Abstract
Purpose
The aim of this study was to clinically and radiographically evaluate and compare treatment of intrabony defects with the use of decalcified freeze-dried bone allograft in combination with a calcium sulphate barrier to collagen membrane.
Methods
Twelve patients having chronic periodontal disease aged 20 to 50 years and with a probing depth >6 mm were selected. Classification of patient defects into experimental and control groups was made randomly. In the test group, a calcium sulphate barrier membrane, and in control group, a collagen membrane, was used in conjunction with decalcified freeze-dried bone graft in both sides. Ancillary parameters as well as soft tissue parameters along with radiographs were taken at baseline and after 6 months of surgery. Parameters assessed were plaque index, modified gingival index, probing depth, relative attachment level, and location of the gingival margin. A Student's t-test was done for intragroup and a paired t-test for intergroup analysis.
Humans have always struggled directly or indirectly with various oral diseases. Gingival and periodontal diseases, in their various forms, have afflicted humans since the dawn of history. In the 21st century, the goals for periodontal therapy are continually being refined not only to achieve a healthy periodontium but also to recreate a normal anatomic relationship and function. Periodontal therapy has the principle objective of the morphological and functional reconstruction of lost periodontal supporting tissues. However, conventional periodontal therapy has been found to result in repair rather than regeneration, and this process is often characterized by the establishment of long junctional epithelium between the root surface and gingival connective tissue.
The first stage of development of periodontal regeneration methods focused on reconstruction of osseous lesions utilizing a variety of bone replacement grafts. Different types of grafts have been used. Allografts like decalcified freeze-dried bone allograft (DFDBA) showed some promising results, but the ability to regenerate the cementum, periodontal ligament (PDL), and alveolar bone was found to be limited. The era of grafts thus made way for the era of the pioneering technique of guided tissue regeneration (GTR). The placement of the occlusive membrane guides the progenitor cells residing in the PDL to repopulate the osseous defects in order to form new tooth supporting tissues.
Collagen is the primary structural protein of connective tissue [1]. Resorbable collagen membranes have advantages over traditional materials in achieving clot stabilization, wound stability, space provision, and epithelial cell exclusion. When placed in human periodontal defects, calcium sulphate was found to be biocompatible [2]. It is porous and resorbable [3] in nature and it eliminates the need for suturing.
Thus the aim of the present study is to clinically and radiographically evaluate and compare intrabony defect treatment results using DFDBA in combination with a calcium sulphate barrier to collagen membrane.
Twelve patients with chronic periodontal disease aged 20 to 50 years and having three-wall defects with probing depth >6 mm were selected from the patient pool of the Department of Periodontology, Government Dental College and Hospital, Ahmedabad, Gujarat, India. Informed consent was obtained from the patients after explaining to them the nature of the study. The inclusion criteria of the study were all of the following: 1) clinical and radiographic evidence of at least one pair of intrabony defects in two different quadrants, 2) periodontal defects with probing depths greater than or equal to 6 mm, 3) endodontically asymptomatic teeth, 4) patients having adequate gingival coverage in selected teeth, and 5) a defect depth of at least 3 mm as detected on the radiographs.
After reevaluation of the phase I therapy, patients with any of the following were excluded from the study: 1) patients who were medically compromised or on any drug therapy, which may influence the healing of tissues, 2) smoking or use of other tobacco products, 3) unacceptable oral hygiene habits, 4) history of previous treatment by open debridement and/or regenerative therapy at the same site.
At phase I therapy, thorough scaling and root planing was done and oral hygiene instructions were given. Customized acrylic occlusal stents with vertical grooves were prepared for each patient on their respective study cast to record the direction of insertion of the periodontal probe interproximally and to standardize it for future measurements. Classification of defects in patients as experimental or control was done at this time. Sites were classified randomly as test (t) or control (c).
Parameters were recorded at baseline, 3 months, and 6 months postoperatively to evaluate the soft tissue response using the same periodontal probe. The parameters assessed were plaque index [4], modified gingival index [5], probing depth, relative attachment level (RAL), and location of the gingival margin. Radiographic evaluation [6] was done preoperatively and 6 months postoperatively by using the long cone paralleling technique in the field of interest. An indigenously developed standardized X-ray grid was placed in front of the intraoral periapical film on a film holder and an X-ray was taken of the selected teeth.
