figs. 1-3. Soluble RANKL and OPG were detectable in all of the samples. The mean level of sRANKL was significantly higher in the periodontitis group than in the healthy subjects (P=0.004). However, in the evaluation of the OPG concentrations, no statistically significant differences were found (P=0.455). However, the sRANKL/OPG ratio was significantly higher in the periodontitis group (P=0.001).
Periodontitis is one of the most prevalent forms of oral disease. Therefore, it can be considered an important health problem related to quality of life. Currently, periodontitis is diagnosed mainly by clinical measurements and radiographic findings, which are insufficient to determine disease activity and patient susceptibility to disease progression. Biomarkers in oral fluids have the potential to provide supplementary information to the standard clinical indices [2].
Many different biomarkers associated with bone formation, resorption, and turnover have been assessed in GCF and saliva [27]. The RANK/RANKL/OPG system plays a significant role in the production and activation of osteoclasts, and therefore in the regulation of bone resorption [28]. The concentrations of salivary sRANKL and OPG, and the salivary sRANKL/OPG ratio in 50 patients with periodontitis and healthy individuals were evaluated in the current study. These results indicated that salivary sRANKL and sRANKL/OPG levels were significantly higher in patients with periodontitis. On the other hand, the difference in the salivary levels of OPG between groups was not statistically significant. Furthermore, positive correlations were found between CAL and PI with salivary concentrations of both sRANKL and the sRANKL/OPG ratio. A large number of investigations have evaluated GCF, RANKL, and OPG in periodontitis and healthy groups. They reported controversial results regarding the concentrations of RANKL and OPG, but the RANKL/OPG ratio had a tendency to be consistently higher in diseased sites. However, few studies have evaluated the salivary levels of RANKL and OPG [18-22].
The study by Frodge et al. [18] indicated that salivary RANKL was below the limit of detection in 81% of subjects, whereas it was detectable in all of the samples in the present study. This discrepancy may be attributed to the technical challenges of sampling, methodological variations in immunoassay analysis, and the differences in the extent, severity, and activity of the disease.
According to the study conducted by Miller et al. [19], the OPG concentration in whole saliva of patients with moderate to severe periodontitis was not correlated with periodontal status, which was in agreement with the current study.
Furthermore, our results are in accordance with Costa et al. [20] and Al-Sabbagh et al. [21], who reported that the OPG concentration in periodontitis patients was higher, although not significantly so, than in a control group.
Tobon-Arroyave et al. [22] performed a study to determine the variations in salivary concentrations of sRANKL and OPG, and the salivary sRANKL/OPG ratio, in smoking and non-smoking chronic periodontitis patients and healthy controls. In accordance with the current study, sRANKL and the sRANKL/OPG ratio were increased in the diseased group in their study. In contrast to the current study and the above-mentioned examinations, the OPG was significantly lower in the patients with periodontitis compared with that in healthy individuals in their study.
It is thought that compared with RANKL, OPG is more strongly affected by factors other than periodontal inflammation, including diabetes and smoking [20,29]. Therefore, it may be difficult to predict the variations of OPG concentration in different stages of periodontal disease. It seems that more studies to evaluate the factors affecting OPG levels are needed in the future. It should also be taken into account that RANKL and OPG have different sources of production. While the lymphocytes, which are one of the main producers of RANKL, are increased in active periodontal lesions, the origins of OPG are almost the same in disease and healthy states [30]. Perhaps this can explain to some extent why, compared with RANKL, the variations in OPG levels are not significant in the current study, similarly to the Miller et al. [19], Costa et al. [20], and Al-Sabbagh et al. [21] investigations.
In comparison to GCF analysis studies, outcomes of the current and other related investigations showed varying results regarding levels of RANKL and OPG in the saliva of patients with periodontal disease and healthy individuals. However, the ratio of sRANKL/OPG increased in diseased individuals in the present study and in a similar study by Tobon-Arroyave et al. [22].
Therefore, it seems that measuring the salivary sRANKL/OPG ratio could be a beneficial and convenient alternative to measuring GCF in the evaluation of periodontal disease.
It appears that the more important factor indicative of disease occurrence is the imbalance between OPG as a protective biomarker and RANKL as a pathogenic biomarker. However, the use of the salivary sRANKL/OPG ratio as a susceptibility, diagnostic, and predictive biomarker of periodontitis, will require further longitudinal studies with larger sample sizes in different populations.
Interpreting the results of this study should be performed with caution due to certain limitations. First, it is a cross-sectional study, and therefore it cannot determine disease activity. Second, the strict inclusion and exclusion criteria limited the sample size; however, this minimized potential confounding factors.
In conclusion, these findings suggest including the sRANKL/OPG ratio in a panel of salivary biomarkers that may be helpful in the screening and diagnosis of periodontitis.
Figures and Tables
Figure 1
A box plot showing the salivary level of soluble receptor activator of nuclear factor kappa B ligand (sRANKL). The results in this study showed that the mean value of sRANKL was significantly different between the two groups (P=0.004).
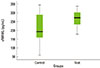
Figure 2
A box plot showing the salivary level of osteoprotegerin (OPG). The results in this study showed that no significant difference was found between the groups (P=0.455).

Figure 3
A box plot showing the salivary soluble receptor activator of nuclear factor kappa B ligand/osteoprotegerin (sRANKL/OPG) ratio. The results of this study indicated that the salivary sRANKL/OPG ratio differed significantly between the two groups (P=0.001).

