Abstract
Purpose
The main purpose of this study was to investigate bone thickness on the buccal and palatal aspects of the maxillary canine and premolars using cone-beam computed tomography (CBCT). The differences between left- and right-side measurements and between males and females were also analyzed.
Methods
The sample consisted of 20 subjects (9 males and 11 females; mean age, 21.9±3.0) selected from the normal occlusion sample data in the Department of Orthodontics, The Catholic University of Korea. The thickness of the buccal and palatal bone walls, perpendicular to the long axis of the root were evaluated at 3 mm and 5 mm apical to cemento-enamel junction (CEJ) and at root apex.
Results
At the canines and first premolars regions, mean buccal bone thickness of at 3 mm and 5 mm apical to CEJ were less than 2 mm. In contrast, at the second premolar region, mean buccal bone thickness at 3 mm and 5 mm apical from CEJ were greater than 2 mm. Frequency of thick bone wall (≥2 mm) increased from the canine to the second premolar.
In recent years, immediate implant placement after tooth extraction has become a procedure that is being performed routinely. Immediate implant placement has many advantages including fewer surgical procedures, shorter treatment time, higher patient acceptance, less psychological stress and improved esthetics [1]. Dental implants which are placed immediately into carefully selected sites have high survival rates comparable to implants placed in healed sites [1,2].
It was previously suggested that immediate implant placement might preserve buccal and lingual bone at the extraction site [3], and some authors have recommended that implant placement should be performed immediately after extraction of teeth to preserve bone at the site of extraction [4,5]. However, a number of studies have demonstrated that alveolar ridge resorption could not be prevented by immediate implant placement [6-8]. Marked buccal bone plate resorption relative to the lingual plate was observed following implant placement in fresh extraction sockets [9]. After these observations, it has been reported that there was a significant association between the width of the buccal bone plate and extent of bone resorption. This report suggested that the width of the buccal bone plate should be at least 2 mm to maintain the alveolar bone level [10].
Recently, cone-beam computed tomography (CBCT) has been brought into widespread use in dentistry and it has been applied for periodontal evaluations, endodontics and dentoalveolar trauma evaluations [11,12]. Dental practitioners obtained information to evaluate hard and soft tissue for possible dental implant placement [13,14].
Maxillary anterior region has esthetic importance on immediate implant placement. Buccal and palatal bone thickness of maxillary central and lateral incisors has been evaluated with CBCT by many researchers [15-17]. Maxillary premolar region is also important for esthetics but relatively few studies have been conducted for the premolar region [15]. The main purpose of this study was to investigate the bone thickness on buccal and palatal aspect of maxillary canine and premolars using CBCT. Additional purpose of this study was to investigate the differences between left- and right-side measurements and between males and females. Within the authors' knowledge, this is the first study to evaluate the bone thickness of maxillary premolars in the sample population with normal occlusion.
The investigation consisted of 20 subjects (9 males and 11 females; mean age, 21.9±3.0) selected from the normal occlusion sample data in the Department of Orthodontics, The Catholic University of Korea. Subjects were selected from 480 Korean students (mean age, 24.3 years; range, 19.1 to 34.6 years) at Wonkwang University. The inclusion criteria were 1) periodontally healthy dentition; 2) normal occlusion; and 3) a preorthodontic treatment state. Normal occlusion was defined as 1) Angle Class I occlusion; 2) fully developed permanent dentition with a normal overbite and overjet between 1 mm and 3 mm; 3) no missing or decayed teeth; 4) no prosthetic crowns; 5) crowding less than 3 mm and spacing less than 1 mm; 6) no facial asymmetry with crossbite. A sample of 40 maxillary canines, 40 maxillary first premolars, and 40 maxillary second premolars were included in the study. This study was approved by the Institutional Review Board of The Catholic University of Korea.
Three-dimensional CBCT scans were acquired with VEGA (Asahi Roentgen Ind. Co., Ltd., Kyoto, Japan) with a 200×179-mm field of view, 80 kVp, and 50 mA, resulting in 0.39-voxel resolution. The obtained data were exported from the iCAT software in DICOM format into the InvivoDental 5 program (Anatomage, San Jose, CA, USA), and 3-D reconstructions were generated. Sagittal slices were produced at the center of the bilateral maxillary canines and first and second premolars. The slice location passed through the center of the root, parallel to the long axis of the root.