All patients were prescribed to take 100 mg doxycycline a day in capsule form before surgery and continue to take the same medicine postoperatively. The surgical area was anesthetized using 2% lidocaine hydrochloride with adrenaline (1:80,000). Sulcular incisions were made aimed at preserving as much of the interproximal tissue as possible by using a no. 15 Bard-Parker blade and mucoperiosteal flaps were raised at the buccal and lingual aspects to expose the 3 to 4 mm alveolar process. The inner surfaces of the flaps were curetted, taking care not to thin them excessively and hence compromise the blood supply to the healing wound. A thorough debridement of the defects was done and the exposed root surfaces were thoroughly planed to a smooth hard surface. After hydration of the graft (DFDBA, Dembone, Pacific Coast Tissue Bank, Los Angeles, CA, USA) particles in physiologic saline, they were incrementally condensed into the defect. Overfilling of the defect was avoided. Interrupted interdental presuturing was done with 3.0 Mersilk suture material.
Following graft placement, a bioresorbable collagen membrane (Progide, equinox, Zeist, Holland) was trimmed and adapted over the entire defect on the control site so as to cover 2 to 3 mm of surrounding alveolar bone and to ensure stability of the graft material. On the experimental site, a calcium sulphate (DentoGen-Calcium Sulphate Hemihydrate, Biodenix Technologies Inc., Richmond, CA, USA) barrier was applied. The barrier material was prepared by mixing the calcium sulphate powder in the sterile box with the liquid provided by the company. The ideal mix was dry enough to clump together but wet enough to spread with an instrument when positioned on the bone graft surface. A dry surgical field was very important at this stage. The mix was then placed over the graft. The barrier should be 1.5- to 2-mm thick. It should cover all of the bone graft particles and extend on to the surrounding bone for an additional 2 to 3 mm. A total soft tissue primary closure was obtained by using 3-0 sutures in interrupted fashion. A periodontal dressing was used to cover the treated sites.
Postoperatively subjects were prescribed 100 mg doxycycline twice on first day and once daily for another 9 days after completion of surgery, and 400 mg analgesic ibuprofen three times a day for 5 days. Rinsing with 0.2% chlorhexidine digluconate solution twice daily for 4 weeks was also mandatory. They were advised to avoid hard chewing on the surgical area for 10 days. Pack and suture removal was done on the 10th day.
The data obtained from the present study was suitably tabulated in appropriate tables. The Student's t-test and paired t-test were applied to achieve the level of significance, whenever indicated. The mean and standard deviation were calculated at 3 months only to show the trends over time. For between-group comparison from baseline to 3 months, the Student's t-test was used. These t-test values were compared with table values to determine the level of significance.
Wound healing was uneventful for all treated cases. Soft tissues healed within normal limits and no significant visual differences were noted between the treatment groups. A statistically significant reduction was noted in the plaque score and gingival inflammation in both test and control groups (Table 1). Between the groups, there is no statistically significant (P>0.05) difference in probable pocket depth (PPD) reduction, as both the groups show similar results. There is no statistically significant (P>0.05) difference in mean RAL gain (Table 2) and mean gingival margin level (Table 3) as both the groups show similar results. There is a statistically significant (P<0.01) increase in defect fill from before surgery to 6 months in both the treatment groups (Table 4) (Figs. 1-4).
For many years, periodontology has been taken as a branch dealing with treatment strategies for attempting to save dentition suffering from periodontitis, and history has shown that our profession has been successful, to some extent.
The evidence of previous literature has shown that osseous grafting techniques represent one of the modes of therapy for managing the combination of pocket and osseous defects. Also, the biological and histological aspects of guided tissue regeneration (GTR) have been established through plenty of animal and human studies. Collagen membrane is one of the most commonly used resorbable membranes, as it is the basic structural unit of connective tissue. It has also the ability to aggregate platelets. Collagen membranes have been found to have the property of clot stabilization, wound stability, space provision [7], and epithelial cell exclusion which are important factors determining tissue regeneration when a barrier technique is used.
In 1975, Frame [3] listed the following properties of an ideal biodegradable bone implant material: 1) acceptance by the tissues with no untoward reactions, 2) porosity to allow some bone in-growth, 3) biodegradability to preclude areas of weakness or possible infection after the new bone has beenformed, 4) ability to be sterilized without a change in its properties, 5) availability and minimal cost. He identified calcium sulphate as such a material.
