Abstract
Purpose
Special care is necessary to avoid invading important anatomic structures during surgery when presurgical planning is made based on radiographs. However, none of these types of radiography represents a perfect modality. The purpose of this study was to determine the reliability of presurgical planning based on the use of two types of radiographic image (digital panoramic radiography [DPR] and cone-beam computed tomography [CBCT]) by beginner dentists to place implants, and to quantify differences in measurements between radiographic images and real specimens.
Methods
Ten fresh cadavers without posterior teeth were used, and twelve practitioners who had no experience of implant surgery performed implant surgery after 10 hours of basic instruction using conventional surgical guide based on CBCT or DPR. Two types of measurement error were evaluated: 1) the presurgical measurement error, defined as that between the presurgical and postsurgical measurements in each modality of radiographic analysis, and 2) the measurement error between postsurgical radiography and the real specimen.
Results
The mean presurgical measurement error was significantly smaller for CBCT than for DPR in the maxillary region, whereas it did not differ significantly between the two imaging modalities in the mandibular region. The mean measurement error between radiography and real specimens was significantly smaller for CBCT than for DPR in the maxillary region, but did not differ significantly in the mandibular region.
Conclusions
Presurgical planning can be performed safely using DPR in the mandible; however, presurgical planning using CBCT is recommended in the maxilla when a structure in a buccolingual location needs to be evaluated because this imaging modality supplies buccolingual information that cannot be obtained from DPR.
Dental implants have been successfully used for replacing missing teeth with reported success rates of more than 90% [1,2]. Improvements in the surface and design of dental implants have contributed to this remarkable success rates. Recent advances in the radiographic techniques used in implant dentistry have increased the accuracy of presurgical planning [3,4]. However, there exist the risks of nerve injury and maxillary sinus perforation originated from inappropriate presurgical planning due to innate discrepancy between radiographic measurements and real dimensions. Precise radiographic assessment of available alveolar bone and identification of characteristic bone morphology are indispensible for dental implant placement. When posterior maxillary and mandibular sites are considered, the location of important anatomic structures such as the mandibular canal and maxillary sinus should be identified carefully for proper implant site selection and length selection.
Pain or paresthesia caused by inferior alveolar nerve injury is one of major complications. Another major complication is maxillary sinus inferior wall perforation which is known to be correlated with the incidence of infection followed by failure of a dental implant [5,6]. Therefore, special care should be taken not to invade important anatomic structures during surgery when presurgical planning is made based on radiographs. More precise radiographic techniques and corresponding proper computer programs to guide precise surgery would reduce the complication rate [4]. Presurgical planning is mostly made with radiographs such as panoramic, lateral cephalometric, and periapical radiographs, and computed tomography (CT) [7,8]. However, none of these types of radiography represents a perfect modality [9,10]. More accurate radiographic technique is required, especially for presurgical planning in areas where important anatomic structures are located. Finding an appropriate location and measuring the available bone based on panoramic radiograph is one of the most frequently used modalities for presurgical planning. A panoramic radiograph displays the body of the mandible and maxilla, mandibular canal, and maxillary sinus on a single image. The length and mesiodistal angulation of an implant are usually determined in the panoramic radiograph. However, in the anterior area where more distortion exists than posterior area, the reliability of panoramic radiographs for presurgical planning of an implant is questionable [11-13].
The necessity of cross-sectional imaging for a dental implant has been emphasized [14,15]. According to the recommendation from American Academy of Oral and Maxillofacial radiology in 2000, cross-sectional images including conventional spiral tomography, linear tomography, or CT should be used for presurgical planning [16]. These cross-sectional imaging techniques exhibit various accuracies. Linear tomography is reported to be significantly less accurate than spiral tomography in detecting mandibular canal [17]. However, it was reported that measuring available bone volume only using spiral tomography may lead to a dangerous situation because the available vertical bone height is exaggerated in spiral tomography relative to panoramic radiography [12]. CT provides less magnification than the other types of cross-sectional tomography. The magnification in CT corresponds to 0 to 4% [18]. CT can offer direct volumetric reconstruction. Faster and easier data transformation into three-dimensional analysis is possible. In addition, convenient interpretation is also possible without overlapping of images [17]. However, one major disadvantage of CT is a high radiation dose [19], and therefore cone-beam CT (CBCT) was developed to overcome this limitation [20,21]. CBCT images are known to have higher quality than CT images with 1/400 radiation dose of conventional CT [19,20].
Each type of radiograph has its own advantages and disadvantages. Therefore, the radiation dose, magnification rate, and specific indications need to be considered when selecting the type of radiographic images to use in presurgical planning. The purpose of this study was to determine the reliability of presurgical planning based on the use of two types of radiographic image (digital panoramic radiography [DPR] and CBCT) by beginner dentists to place implants.
Ten fresh cadavers without posterior tooth were used to examine the accuracy of CBCT and DPR measurements. These cadavers were from persons who donated their bodies for research or teaching purposes. The posterior teeth were extracted when there is not any missing posterior tooth. Twelve dentists who never had any experience of implant surgery were participated in implant surgery after 10 hours of basic instruction not including hands-on training. Thereafter, each participant performed implant surgery using a conventional surgical guide based on CBCT or DPR on their own. The sites for implant surgery were randomly assigned for the two investigated presurgical planning methods: 31 implants were placed with the surgical guide based on DPR and the corresponding computer program (Starpacs, Infinitt Co., Seoul, Korea), while 32 implants were placed with the surgical guide based on CBCT and the corresponding computer program (Ondemend 3D, Cybermed Inc., Seoul, Korea).
