INTRODUCTION
In contemporary dentistry, there has been increasing demand for improved aesthetics by both dentists and patients. The teeth and gingiva play an important role in an esthetic smile. A balanced size, shape, position, and color of the teeth in harmony with the surrounding tissue are essential components. The existence of the interproximal papilla is pivotal to an esthetic gingival form [
1,
2], which is determined by the form and position of the clinical crown, interproximal contact point, and form of embrasure space [
3]. The loss of the interproximal papilla causes an open embrasure space, food impactions, and phonetic problems. In particular, the loss of maxillary anterior teeth and the interproximal papilla is a decisive factor in esthetic impairment [
4,
5]. In this regard, clinicians should carefully analyze the factors that affect the integrity of the interproximal papilla to prevent its loss or restore it [
6].
The distance from the contact point to the bone crest, inter-radicular distance, size of the embrasure space, tooth shape, and gingival biotype have been listed to be relevant factors, among which the distance from the contact point to the bone crest, the vertical element of the inter-radicular space were claimed to be the most important to determining its existence. Tarnow et al. [
4] suggested that the interproximal papilla shows complete fidelity if the distance from the contact point to the bone crest is less than 5 mm but the fidelity of the interproximal papilla is reduced if it is greater than 7 mm. Chen et al. [
7] also supported this notion that the number of interproximal papilla that fill up the inter-radicular space decreases with increasing distance. Chang [
8] claimed that the distance from the contact point to the bone crest is closely related to the receded papilla, and only the distance from the cemento-enamel junction (CEJ) to the bone crest has a statistically significant relationship.
The inter-radicular space was examined as a potential element. Several studies have reported that the number of interproximal papillae that show complete fidelity decreases with increasing inter-radicular distance, which is measured at the level of the bone crest [
6,
7,
9]. In contrast, Sasaki et al. [
10,
11] claimed that the inter-radicular distance does not affect the papilla height but affects the appearance. Taken together, these reports have shown that the fidelity or appearance of the interproximal papilla improves as the inter-radicular distance becomes narrower.
The size of the embrasure space is also related to the fidelity of the interproximal papilla. There is a high probability that the fidelity of the interproximal papilla decreases if the size of the embrasure space increases due to the long distance from the contact point to the bone crest and long inter-radicular distance [
3,
7,
12,
13].
The morphological properties of the periodontal tissues are related to the shape and appearance of the teeth [
14,
15], which is generally divided into triangular, oval, and rectangular types. Chen et al. [
7] suggested that there is a high likelihood that the fidelity of the interproximal papilla increases as the tooth shape becomes more rectangular. Kois [
12] and Shigeno [
16] further claimed that a rectangular tooth shape has a longer contact area and requires less of the interproximal papilla to fill up the embrasure space.
The appearance of the gingiva can be divided into 2 types, a thick and flat form or a thin and scalloped shape, as classified by Ochsenbein and Ross [
17]. Subsequently, Seibert and Lindhe [
18] introduced the term "gingival biotype." Kois [
12] reported that the thick gingival biotype is resistant to gingival recession, whereas the thin gingival biotype carries a high risk of interproximal papilla recession. Maynard Jr and Wilson [
19] also suggested that the risk is affected by the gingival biotype and alveolar bone, and that there is a higher risk of recession if the gingiva and cortical bone plate is thin.
However, few studies have examined the existence of the interproximal papilla from the perspective of multilateral factors. In particular, there is a paucity of studies on the position of the interproximal papilla, such as the appearance and height of the interproximal papilla. Comprehensive analysis of the factors related to the fidelity of the interproximal papilla is essential for prevention and management.
In this regard, the present study was designed to analyze an array of elements that may be associated with the relative position and appearance of the interproximal papilla of healthy maxillary central incisors.
MATERIALS AND METHODS
Subjects
One hundred and forty-seven healthy interproximal papilla between the maxillary central incisors were examined (male, 74; female, 73; average age, 25.36±7.58 years). The inclusion criteria were as follows:
1) No redness or swelling on the gingiva
2) Probing pocket depth within 3 mm and no attachment loss in the buccolingual sites of the central incisors
3) No radiographic evidence of alveolar bone resorption between the central incisors
4) No orthodontic appliance or prosthesis on the central incisors
The protocol for human subjects was reviewed and approved by the Institutional Review Board of Pusan National University Hospital in 2011 (No. 2011085).