The use of calcium sulphate as a barrier membrane for GTR has been established by various clinical reports. Calcium sulphate retards epithelial and connective tissue in-growth to produce a predictable regenerative response [7]. It shows a lack of infection if the material becomes exposed. The material adapts very well and adheres to the root surface, including root concavities [8]. Above all, it is readily available, easily sterilized, inexpensive, completely resorbable, and biocompatible, and in the presence of bone and periosteum, it becomes osteogenic. Also, it has been found that the compressive strength of calcium sulphate is greater than that of cancellous bone with a resorbable capacity of 5 to 7 weeks [9].
Opinions on the effectiveness of DFDBA as a bone implant to augment GTR is varied [10,11]. DFDBA has been used during GTR procedures because it is thought to be a space maintainer and to enhance periodontal tissue regeneration by its osteoinductive properties. Urist and Strates [11] reported that the addition of bone grafting materials resulted in significantly greater pocket depth reduction than in the membrane group only.
Thus, in the present study we have used calcium sulphate as a barrier membrane along with DFDBA as a test group in comparison to collagen membrane along with DFDBA as a control group.
Ancillary parameters were employed to monitor periodontal condition throughout the study namely, the Plaque Index [4] and Modified Gingival Index [5].
All soft tissue parameters were measured from the lower border of a customized acrylic stent covering the occlusal surface of the teeth. The acrylic stent was shown to provide a stable, fixed reference point [12] for measurements as compared to the cemento-enamel junction, which is often obscured by calculus or soft tissues and difficult to locate clinically. Moreover, the occlusoapical groove helped to standardize the direction of probe insertion.
In the present study, the initial mean probing depths between the groups were not significantly different (Table 1). After 6 months, the results showed a statistically significant (P<0.01) reduction in probing depth in both treatment groups because of resolution of inflammation. This result showed a statistically significant PPD reduction from baseline to 6 months in the two groups. The findings of this study are in accordance with similar studies conducted by Orsini et al. [13] and Paolantonio et al. [14]. Similar results were also observed in studies conducted by Trejo et al. [15], Aichelmann-Reidy et al. [16], and Vouros et al. [17].
RAL assessments, made from a fixed reference point (lower border of stent) have the advantage of being a more realistic portrayal of attachment gain or loss than PPD, as they are not influenced by gingival margin changes. The RAL is different from the clinical attachment level, but is recommended for clinical studies due to its ease and reproducibility [18]. In the present study, the RAL gain was statistically significant (Table 2) in both treatment groups after 6 months. The results were analogous to a study by Orsini et al. [13], Paolantonio et al. [14], Trejo et al. [15], Aichelmann-Reidy et al. [16], and Vouros et al. [17], Zybutz et al. [19].
The gingival recession (Table 3) noted in the present study was 0.43±0.14 mm for the test site and 0.51±0.14 mm for the control site. Recession at the test site was not significantly different from that of the control site (P>0.05). The reduction in the size of the gingiva was attributed to resolution of inflammation (shrinkage) after healing. The results were in accordance with the results of studies done by Paolantonio et al. [14], Trejo et al. [15], Aichelman-Reidy et al. [16], and Vouros et al. [17].
Radiographic changes in bone were assessed by taking serial radiographs exposed with a standardized millimetre grid. Using such a grid provides an accurate way of assessing changes in bone height less than 1 mm. Measurements were made from the crest of the defect to the base of the defect so as to calculate the defect depth (difference of two measurements). The radiographic picture (Table 4) in the present study shows gain or defect fill at the test and control site (P<0.01). These results were analogous to those of Trejo et al. [15], Aichelmann-Reidy et al. [16], Zybutz et al. [19], and Zitzmann et al. [20].
The radiographic findings confirm the clinical findings of the soft tissue response. Despite a lack of concrete evidence of regeneration, the radiographic parameters provided a noninvasive means of evaluating the effect of calcium sulphate/DFDBA and collagen membrane/DFDBA, as compared to histologic analysis, which is rarely possible in human subjects due to ethical constraints. The improvements in parameters show that both the groups, calcium sulphate/DFDBA and collagen membrane/DFDBA, experienced significant benefits with the periodontal grafting materials.
The intergroup statistical analysis showed no statistically significant differences (P>0.05) in the results between the groups, as the calcium sulphate/DFDBA group showed almost the same results as that of the collagen membrane/DFDBA group after 6 months in terms of all of the parameters.
All of the above-mentioned comparable results achieved by calcium sulphate/DFDBA compared to collagen membrane/DFDBA indicated that calcium sulphateis as efficacious as that of collagen membrane as a barrier material. It holds a great promise for improved clinical performance and can be used as a cost-effective replacement for collagen membrane.
Figures and Tables
Figure 1
Preoperative radiograph showing defect site prior to treatment with calcium sulphate barrier and decalcified freeze-dried bone allograft.