ACKNOWLEDGEMENTS
This study has been supported by a grant from the Iranian National Elite Foundation. We would also like to extend our thanks to Mr. Reza Norian for his assistance during the laboratory procedures.
References
1. Genco RJ. Current view of risk factors for periodontal diseases. J Periodontol. 1996; 67:10 Suppl. 1041–1049.

2. Giannobile WV, Beikler T, Kinney JS, Ramseier CA, Morelli T, Wong DT. Saliva as a diagnostic tool for periodontal disease: current state and future directions. Periodontol 2000. 2009; 50:52–64.

3. Sexton WM, Lin Y, Kryscio RJ, Dawson DR 3rd, Ebersole JL, Miller CS. Salivary biomarkers of periodontal disease in response to treatment. J Clin Periodontol. 2011; 38:434–441.

4. Kaufman E, Lamster IB. Analysis of saliva for periodontal diagnosis: a review. J Clin Periodontol. 2000; 27:453–465.
5. Buduneli N, Kinane DF. Host-derived diagnostic markers related to soft tissue destruction and bone degradation in periodontitis. J Clin Periodontol. 2011; 38:Suppl 11. 85–105.

6. Suda T, Takahashi N, Udagawa N, Jimi E, Gillespie MT, Martin TJ. Modulation of osteoclast differentiation and function by the new members of the tumor necrosis factor receptor and ligand families. Endocr Rev. 1999; 20:345–357.

7. Yasuda H, Shima N, Nakagawa N, Yamaguchi K, Kinosaki M, Mochizuki S, et al. Osteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc Natl Acad Sci U S A. 1998; 95:3597–3602.

8. Quinn JM, Horwood NJ, Elliott J, Gillespie MT, Martin TJ. Fibroblastic stromal cells express receptor activator of NF-kappa B ligand and support osteoclast differentiation. J Bone Miner Res. 2000; 15:1459–1466.

9. Horwood NJ, Kartsogiannis V, Quinn JM, Romas E, Martin TJ, Gillespie MT. Activated T lymphocytes support osteoclast formation in vitro. Biochem Biophys Res Commun. 1999; 265:144–150.

10. Lacey DL, Timms E, Tan HL, Kelley MJ, Dunstan CR, Burgess T, et al. Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell. 1998; 93:165–176.

11. Kong YY, Yoshida H, Sarosi I, Tan HL, Timms E, Capparelli C, et al. OPGL is a key regulator of osteoclastogenesis, lymphocyte development and lymph-node organogenesis. Nature. 1999; 397:315–323.

12. Boyle WJ, Simonet WS, Lacey DL. Osteoclast differentiation and activation. Nature. 2003; 423:337–342.

13. Vega D, Maalouf NM, Sakhaee K. CLINICAL Review #: the role of receptor activator of nuclear factor-kappaB (RANK)/RANK ligand/osteoprotegerin: clinical implications. J Clin Endocrinol Metab. 2007; 92:4514–4521.

14. Crotti T, Smith MD, Hirsch R, Soukoulis S, Weedon H, Capone M, et al. Receptor activator NF kappaB ligand (RANKL) and osteoprotegerin (OPG) protein expression in periodontitis. J Periodontal Res. 2003; 38:380–387.

15. Mogi M, Otogoto J, Ota N, Togari A. Differential expression of RANKL and osteoprotegerin in gingival crevicular fluid of patients with periodontitis. J Dent Res. 2004; 83:166–169.

16. Vernal R, Chaparro A, Graumann R, Puente J, Valenzuela MA, Gamonal J. Levels of cytokine receptor activator of nuclear factor kappaB ligand in gingival crevicular fluid in untreated chronic periodontitis patients. J Periodontol. 2004; 75:1586–1591.

17. Bostanci N, Ilgenli T, Emingil G, Afacan B, Han B, Toz H, et al. Gingival crevicular fluid levels of RANKL and OPG in periodontal diseases: implications of their relative ratio. J Clin Periodontol. 2007; 34:370–376.

18. Frodge BD, Ebersole JL, Kryscio RJ, Thomas MV, Miller CS. Bone remodeling biomarkers of periodontal disease in saliva. J Periodontol. 2008; 79:1913–1919.

19. Miller CS, King CP Jr, Langub MC, Kryscio RJ, Thomas MV. Salivary biomarkers of existing periodontal disease: a cross-sectional study. J Am Dent Assoc. 2006; 137:322–329.
20. Costa PP, Trevisan GL, Macedo GO, Palioto DB, Souza SL, Grisi MF, et al. Salivary interleukin-6, matrix metalloproteinase-8, and osteoprotegerin in patients with periodontitis and diabetes. J Periodontol. 2010; 81:384–391.

21. Al-Sabbagh M, Alladah A, Lin Y, Kryscio RJ, Thomas MV, Ebersole JL, et al. Bone remodeling-associated salivary biomarker MIP-1α distinguishes periodontal disease from health. J Periodontal Res. 2012; 47:389–395.

22. Tobon-Arroyave SI, Isaza-Guzman DM, Restrepo-Cadavid EM, Zapata-Molina SM, Martinez-Pabon MC. Association of salivary levels of the bone remodelling regulators sRANKL and OPG with periodontal clinical status. J Clin Periodontol. 2012; 39:1132–1140.

23. Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999; 4:1–6.

24. Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964; 22:121–135.

25. Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975; 25:229–235.
27. Kinney JS, Ramseier CA, Giannobile WV. Oral fluid-based biomarkers of alveolar bone loss in periodontitis. Ann N Y Acad Sci. 2007; 1098:230–251.

28. Takayanagi H. Inflammatory bone destruction and osteoimmunology. J Periodontal Res. 2005; 40:287–293.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download