Abstract
Purpose
Cigarette smoking is a major risk factor in periodontal diseases. The pathogenesis of periodontal diseases may be affected by alterations of the inflammatory response by smoke. Nitric oxide (NO) is a gaseous, colorless, highly reactive, short-lived free radical with a pivotal role in the regulation of various physiological and pathological mechanisms in the body. It is important in host defense and homeostasis, on the one hand, whereas, on the other hand, it modulates the inflammatory response in periodontitis, leading to harmful effects. The aim of this study was to assess the levels of NO in both the serum and saliva of smokers and nonsmokers having chronic periodontitis and to compare them with periodontally healthy controls.
Methods
Sixty subjects participated in the study and were divided into three groups: group I, healthy nonsmoking subjects; group II, nonsmoking patients with chronic periodontitis; group III, smoking patients with chronic periodontitis. Each group consisted of twenty subjects. The biochemical estimation of NO in the collected serum and in the saliva was performed using the Griess colorimetric reaction.
Results
The results showed that the mean value of the salivary and serum NO was greater in group II than in group I, and also greater in group III than in group II.
Conclusions
NO appears to play an important and rather complex role in the immuno-inflammatory process and in the remodeling and maintenance of osseous structures. It is therefore logical that modulation of this mediator has potential for the treatment of a number of inflammatory conditions including periodontal disease.
Nitric oxide (NO) is a gaseous, colorless, highly reactive, short-lived free radical that plays a pivotal role in the regulation of various physiological and pathological mechanisms in the body [1]. It is formed in almost all cell types and despite the fact that it has a short half-life of approximately 4 seconds in vivo, it penetrates the surrounding tissues and activates a variety of cellular signaling pathways. NO is synthesized by the oxidative process of the guanidine of the amino acid L-arginine by a family of enzymes named NO synthases (NOS) [2]. This oxidative process produces NO and L-citrulline. Three isoforms of this group of enzymes have been identified: NOS1, NOS2, and NOS3. NOS1 and NOS3 are termed constitutive NOS, and were previously known as neuronal and endothelial NOS, respectively. The other isoform, NOS2, is termed inducible NOS (iNOS). iNOS is produced by immunocompetent cells such as macrophages infected with bacteria and is involved in the regulation of inflammatory reactions [3].
A simple rule about NO's role was established in the early 1990s. Low levels of NO, as produced by the constitutive NOS isoforms (NOS1 and NOS3), are involved in physiological homeostatic processes, whereas high levels, as produced by the inducible NOS isoform (NOS2), are involved in pathological processes, that is, altered physiologic conditions such as inflammation due to upregulation of NOS2 and NO production with indirect proinflammatory interactions [4]. NO exerts beneficial effects by acting as an antibacterial, antiparasital, antiviral, and antitumoricidal agent. Nonetheless, it has some detrimental effects if uncontrolled high levels of NO are present. High amounts of NO can react with superoxide anions generating highly toxic compounds. When NO is released simultaneously with superoxide, it forms the peroxynitrite anion, which is responsible for many of its cytotoxic effects, as it contains both reactive nitrogen as well as reactive oxygen species (ROS) [5]. Peroxynitrite has been shown to induce lipid peroxidation, and damage to proteins and nucleic acids, which results in DNA strand breaks.
Periodontitis, a chronic inflammatory disease of the periodontal tissues, is a multifactorial disease of bacterial origin [6,7]. The products of the bacteria and proinflammatory cytokines produced by inflammatory cells trigger the expression of iNOS, which is involved in inflammatory processes and accelerates periodontal disease. Hence, the evaluation of the involvement of NO in periodontal disease will enable us to understand one aspect of the complex process of periodontal disease progression.
Risk factors for periodontitis may be systemic or local, and among them, smoking is the most significant [8,9]. Periodontitis patients appear to express a hyperinflammatory phenotype involving excess or prolonged production of enzymes and ROS via activation of innate immune responses. Thus, cigarette smoke increases the oxidative burden, as it contains a large number of free radicals, and it has been suggested that it may increase the susceptibility to periodontal pathogens [10]. As smoking increases the risk of periodontitis, the present study aimed to evaluate the effect of smoking on oxidative stress in chronic periodontitis patients, that is, the NO levels in these patients.
The present study was conducted in the Department of Periodontology, Dr Z.A. Dental College, Aligarh Muslim University, Aligarh, India. The institutional ethics committee of the faculty of medicine approved the study. This was a case-control study in smokers and nonsmokers with chronic periodontitis. This study compared the serum and salivary NO levels of smoking and nonsmoking chronic periodontitis patients to those of clinically healthy patients as controls.