Two types of measurement error were evaluated in this study: 1) The presurgical measurement error: difference between the presurgical and postsurgical measurements in radiographs. 2) The measurement error: difference of measured distances between postsurgical radiographs and the cadaver specimens.
Virtual planning to determine the appropriate length of the implant was first performed using CBCT and the corresponding program. D1 was the difference between the distance from the implant platform to the anatomic structure (e.g., inferior wall of the maxillary sinus or superior border of the mandibular canal) and the distance from the implant platform to the implant apex. D2 was the distance from the implant apex to the anatomic structure in postsurgical CBCT. D3 was the distance from the implant apex to the anatomic structure in the real specimen. The presurgical and postsurgical measurement errors for CBCT were calculated by subtracting D2 from D1 and subtracting D3 from D2, respectively. These measurements are illustrated Figs. 1-3.
Virtual planning to determine the appropriate length of the implant was performed using DPR and the corresponding program. A presurgical panoramic radiograph was obtained to measure the distance from the implant apex to the anatomic structure (D4), which was the difference between the distance from the alveolar ridge to the anatomic structure and the planned implant length. D5 was the distance from the implant apex to the anatomic structure in postsurgical DPR. D6 was the distance from the implant apex to the anatomic structure in a real cross-sectioned specimen. The presurgical and postsurgical measurement errors for DPR were calculated by subtracting D5 from D4 and subtracting D6 from D5, respectively. These measurements are illustrated Figs. 4 and 5.
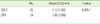
The mean presurgical measurement error was significantly smaller for CBCT than for DPR (P≤0.05) (Table 1). The presurgical measurement error was significantly smaller for CBCT (1.26±1.23 mm) than for DPR (3.32±2.34 mm, P=0.008) in the maxillary region, whereas it did not differ significantly between the two imaging modalities in the mandibular region (1.58±1.25 mm vs. 2.32±1.81 mm, respectively, P=0.164) (Table 2).
The measurement error between postsurgical radiography and cadaver specimens was significantly smaller for CBCT than for DPR (P≤0.05) (Table 3). This difference was statistically significant in the maxillary region (P≤0.05) but not in the mandibular region (1.65±1.24 mm vs. 1.06 ± 0.55 mm, P=0.098) (Table 4).
Some specimens experienced critical errors such as maxillary-sinus invasion, mandibular-canal invasion, and lingual-plate perforation (Fig. 6). The error rate in the implant surgery was higher in DPR than in CBCT.
Statistically significant differences in measurement errors were found between the two radiographic techniques in the present study. This result is consistent with that of previous studies [22,23]. The errors were greater for DPR than CBCT because presurgical plans are made on a two-dimensional plane for DPR. CBCT should be used for presurgical planning and postoperative evaluation, especially when dentists with limited experiences place implants, considering the reduced errors in three-dimensional presurgical planning.
The measurement errors in the maxilla were significantly lower for CBCT than DPR. It can be attributed to the difficulty of identifying the exact location of the inferior wall of the maxillary sinus in presurgical planning when using DPR. Various levels of the inferior border of the maxillary sinus are overlapped in DPR. To the contrary, the exact levels of the inferior border of the maxillary sinus can be identified using CBCT because the view in the specific plane where the implant will be placed is used for presurgical planning. These data suggest that presurgical planning using DPR for implant placement on the maxillary premolar or molar area is not sufficiently reliable. Even though limitation of DPR can be compensated by abundant clinical experiences, more accurate and precise methods are recommended for preventing unexpected complications.
In mandible, the measurement error in CBCT didn't show any statistically significant difference from that in DPR. This result is in accordance with that of one previous study [11]. This shows that there will be fewer errors when presurgical plans are made using DPR in mandible than maxilla. Identifying the superior border of the mandibular canal is easier than the inferior border of the maxillary sinus because the mandibular canal is easy to identify in most cases, except those with thick cortical bone or a high proportion of trabecular bone. This convenient detection of the mandibular canal can allow dentists to place implants in the posterior mandibular area without any critical complications as long as the buccolingual width is measured carefully. Direct measurement using calipers is recommended intraorally or extraorally in a study cast. In summary, presurgical planning in the mandible can be performed safely using DPR by dentists with sufficient experience and skill, whereas presurgical planning using CBCT is strongly recommended when a buccolingual location of the mandibular canal needs to be evaluated.
Radiographic images do not always display anatomic structures accurately. In maxilla, it was revealed that less measurement errors between postsurgical radiographic images and real specimens were found in CBCT than DPR. More accurate detection of the inferior wall of the maxillary sinus was possible using CBCT.
Both positive and negative presurgical measurement errors were obtained, whereas only positive measurement errors were obtained between postsurgical radiographs and real specimens. It appears that the distance from the implant apex to anatomic structures was always greater in a postsurgical radiograph than in the corresponding real specimen.
This study has revealed the best radiographic methods to use in order to reduce errors by beginner dentists during dental implantation. Future studies should evaluate the validity of computer-assisted implant surgery with a surgical guide fabricated based on CBCT. In addition, it is necessary to evaluate the measurement errors when experienced dentists are placing implants.
Figures and Tables
Figure 1
Measurement of D1. D1 was the difference between the distance from the implant platform to the anatomic structure (e.g., inferior wall of the maxillary sinus or superior border of the mandibular canal) in presurgical cone-beam computed tomography and the distance from the implant platform to the implant apex. M: mandibular canal.