Clinical measurement
The following parameters were measured using the periodontal pocket probe (William's probe, Osung, Seoul, Korea) and electronic calipers (Digimatic Caliper, Mitutoyo Co., Kawasaki, Japan):
1) The amount of recession of the interproximal papilla: the distance between the lowest part of the contact area and the interproximal papilla tip
2) The length of the interproximal contact area: the distance between the incisal part of the contact area and the lowest part of it
3) Gingival biotype: classified into the thick or thin gingiva biotypes according to the degree of reflection of the periodontal pocket by inserting the periodontal pocket into the buccal gingiva
4) Form of the papilla tip: pointed type or flat type
Radiograph measurement
Periapical radiographs of the maxillary anterior teeth were taken using the parallel photographing technique using an auto-radiographic indicator and 1-mm grid metal piece, and converted to digital images. The following indicators were measured in pixel units on the digital images using a image evaluation program (Image J, JAVA, National Institutes of Health, Bethesda, MD, USA):
1) Distance from the apical end of the contact point to the bone crest
2) Distance from the apical end of the contact point to the CEJ: the distance between the apical end of the contact point and a line connecting the adjacent CEJ of both sides of the maxillary central incisor
3) Distance from the CEJ to the bone crest: the distance between the line connecting the adjacent CEJ of both sides of the maxillary central incisor and the bone crest
4) Inter-radicular distance: inter-radicular distance at the level of the bone crest
5) Size of the embrasure space: size of the embrasure space 2-dimensionally, referring to the distance from the contact point to the bone crest (vertical element) and the inter-radicular distance (horizontal element)
-
6) Tooth shape: the tooth shape was measured using the noninvasive radiological method reported by Chen et al. [7] (Fig. 1). The horizontal distance between the adjacent CEJ of both sides of the maxillary central incisor and the central line of the teeth was measured (Fig. 1; d1, d3), and the horizontal distance between the lowest part of the contact area and the central line of the teeth was determined (Fig. 1; d2, d4). The tooth shape (mean mesial divergence ratio of the maxillary central incisor) was calculated using the following equation.
Tooth shape (mean mesial divergence ratio of the maxillary central incisor)=[(d1/d2)+(d3/d4)]÷2
As the value becomes either lower or higher, the tooth shape was considered to be either triangular or rectangular, respectively.
7) The papilla height was determined by subtracting the amount of recession of the interproximal papilla from the distance from the contact point to the bone crest.
Data analysis
The following results were analyzed using the clinical and the radiological measurements explained above:
1) The amount of recession of the interproximal papilla according to the elements that are associated with the relative position of the maxillary central incisor interproximal papilla
2) Elements that are associated with the relative position of the bone crest
3) The correlation among the elements
The analysis of the correlation among the elements included:
The correlation among tooth shape and inter-radicular distance, length of the interproximal contact area, size of the embrasure space, and gingival biotype
The correlation among the form of the papilla tip and tooth shape, inter-radicular distance, and distance from the CEJ to the bone crest
The correlation among the papilla height and gingival biotype, and the inter-radicular distance
The correlation among the distance from the contact point to the bone crest and inter-radicular distance, and the tooth shape
The correlation among the distance from the CEJ to the bone crest and inter-radicular distance, and the tooth shape
Statistical analysis
IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA) was used for statistical analysis. The mean and the standard deviation of the clinical and the radiological measurements were calculated. The Pearson correlation coefficient was used to examine the relationship between the recession of the interproximal papilla and the elements that are believed to affect it, as well as the relationship among the elements that are associated with the recession of the interproximal papilla. A P-value< 0.05 was considered significant.
The form of the papilla tip and the gingival biotype that appear with qualitative variables were assessed using Spearman rank-order correlation after setting the flat type interproximal papilla tip and thin gingival biotype to 1, and the pointed type interproximal papilla tip and thick gingival biotype to 0.