Sixty subjects participated in the study and were divided into three groups: group I, healthy nonsmoking subjects; group II, nonsmoking patients with chronic periodontitis; and group III, smoking patients with chronic periodontitis. Each group consisted of 20 subjects.
Clinical examinations were performed using the plaque index (PI), gingival index (GI), probing pocket depth (PD) and clinical attachment level (CAL), except for control group subjects, whose clinical attachment levels were not recorded. Using a University of North Carolina-15 periodontal probe, the pocket depth was measured as the distance from the gingival margin to the base of the pocket in millimeters. The clinical attachment levels were calculated from the recession and pocket depth measures and represented as the distance in millimeters from the cementoenamel junction to the base of the pocket. All of the measurements were examined at 6 sites per tooth excluding third molars. Informed consent was obtained from all of the patients before participating in the study.
The inclusion criteria for patient selection were as follows: Individuals with a minimum of 20 teeth were enrolled in the study.
No history of systemic diseases, no history of smoking, and clinically healthy periodontal status, that is, a PD of ≤2 mm along with no signs of inflammation.
Subjects with ≥30% of sites with the presence of a PD of ≥4 mm along with a CAL of ≥4 mm [11].
Exclusion criteria included the following: pregnant women or lactating mothers; subjects treated for periodontitis in the past 6 months; subjects on antibiotics, anti-inflammatory therapy, or vitamin/nutritional supplements; and subjects with systemic diseases such as diabetes mellitus, hypertension, renal disease, rheumatoid arthritis, periapical infection of any tooth, or any other form of systemic inflammatory involvement.
Two-mililiter venous blood and 4 mL of unstimulated saliva was collected in a vacutainer and sterile plastic vial, respectively, from all of the subjects and controls. The blood and saliva samples were then centrifuged at 3,000 rpm and 2,500 rpm, respectively, for 5 minutes. The biochemical estimation of NO in the collected serum and in the supernatant obtained from the saliva was performed using the Griess colorimetric reaction.
Estimation of NO in the serum and saliva was evaluated by the measurement of nitrite (NO2), the stable product of decomposition, employing the Griess reaction according to the method of Green et al. [12].
The Griess reaction involves formation of a chromophore during the reaction of nitrite with sulfanilamide and heterocyclic amine of naphthylene-ethylene-diamine (Griess reagent) under low pH conditions. During this reaction, acidified nitrite undergoes diazotization with sulfanilamide to form a diazonium salt. This diazonium salt then couples to N-(1-Naphthyl)ethylenediamine to form a magenta-colored azo dye with a characteristic absorption spectrum. The only stable product formed by spontaneous autoxidation of NO in oxygenated solutions is NO2.
The following materials were used to freshly prepare Griess reagent each time before use for NO estimation: ortho-phosphoric acid (about 85% pure; Merck KGsA, Damstadt, Germany), purified sodium nitrite (Merck KGsA, Damstadt, Germany), N-(1-naphthyl) ethylenediamine dihydrochloride (Merck KGaA, Darmstadt, Germany), sulfanilamide (4-aminobenzene sulphonamide) (Bio Basic Inc., Markham, ON, Canada).
The serum and saliva samples were processed on the same day that the assay was performed. One hundred microliters of each of the test samples were added to microwells. Fifty microliters of Griess reagent 1 and 50 µL of Griess reagent 2 were added to each well and mixed thoroughly by tapping the sides. After 10 minutes of incubation at room temperature, the absorbance was read at 540 nm using an iMark microplate reader from Bio-Rad Laboratories Inc. (Hercules, CA, USA). The nitrite content in the samples was determined from the standard curve (Fig. 1) constructed from the known standard concentration, and their corresponding absorbance value by a linear regression equation.
Data was summarized as mean±standard deviation (SD). The groups were compared by one-way analysis of variance, and the significance of the mean difference between the groups was calculated by Tukey Honest Significant Difference post hoc test. All of the analyses were performed on STATISTICA ver. 6.0 (Informer Technologies Inc).
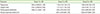
Table 1 shows that the mean PI, PD, and CAL values of groups 2 and 3 were comparatively higher than those of group 1, with the highest values in group 3. However, this trend was not seen in the GI values as the mean GI values of group 2 and group 3 were comparatively higher than that of group 1, with the highest value in group 2. The NO in the serum and saliva of the three groups are summarized in Table 2 and show that the mean NO in the serum and saliva values of group 2 and group 3 were significantly (P<0.05) higher than those of group 1, with the highest being in group 3. A significant trend was observed in which smoker subjects with chronic periodontitis exhibited an increase in serum and saliva NO levels compared to those in nonsmoker subjects with chronic periodontitis, and in turn nonsmoker subjects with chronic periodontitis had greater NO levels in serum and saliva than the healthy controls. There was a significant difference between the groups (group 1 to group 2, group 1 to group 3, and group 2 to group 3) for both serum and salivary NO levels.
