Abstract
Purpose
The aim of the present clinical trial was to compare pain during injection of anterior middle superior alveolar (AMSA) technique with that of infiltration injection technique in the maxilla in periodontal flap surgeries of patients referring to the Department of Periodontics, Faculty of Dentistry, Tabriz University of Medical Sciences.
Methods
Twenty subjects with an age range of 20 to 40 years were selected for the present study. One side of the maxilla was randomly selected as the test side and the other as the control side using a flip of a coin. AMSA technique was used on the test side and infiltration technique was used on the control side for anesthesia. On both sides 2% lidocaine containing 1:80,000 epinephrine was used for anesthesia. The operator obtained the visual analogue scale for each patient immediately after the injection and immediately after surgery. Data was analyzed using descriptive statistical methods (frequency percentages, means and standard deviations) and Wilcoxon's test using SPSS ver. 13 (SPSS Inc.). Statistical significance was defined at P<0.05.
Maxillary periodontal surgery typically requires multiple injections to obtain anesthesia of the hard and soft tissues. Posterior and superior, middle superior alveolar (MSA), and anterior superior alveolar (ASA) block injections are used to anesthetize buccal tissues, whereas greater palatine and nasopalatine blocks are used for palatal anesthesia. Although these injections effectively anesthetize maxillary tissues, it may also affect facial structures, such as the upper lip, lateral aspect of the nose and lower eyelid [1]. In addition, the pain of these repetitive trasmucosal punctures is unpleasant for the patient. A new technique has been introduced for anesthetizing maxillary teeth: anterior MSA (AMSA) injection [2-4]. Friedman and Hochman [2-4] defined the AMSA injection and a number of its clinical applications. The AMSA injection site is located palatally at a point that bisects the premolars and is approximately halfway between the midpalatine raphe and the crest of the free gingival margin [2-4]. Following diffusion of the anesthetic agent, anesthesia of structures typically innervated by the greater palatine nerve, nasopalatine nerve, ASA nerve, and MSA nerve is achieved [2-4]. The MSA and ASA nerves are given off from the infraorbital nerve before their exit from the infraorbital foramen [1]. The MSA nerve is thought to innervate the maxillary premolars and plays some role in pulpal innervation of the mesiobuccal root of the first molar [1]. The ASA nerve provides pulpal innervations to the central and lateral incisors and canines [1]. A bilateral AMSA injection supposedly anesthetizes 10 maxillary teeth extending from the second premolar on one side to the second premolar on the opposite side [3]. To avoid patient discomfort due to the tightly bound nature of palatal tissues, the anesthetic agent should be injected into the site at a moderate rate of 0.5 mL per minute [3]. Computer-controlled anesthetic delivery systems have been recommended to achieve this consistent anesthetic delivery rate, although this is not an absolute requirement [5]. Studies on AMSA injection have demonstrated inconclusive evidence as to its effectiveness on pulpal tissues. Depending on the method of anesthetic delivery and tooth type, complete pulpal anesthesia with AMSA injections ranges from 20 to 86% [6,7].
The AMSA technique has been recommended for procedures ranging from operative restorations to scaling and root planing [4,5]. Holtzclaw and Tosano [8] in 2005 evaluated a case series of AMSA injection techniques for a variety of maxillary surgical procedures and described the benefits of this technique, including avoidance of undesirable collateral anesthesia and a reduced number of injections. The aim of this study was to compare the pain severity of infiltration injections with that of AMSA technique on opposite sides of maxilla in periodontal flap surgery.
Twenty adult patients (10 males and 10 females) who had moderate to severe chronic periodontitis with indication of periodontal surgery on both left and right maxillary sides participated in this study. They ranged in age from 20 to 40 years and were in good health. The patients were not taking any medications that would alter their pain perception, as determined by a written medical health form and oral questioning. Allergy to lidocaine, history of significant medical problems, use of central nervous system depressants within the previous 48 hours, pregnancy and inhibition to give informed consent were the exclusion criteria. The study design was approved by the Ethics Committee and supported by the Research Deputy of Tabriz Medical Sciences University. The nature of this investigation was explained to the participants in detail and the patients signed an informed consent form. All the patients underwent initial therapy, consisting of oral hygiene instructions and full-mouth scaling and root planing. In order to perform the periodontal surgery, AMSA technique and infiltration injections were administered on opposite maxillary arches by the same operator.