DISCUSSION
This study examined the elements that are associated with the relative position of the interproximal papilla of healthy maxillary central incisors, which plays an important role in healthy interproximal papillae, particularly in their aesthetics. Many studies have examined the elements that are associated with the existence of the interproximal papilla, but few have examined the existence of the interproximal papilla from the perspective of multilateral factors. In particular, there is a paucity of studies on the position of the interproximal papillae, such as the appearance and height of the interproximal papillae. Moreover, for the interproximal papillae, in addition to the pathological recession related to periodontal disease, recession can also occur in healthy gingiva due to anatomical and physiological predispositions to recession [
20]. Therefore, this study examined the various elements that are associated with the relative positions of the interproximal papilla of healthy maxillary central incisors.
Similar to previous studies [
4,
7,
9,
21], the increase in the distance from the contact point to the bone crest and the distance from the CEJ to the bone crest also had a strong correlation with the amount of recession of the interproximal papilla. On the other hand, in contrast to Chang [
8], who claimed that only the distance from the CEJ to the bone crest showed a statistically significant correlation, the distance from the contact point to the CEJ also showed a significant correlation with an increasing amount of recession of the interproximal papilla.
For the inter-radicular distance, Chow et al. [
6], Chen et al. [
7], and Cho et al. [
9] concluded that the number of interproximal papillae that shows complete fidelity decreases with increasing inter-radicular distance. Similarly, in this study, the amount of recession of the interproximal papilla also increased with increasing inter-radicular distance. In the present study, the form of the papilla tip tended to be the flat type as the inter-radicular distance increased. These results are similar to those reported by Sasaki et al. [
10,
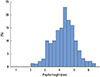
11], in that the inter-radicular distance affects the form of the papilla tip. In the present study, there were no significant correlations between the inter-radicular distance and papilla height, and the mean papilla height was 4.25±0.84 mm with a maximum and minimum of 6.3 mm and 2.2 mm, respectively. The mean papilla height in most participants was 4 to 4.5 mm, with more than 50% between 4 and 5 mm. When the 95% confidence interval was selected, the mean interproximal papilla height was within 4.11-4.39 mm. This means that the papilla height was within a regular range regardless of the inter-radicular distance. This is similar to that reported by Sasaki et al. [
10,
11], who showed that the inter-radicular distance is not involved in the papilla height, and the papilla height is approximately 4 mm regardless of the inter-radicular distance.
An examination of the inter-radicular distance revealed no correlation between the distance from the contact point to the bone crest, and the distance from the CEJ to the bone crest. That is, the horizontal element of the embrasure space was not associated with the vertical elements of the embrasure space.
For the tooth shape, a significant correlation was observed between the increase in the amount of recession of the interproximal papilla and the tooth shape, which is similar to Zetu and Wang [
3], who reported that the gingival shapes and forms vary and are affected by the size and appearance of teeth, position and size of the interproximal contact point, and volume of the embrasure space. The inter-radicular distance, length of the interproximal contact area, and the size of embrasure space can be considered related elements.
For the length of the interproximal contact area, Chow et al. [
6] reported that teeth with interproximal papillae with high fidelity appear to have longer interproximal contact, and the length of the interproximal contact area on a gingival papilla with high fidelity was 0.6 mm longer than that with low fidelity. This shows that the length of the interproximal contact area is associated with the fidelity of the interproximal papilla. For the embrasure space, Kois [
12] and Spear [
22] reported that the volume of the embrasure space is associated with the fidelity of the interproximal papilla. In the present study, the amount of recession of the interproximal papilla decreased with increasing interproximal contact area, decreasing embrasure space, and with a more rectangular the tooth shape. Moreover, the tooth shape had a significant correlation with the length of the interproximal contact area, size of the embrasure space, and inter-radicular distance. In addition, the length of the interproximal contact area increased and the inter-radicular distance decreased as the tooth shape became more rectangular. This reduced the size of the embrasure space, which resulted in a decrease in the amount of recession of the interproximal papilla.