Figure 2
Measurement of D2. D2 was the distance from the implant apex to the anatomic structure in postsurgical cone-beam computed tomography. M: mandibular canal.

Figure 3
Measurements of D3 and D6. D3 was the distance from the implant apex to the anatomic structure in the real specimen using cone-beam computed tomography as a guide. D6 was same distance in the real specimen using digital panoramic radiography as a guide.

Figure 4
Measurement of D4. D4 was the difference between the distance from the alveolar ridge to the anatomic structure in presurgical digital panoramic radiography and the planned implant length.

Figure 5
Measurement of D5. D5 was the distance from the implant apex to the anatomic structure in postsurgical digital panoramic radiography.
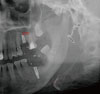
Figure 6
Some critical errors. (A) Maxillary-sinus invasion, (B) mandibular-canal invasion, and (C) lingual-plate perforation.

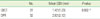
Table 1
Presurgical measurement errors for cone-beam computed tomography (CBCT) and digital panoramic radiography (DPR).
ACKNOWLEDGEMENTS
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2010-0007829) and by a grant of the Korean Health Technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (A100126).
References
1. Albrektsson T, Dahl E, Enbom L, Engevall S, Engquist B, Eriksson AR, et al. Osseointegrated oral implants: a Swedish multicenter study of 8139 consecutively inserted Nobelpharma implants. J Periodontol. 1988. 59:287–296.
2. Misch CE, Perel ML, Wang HL, Sammartino G, Galindo-Moreno P, Trisi P, et al. Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent. 2008. 17:5–15.