At baseline examination, the periodontist instructed the subjects to use a visual analog scale (VAS) [9] to record the level of pain they felt during treatment procedures. VAS was scored on a 100-mm horizontal line with the left endpoint marked "no pain" and the right endpoint marked "pain as bad as it can be." To eliminate people who were stoic about pain, only the subjects were enrolled in the study, who registered VAS pain scores of greater than 20 during periodontal probing at baseline examination. This study was carried out according to a split-mouth design, with both injections given to all the patients. For each patient, the AMSA technique was used on one side and the infiltration injections on the contralateral side. The order of anesthesia techniques was randomly selected by the flip of a coin. The subjects received the injections during two separate appointments spaced at least 1 week apart in a crossover design. The AMSA injection site is located at a point that bisects the maxillary first and second premolars, and midway between the crest of the free gingival margin and mid-palatine suture. The needle is orientated at a 45-degree angle with the bevel facing the palatal tissue (Fig. 1). All the injections were given by the same operator. Surgical sites were anesthetized utilizing 1 to 2 cartridges of lidocaine 0.2% (1:80,000 epinephrine) with a conventional syringe and a 27-gauge dental needle. The operator obtained the VAS for each patient immediately after the injection was administered. All the surgical procedures were performed by the same surgeon. Surgery consisted of an open flap debridement procedure, reflection of a full-thickness mucoperiosteal flap and debridement of the exposed roots and osseous defects with hand and ultrasonic instruments. Bone architecture was not corrected except when it prevented good tissue adaptation to the cervical areas of the teeth. The flap was repositioned and sutured using 4-0 silk sutures (interrupted direct sutures). Subsequent to the surgery the patients were also asked to determine the severity of their discomfort on VAS.
After the surgical procedure the patients were asked to use 0.2% chlorhexidine gluconate mouthwash twice daily for 4 weeks. Acetaminophen was prescribed for the relief of postoperative pain and 500-mg Amoxicilin capsules tid were administered for 10 days.
Twenty subjects (10 males and 10 females) with an age range of 20 to 40 years were evaluated in the present study. The mean ages of the subjects in the AMSA and infiltration groups were 42.9±8.04 and 41.75±8.32 years, respectively. The results of the test for mean differences in independent groups did not reveal any statistically significant differences (P=0.66). None of the subjects reported any adverse events, including ulcerations, soreness or swelling in relation to injections the day after treatment. In addition, no history or clinical evidence of swelling or ulceration was observed at any treatment visit or the final examination visit. The VAS data is presented in Table 1.
Data analysis did not reveal any significant differences in pain severity during injection between AMSA and infiltration anesthetic techniques (P=0.856). However, there were significant differences in postoperative pain severity between the two techniques (P=0.025).
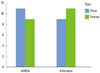
There were no significant differences between males and females in relation to pain severity between the AMSA and infiltration techniques (P=0.75). In the AMSA technique, pain severity scores were 11 and 9 in males and females, respectively. In the infiltration technique, pain severity scores were 9 and 11 in males and females, respectively (Fig. 2).
Proper anesthesia is of utmost importance in dental procedures. Therefore, selection of an appropriate anesthetic technique is particularly important. In periodontal surgeries in maxilla, AMSA anesthetic technique, in comparison with the infiltration technique, is a single injection technique, which anesthetizes the maxillary teeth and the relevant gingival tissues without any need for direct injection in the area needing anesthesia; at the same time, it preserves the function of the upper lip. The aim of the present study was to compare pain during AMSA anesthetic technique with that of the infiltration technique. Friedman and Hochman [2] introduced this technique in 1997 in a case report and claimed that it has a number of advantages.
Several studies evaluated AMSA technique after it was introduced. Some of these studies are mentioned here but none of them has compared AMSA technique with the infiltration technique with the use of a conventional syringe. These two techniques were compared in the present study in the periodontal surgery on the palate. Each of the previous studies has reported a number of advantages for the AMSA technique and has emphasized the use of Wand injection system (Milestone Scientific, Livingston, NJ, USA) for this anesthetic procedure. Since postoperative pain after AMSA technique was less than that with the infiltration technique in the present study, which is considered an advantage for the technique and the pain during this technique was not more severe than that during the infiltration technique, there is overall consistency with the results of previous studies, of which the following studies are mentioned here.