The findings of Batista et al. [13] demonstrated a significant increase in iNOS expression in periodontitis patients as compared to gingivitis samples and in gingivitis samples as compared to the controls. Another study by Reher et al. [14] revealed that periodontal disease and its severity are related to salivary nitrite concentration. Recently, Menaka et al. [15] also showed subjects with periodontitis had significantly higher nitrite in serum than healthy subjects. Our results were in accordance with these studies. In contrast, one rare report described a reduction of salivary NO levels in individuals with adult periodontitis and with aggressive periodontitis [16]. This report was in disagreement with the vast majority of the literature that describes increased levels of NO in periodontal disease.
The results of our study showed significantly increased concentrations of serum and salivary NO in patients with chronic periodontitis, as compared to the healthy control group. This finding was expected, as it was shown that NO synthesis increases in inflamed periodontal tissues as during inflammation proinflammatory cytokines and bacterial cell wall components stimulate the production of NO by inducible NO [17,18].
Although both groups 2 and 3 subjects had generalized chronic periodontitis or a similar severity of periodontal inflammation, the results showed significantly increased concentrations of serum and salivary NO in smokers (group 3) as compared to nonsmokers (group 2) with chronic periodontitis. Thus the difference between NO levels in groups 2 and 3 was due to smoking. A possible explanation for this could be that the harmful effects of smoking manifest themselves by interfering with vascular and immunologic reactions, as well as by undermining the supportive functions of the periodontal tissues. Also, the large number of free radicals in cigarette smoke may increase the susceptibility to periodontal pathogens and due to the presence of a wide variety of ROS, smokers were found to present with high levels of oxidant stress. Another mechanism might be that the exposure to cigarette smoke in periodontitis leads to increased lipid peroxidation [19]. Therefore, it can be suggested that oxidative damage in periodontitis was aggravated by the effect of smoking.
In a study by Epperlein et al. [10], it was suggested that one of the main pathways to damage caused by the gas phase of cigarette smoke was through the NO and hydrogen peroxide interaction giving rise to an active molecule (which may be singlet oxygen) that can initiate lipid peroxidation, and red blood cell glutathione is one of the chief sources of protection against this damage. Another study by Dhotre et al. [20] showed a significant increase in serum lipid peroxide and NO with a corresponding decrease in serum superoxide dismutase, glutathione peroxidase, and total antioxidant capacity in periodontitis patients. Further, it was noted that the oxidant levels were significantly higher and antioxidants were significantly lower in smoker patients than nonsmoker patients. Thus, smoking plays a pivotal role in enhancing the oxidative burden in periodontitis.
There were some limitations of this study, such as the small sample size. Thus, further longitudinal studies must be undertaken involving a larger number of subjects to evaluate the role of NO in other forms of periodontitis and gingivitis during different stages of periodontal disease progression. In addition, there may be other influencing factors such as stress and dietary factors that cannot be controlled and may effect NO levels.
To the best of our knowledge, this study was the first to investigate the association among smokers and nonsmokers with chronic periodontitis based upon NO levels. As demonstrated by previous studies, NO appears to play an important and rather complex role in the immuno-inflammatory process and in the remodeling and maintenance of osseous structures. It is, therefore, logical that modulation of this mediator has potential for the treatment of a number of inflammatory conditions including periodontal disease.
As various reports have proposed a role for NO in the progression of periodontal disease, some investigators have suggested the selective inhibition of iNOS and scavenging of peroxynitrite or neutralization of reactive species by antioxidant substances (green tea) as a promising novel approach for the treatment of periodontitis.
The anti-inflammatory effects of Lactobacillus brevis in chronic periodontitis could also be attributed to its capacity to prevent the production of NO and, consequently, the release of prostaglandins E2 and the activation of matrixmetalloproteinases induced by NO [21].
A novel mechanism of action of tetracyclines was to inhibit the expression of NOS. Since the overproduction of NO has been implicated in the pathogenesis of inflammatory diseases, tetracyclines should be evaluated as potential therapeutic modulators of NO for various pathological conditions [22].
More studies and further exploration of these new non invasive treatment approaches incorporating the above-mentioned future implications of NO must be done to improve periodontal health.
To conclude, serum and salivary NO levels can be utilized as a good indicator of the inflammatory status of the periodontium. Furthermore, the results suggest that the more destructive nature of periodontal disease in smokers leads to an increase in serum and salivary NO levels.
Figures and Tables
Table 2
Nitric oxide status in serum and saliva of three groups.