3. Van de Velde T, Glor F, De Bruyn H. A model study on flapless implant placement by clinicians with a different experience level in implant surgery. Clin Oral Implants Res. 2008. 19:66–72.

5. Hong YH, Mun SK. A case of massive maxillary sinus bleeding after dental implant. Int J Oral Maxillofac Surg. 2011. 40:758–760.

6. Cho-Lee GY, Naval-Gias L, Castrejon-Castrejon S, Capote-Moreno AL, Gonzalez-Garcia R, Sastre-Perez J, et al. A 12-year retrospective analytic study of the implant survival rate in 177 consecutive maxillary sinus augmentation procedures. Int J Oral Maxillofac Implants. 2010. 25:1019–1027.
7. Scaf G, Lurie AG, Mosier KM, Kantor ML, Ramsby GR, Freedman ML. Dosimetry and cost of imaging osseointegrated implants with film-based and computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997. 83:41–48.

8. Stella JP, Tharanon W. A precise radiographic method to determine the location of the inferior alveolar canal in the posterior edentulous mandible: implications for dental implants. Part 2: Clinical application. Int J Oral Maxillofac Implants. 1990. 5:23–29.
9. Reiskin AB. Implant imaging: status, controversies, and new developments. Dent Clin North Am. 1998. 42:47–56.
10. Sunden S, Grondahl K, Grondahl HG. Accuracy and precision in the radiographic diagnosis of clinical instability in Branemark dental implants. Clin Oral Implants Res. 1995. 6:220–226.
11. Peker I, Alkurt MT, Michcioglu T. The use of 3 different imaging methods for the localization of the mandibular canal in dental implant planning. Int J Oral Maxillofac Implants. 2008. 23:463–470.
12. Frei C, Buser D, Dula K. Study on the necessity for cross-section imaging of the posterior mandible for treatment planning of standard cases in implant dentistry. Clin Oral Implants Res. 2004. 15:490–497.

13. Tal H, Moses O. A comparison of panoramic radiography with computed tomography in the planning of implant surgery. Dentomaxillofac Radiol. 1991. 20:40–42.

14. Bolin A, Eliasson S, von Beetzen M, Jansson L. Radiographic evaluation of mandibular posterior implant sites: correlation between panoramic and tomographic determinations. Clin Oral Implants Res. 1996. 7:354–359.

15. Lindh C, Petersson A, Klinge B. Visualisation of the mandibular canal by different radiographic techniques. Clin Oral Implants Res. 1992. 3:90–97.

16. Tyndall DA, Brooks SL. Selection criteria for dental implant site imaging: a position paper of the American Academy of Oral and Maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000. 89:630–637.

17. Hanazawa T, Sano T, Seki K, Okano T. Radiologic measurements of the mandible: a comparison between CT-reformatted and conventional tomographic images. Clin Oral Implants Res. 2004. 15:226–232.

18. Reddy MS, Mayfield-Donahoo T, Vanderven FJ, Jeffcoat MK. A comparison of the diagnostic advantages of panoramic radiography and computed tomography scanning for placement of root form dental implants. Clin Oral Implants Res. 1994. 5:229–238.

19. Al-Ekrish AA, Ekram M. A comparative study of the accuracy and reliability of multidetector computed tomography and cone beam computed tomography in the assessment of dental implant site dimensions. Dentomaxillofac Radiol. 2011. 40:67–75.

20. Hashimoto K, Arai Y, Iwai K, Araki M, Kawashima S, Terakado M. A comparison of a new limited cone beam computed tomography machine for dental use with a multidetector row helical CT machine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003. 95:371–377.

21. Mozzo P, Procacci C, Tacconi A, Martini PT, Andreis IA. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol. 1998. 8:1558–1564.

22. Kobayashi K, Shimoda S, Nakagawa Y, Yamamoto A. Accuracy in measurement of distance using limited cone-beam computerized tomography. Int J Oral Maxillofac Implants. 2004. 19:228–231.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download