In a study carried out by Yenisey [10] in 2009, the AMSA technique with the use of Wand system was compared with the infiltration technique and the results were evaluated using the verbal rating scale scale. The Wand is a computer-controlled local anesthetic delivery system that drives local anesthetic from a conventional local anesthetic cartridge through plastic microtubing into a plastic handle to which a Luer-Lok needle is attached. The computer-controlled flow is initiated by pressing a foot pedal. The pump allows administration of local anesthetic agent at slow but constant rates, and the computer compensates for variation in resistance to the flow. During needle insertion, continuous positive pressure delivers an anesthetic drip that precedes the needle. The combination of an anesthetic pathway and controlled flow rate results in a virtually imperceptible injection and rapid onset of profound anesthesia [11]. The results showed less pain with the Wand system during needle entry. However, the results of the present study did not reveal any significant differences between these two techniques in this regard. The differences between the results of the two studies might be attributed to the fact that Yenisey used Wand system in his study but conventional syringes were used in the present study.
In a study by Fukayama et al. [7] in 2003 the local anesthesia of maxillary teeth was evaluated using the AMSA system. The results showed that the AMSA technique prevents severe pain during needle entry and during injection and is an effective technique to anesthetize 10 maxillary teeth; however, the AMSA technique was not compared with the infiltration technique.
In a study carried out by Loomer and Perry [5] in 2004 the use of a computer-controlled technique with AMSA was compared with greater palatine and nasopalatine anesthetic techniques. The results revealed a lower VAS for AMSA compared to the other two techniques; a less severe pain with the AMSA in that study was attributed to the use of a computer-controlled injection system. Lee et al. [6] carried out a prospective study in 2004 to compare the two following techniques with AMSA anesthetic procedure.
Lee et al. [6] reported that AMSA is more successful with Wand Plus compared to a conventional syringe, confirming the results of a study carried out by Yenisey. The higher analgesic effects of AMSA technique in the present study confirmed the results of previous studies, too. The severity of postoperative pain with this technique was less than that with the infiltration technique. However, there is controversy over the choice of the best and most effective anesthetic technique. More comprehensive studies and evaluation of various anesthetic techniques in more widespread areas might help dental practitioners choose the best anesthetic technique.
Palatal vault shape was not recorded and evaluated in the present study. However, in retrospect, there is a feeling that in the present study there were, to some extent, normal distribution of shallow and deep vaults. It is possible to evaluate the effect of deep and shallow palatal vaults on the efficacy of AMSA anesthetic technique in a future study. Since a group of young adult subjects were evaluated in the present study, the results might not be extended to children or the elderly.
Postoperative pain with AMSA technique is less severe compared to that with the infiltration technique. Therefore, the technique could be recommended for the anesthesia of palatal tissues in periodontal surgeries given the fact that it has other advantages, too.
Figures and Tables
References
1. Malamed SF. Handbook of local anesthesia. 2004. 5th ed. St. Louis: Mosby.
2. Friedman MJ, Hochman MN. A 21st century computerized injection system for local pain control. Compend Contin Educ Dent. 1997. 18:995–1000. 1002–1003.
3. Friedman MJ, Hochman MN. The AMSA injection: a new concept for local anesthesia of maxillary teeth using a computer-controlled injection system. Quintessence Int. 1998. 29:297–303.
4. Friedman MJ, Hochman MN. Using AMSA and P-ASA nerve blocks for esthetic restorative dentistry. Gen Dent. 2001. 49:506–511.

5. Loomer PM, Perry DA. Computer-controlled delivery versus syringe delivery of local anesthetic injections for therapeutic scaling and root planing. J Am Dent Assoc. 2004. 135:358–365.

6. Lee S, Reader A, Nusstein J, Beck M, Weaver J. Anesthetic efficacy of the anterior middle superior alveolar (AMSA) injection. Anesth Prog. 2004. 51:80–89.

7. Fukayama H, Yoshikawa F, Kohase H, Umino M, Suzuki N. Efficacy of anterior and middle superior alveolar (AMSA) anesthesia using a new injection system: the Wand. Quintessence Int. 2003. 34:537–541.

8. Holtzclaw D, Toscano N. Alternative anesthetic technique for maxillary periodontal surgery. J Periodontol. 2008. 79:1769–1772.

10. Yenisey M. Comparison of the pain levels of computer-controlled and conventional anesthesia techniques in prosthodontic treatment. J Appl Oral Sci. 2009. 17:414–420.
11. Blanton PL, Jeske AH. Dental local anesthetics: alternative delivery methods. J Am Dent Assoc. 2003. 134:228–234.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download