Values are presented as mean±standard deviation (range). F value=3.11 (one way analysis of variance post hoc test [Tukey-equal variances assumed]). df=19.
Group 1: normal, group 2: nonsmoker, group 3: smoker.
a)Statistically significant difference compared to group 1 (P<0.05). b)Statistically significant difference compared between groups 2 and 3 (P<0.05).
References
1. Moncada S, Higgs EA. Endogenous nitric oxide: physiology, pathology and clinical relevance. Eur J Clin Invest. 1991; 21:361–374.

3. Nussler AK, Billiar TR. Inflammation, immunoregulation, and inducible nitric oxide synthase. J Leukoc Biol. 1993; 54:171–178.

4. Kroncke KD, Fehsel K, Kolb-Bachofen V. Nitric oxide: cytotoxicity versus cytoprotection: how, why, when, and where? Nitric Oxide. 1997; 1:107–120.

6. Nunn ME. Understanding the etiology of periodontitis: an overview of periodontal risk factors. Periodontol 2000. 2003; 32:11–23.

8. Johnson GK, Hill M. Cigarette smoking and the periodontal patient. J Periodontol. 2004; 75:196–209.

9. Razali M, Palmer RM, Coward P, Wilson RF. A retrospective study of periodontal disease severity in smokers and non-smokers. Br Dent J. 2005; 198:495–498.

10. Epperlein MM, Nourooz-Zadeh J, Noronha-Dutra AA, Woolf N. Nitric oxide in cigarette smoke as a mediator of oxidative damage. Int J Exp Pathol. 1996; 77:197–200.

11. American Academy of Periodontology. Parameter on chronic periodontitis with slight to moderate loss of periodontal support. J Periodontol. 2000; 71:5 Suppl. 853–855.
12. Green LC, Wagner DA, Glogowski J, Skipper PL, Wishnok JS, Tannenbaum SR. Analysis of nitrate, nitrite, and [15N]nitrate in biological fluids. Anal Biochem. 1982; 126:131–138.

13. Batista AC, Silva TA, Chun JH, Lara VS. Nitric oxide synthesis and severity of human periodontal disease. Oral Dis. 2002; 8:254–260.

14. Reher VG, Zenobio EG, Costa FO, Reher P, Soares RV. Nitric oxide levels in saliva increase with severity of chronic periodontitis. J Oral Sci. 2007; 49:271–276.

15. Menaka KB, Ramesh A, Thomas B, Kumari NS. Estimation of nitric oxide as an inflammatory marker in periodontitis. J Indian Soc Periodontol. 2009; 13:75–78.

16. Aurer A, Aleksic J, Ivic-Kardum M, Aurer J, Culo F. Nitric oxide synthesis is decreased in periodontitis. J Clin Periodontol. 2001; 28:565–568.

17. Matejka M, Partyka L, Ulm C, Solar P, Sinzinger H. Nitric oxide synthesis is increased in periodontal disease. J Periodontal Res. 1998; 33:517–518.

18. Lappin DF, Kjeldsen M, Sander L, Kinane DF. Inducible nitric oxide synthase expression in periodontitis. J Periodontal Res. 2000; 35:369–373.

19. Ojima M, Hanioka T. Destructive effects of smoking on molecular and genetic factors of periodontal disease. Tob Induc Dis. 2010; 8:4.

20. Dhotre PS, Suryakar AN, Bhogade RB. Oxidative stress in periodontitis. Eur J Gen Med. 2012; 9:81–84.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download