The distance from the contact point to the bone crest and the distance from the CEJ to the bone crest increased as the tooth shape became more triangular. That is, the tooth shape is associated with the bone level of the bone crest, and the distance from the contact point to the bone crest had a stronger correlation than the distance from the CEJ to the bone crest. In this way, the tooth shape is associated with the distance from the contact point to the bone crest (vertical distance) and the inter-radicular distance (horizontal distance), influencing the size of the embrasure space, which has a relationship with the amount of recession of the interproximal papilla.
The tooth shape also had a relationship with the form of the papilla tip. The interproximal papilla tip tended to be the flat type when it had a triangular tooth shape. In the triangular tooth shape, compared to the rectangular tooth shape, the bone crest was located lower than the CEJ, and although the papilla height was the same, the interproximal papilla existing between the CEJ and bone crest became longer. That is, the interproximal papilla hidden in the low part of the CEJ is placed deeper, and the interproximal papilla tip is placed lower. On the other hand, the interproximal contact point was located on the upper part for the triangular tooth shape. Therefore, the interproximal papilla has a lower probability of showing complete fidelity. This means that even in a healthy status without inflammation, the fidelity of the interproximal papilla can be reduced if the tooth shape is triangular due to an increase in the amount of recession of the interproximal papilla and the formation of a flat type interproximal papilla tip. Moreover, when periodontal disease is involved, for a triangular tooth shape, where the angle between crowns becomes dramatically larger, the degree appears to stand out when the recession of the interproximal papilla appears.
Although previous studies [
23] reported that if the tooth shape is rectangular, the interproximal papilla would likely be the flat type, the present study showed that the papilla tip is likely to be the pointed type when the tooth shape is rectangular. However, the flat type means there is little difference in the heights of the interproximal gingiva and marginal gingiva, which should be differentiated from the form of the papilla tip.
For the gingival biotype, unlike Kois [
12] or Maynard Jr and Wilson [
19], who claimed that it affected the gingival recession, no significant correlation was found between the gingival biotype and the amount of recession of the interproximal papilla, and there was no correlation between the gingival biotype and the heights of the interproximal papilla. An infiltrating method [
23,
24], which uses a periodontal probe or needle under local anesthesia, and a noninfiltrating method [
6,
25,
26], which uses ultrasonic waves or computed tomography (CT), were used to measure the thickness of the gingiva. This study used the probe transparency method to classify the thick gingival biotype and thin gingival biotype. Kan et al. [
27] reported that the probe transparency method does not reveal a difference from the gingival biotype measured by CT, whereas Fu et al. [
25] claimed that the probe transparency method is not a proper method for measuring the gingival biotype. This study measured the gingival biotype qualitatively, but the result might have been different if it were measured quantitatively using ultrasonic waves or other techniques.
Many studies have examined the correlation between the tooth shape and gingival biotype. Sanavi et al. [
28] claimed that the thick and flat periodontal tissues have a rectangular tooth shape, and the thin scallop-shaped periodontal tissues have a triangular tooth shape. Olsson and Lindhe [
29] reported that long and narrow crowns have thin periodontal tissues and a high likelihood of having gingival recession compared to the thick gingival biotype, suggesting a relationship between the tooth shape and gingival biotype. On the other hand, Olsson et al. [
23] reported no relationship between the tooth shape and gingival thickness according to the crown width and length. Similarly, there are a range of opinions concerning the relationship between the tooth shape and gingival biotype, and the present study could not find any significant correlation between them, which is similar to Olsson et al. [
23].
The elements that are associated with the distance from the contact point to the bone crest and the distance from the CEJ to the bone crest, i.e., the relative level of the bone crest, would be the inter-radicular distance and tooth shape, but the inter-radicular distance did not show a statistically significant correlation. Only the tooth shape showed a correlation. As the tooth shape became more triangular, the distances from the contact point to the bone crest and from the CEJ to the bone crest became longer. This means that the tooth shape is the element that is associated with the relative position of the bone crest.
For the esthetic success of dental treatments, it is important to understand the characteristic behavior of the interproximal papilla. Therefore, this study analyzed diverse elements that are associated with the relative positions and forms of the interproximal papillae of healthy maxillary central incisors as well as the correlations among them.




 PDF
PDF ePub
ePub Citation
Citation Print
Print











 XML Download
XML Download