Figure 2
Postoperative radiograph showing defect fill after undergoing treatment with calcium sulphate barrier and decalcified freeze-dried bone allograft.
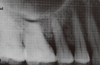
Figure 3
Preoperative radiograph showing defect site prior to treatment with collagen and decalcified freeze-dried bone allograft.

Figure 4
Postoperative radiograph showing defect fill after undergoing treatment with collagen membrane and decalcified freeze-dried bone allograft.

Table 1
Comparison of mean probable pocket depth reduction at baseline to 6 months postoperatively between the groups (mm).

Table 2
Comparison of mean relative attachment level at baseline to 6 months post operatively between the groups (mm).

References
1. Bunyaratavej P, Wang HL. Collagen membranes: a review. J Periodontol. 2001. 72:215–229.
2. Shaffer CD, App GR. The use of plaster of paris in treating infrabony periodontal defects in humans. J Periodontol. 1971. 42:685–690.
3. Frame JW. Porous calcium sulphate dihydrate as a biodegradable implant in bone. J Dent. 1975. 3:177–187.

4. Turesky S, Gilmore ND, Glickman I. Reduced plaque formation by the chloromethyl analogue of victamine C. J Periodontol. 1970. 41:41–43.

5. Lobene RR, Weatherford T, Ross NM, Lamm RA, Menaker L. A modified gingival index for use in clinical trials. Clin Prev Dent. 1986. 8:3–6.

6. Reddy MS. Radiographic methods in the evaluation of periodontal therapy. J Periodontol. 1992. 63:12 Suppl. 1078–1084.

7. Sottosanti J. Calcium sulfate: a biodegradable and biocompatible barrier for guided tissue regeneration. Compendium. 1992. 13:226–228. 230232–234.

8. Anson D. Calcium sulfate: a 4-year observation of its use as a resorbable barrier in guided tissue regeneration of periodontal defects. Compend Contin Educ Dent. 1996. 17:895–899.

9. Sukumar S, Drizhal I, Paulusova V, Bukac J. Surgical treatment of periodontal intrabony defects with calcium sulphate in combination with beta-tricalcium phosphate: clinical observations two years post-surgery. Acta Medica (Hradec Kralove). 2011. 54:13–20.

10. Blumenthal N, Steinberg J. The use of collagen membrane barriers in conjunction with combined demineralized bone-collagen gel implants in human infrabony defects. J Periodontol. 1990. 61:319–327.

11. Urist MR, Strates BS. Bone formation in implants of partially and wholly demineralized bone matrix. Including observations on acetone-fixed intra and extracellular proteins. Clin Orthop Relat Res. 1970. 71:271–278.

12. Clark DC, Chin Quee T, Bergeron MJ, Chan EC, Lautar-Lemay C, de Gruchy K. Reliability of attachment level measurements using the cementoenamel junction and a plastic stent. J Periodontol. 1987. 58:115–118.

13. Orsini M, Orsini G, Benlloch D, Aranda JJ, Lazaro P, Sanz M, et al. Comparison of calcium sulfate and autogenous bone graft to bioabsorbable membranes plus autogenous bone graft in the treatment of intrabony periodontal defects: a split-mouth study. J Periodontol. 2001. 72:296–302.

14. Paolantonio M, Perinetti G, Dolci M, Perfetti G, Tete S, Sammartino G, et al. Surgical treatment of periodontal intrabony defects with calcium sulfate implant and barrier versus collagen barrier or open flap debridement alone: a 12-month randomized controlled clinical trial. J Periodontol. 2008. 79:1886–1893.

15. Trejo PM, Weltman R, Caffesse R. Treatment of intraosseous defects with bioabsorbable barriers alone or in combination with decalcified freeze-dried bone allograft: a randomized clinical trial. J Periodontol. 2000. 71:1852–1861.

16. Aichelmann-Reidy ME, Heath CD, Reynolds MA. Clinical evaluation of calcium sulfate in combination with demineralized freeze-dried bone allograft for the treatment of human intraosseous defects. J Periodontol. 2004. 75:340–347.

17. Vouros I, Aristodimou E, Konstantinidis A. Guided tissue regeneration in intrabony periodontal defects following treatment with two bioabsorbable membranes in combination with bovine bone mineral graft. A clinical and radiographic study. J Clin Periodontol. 2004. 31:908–917.

18. Caton JG, Greenstein G. Factors related to periodontal regeneration. Periodontol 2000. 1993. 1:9–15.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download