Image measurement was performed by two examiners (SHJ, SP) at the same slice of the image. The long axis ran from the tip of the cusp to the root apex in the canines and from the central groove to the root apex in the premolar teeth (Fig. 1A and B). When two roots existed in premolar teeth, the buccal cusp and buccal root apex were used as the long axis line (Fig. 1C). For the reference point, the line from the buccal cemento-enamel junction (CEJ) to the palatal CEJ (CEJ line) was used. The CEJ point was defined as the intersection between the long axis and the CEJ line. The thickness of the buccal and palatal bone walls perpendicular to the long axis of the root were evaluated at 3 mm and 5 mm apical from the CEJ point and at root apex.
The correlations between left- and right-side measurements and between males and females were analyzed with commercially available software SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). The level of significance was considered to be 0.05. Internal consistency between the examiners was evaluated by coefficient α and minimum acceptable score for internal consistency was 0.7. If α was ≥0.9, it was considered excellent [18].
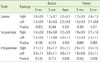
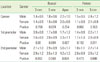
Buccal bone thickness at 3 mm and 5 mm apical from the CEJ and at the root apex, and palatal bone thickness at 3 mm and 5 mm from the CEJ is reported in Table 1. At the canine and first premolar regions, the mean buccal bone thickness at the 3 mm and 5 mm positions from the CEJ were below 2 mm. In contrast, at the second premolar region, the mean buccal bone thickness at 3 mm and 5 mm from the CEJ were greater than 2 mm. At the root apex, the mean buccal bone thickness at all three teeth positions were greater than 2 mm.
The frequency distribution (%) of buccal bone thickness at 3 mm and 5 mm from the CEJ and at the apex is shown in Table 2, and the frequency distribution of the palatal bone wall thickness examined at 3 mm and 5 mm from the CEJ is shown in Table 3. The frequency distribution of thick bone wall (≥2 mm) increased from the canine to the second premolar at 3 mm and 5 mm from the CEJ (Figs. 2 and 3). However, the thick bone wall (≥2 mm) at the root apex showed almost the same frequency in the canines and first premolar teeth (Fig. 4).
For the canines, the buccal bone thickness at 3 mm and 5 mm from the CEJ of most teeth was less than 2 mm. The bone thicknesses of only 12.5% (at 3 mm from the CEJ) and 25.0% (at 5 mm from the CEJ) of the canines were greater than 2 mm. However, in about half of the cases (51.2%), the buccal bone thickness at the root apex was equal to or greater than 2 mm. Only 21.2% of the first premolars showed a buccal bone thickness greater than 2 mm at 3 mm from the CEJ. However, at 5 mm from the CEJ, 42.5% of the first premolars presented with buccal bone thickness above 2 mm. Similarly, in canines, the frequency of teeth with buccal bone thickness ≥2 mm at the root apex was 50.0%. For the second premolars, 68.8% of buccal bone thickness measurements at 3 mm from CEJ were greater than 2 mm. The majority of the buccal bone thickness measurements at 5 mm apical to the CEJ and root apex were greater than 2 mm (90.0% and 97.5%). The mean buccal bone thickness at 3 mm from the CEJ increased from the canine to the second premolar. Similar trends were seen in the mean palatal bone thickness at 3 mm from the CEJ.
No significant difference between left and right was found from the bone thickness measurements (Table 4). The overall measurements of the bone thickness did not show significant male/female differences (Table 5). However, a significantly higher buccal bone thickness at 3 mm from the CEJ was observed in females than males in first and second premolars.
Internal consistency between the two examiners was excellent. Statistical analysis showed excellent internal consistency among the teeth overall (α=0.978) as well as in each type of tooth (Table 6).
The main purpose of the present study was to determine the thickness of the buccal bone in different locations apical to the CEJ in normal occlusion subjects. In this study, alveolar bone thickness was measured in normal occlusion samples. A few studies have reported that certain malocclusion groups had greater bone loss around specific teeth than was seen in normal occlusion samples [19]. Furthermore, alveolar bone thickness at the root apex was significantly greater in the normal occlusion samples than certain malocclusion groups [20].
It is important to investigate the thickness of buccal bone for implant installation and whether the bone thickness is greater than 2 mm is of crucial importance for selecting the appropriate treatment approach. Mean buccal resorption was reported to be significantly greater when the ridge width was <2 mm than with a wider ridge [10]. It was suggested that the buccal bone should be at least 2 mm in thickness to ensure proper soft tissue support and to avoid resorption following restoration [15]. Moreover, there was no statistically significant difference in the implant failure rate in groups with less than 1 mm or with 1 to 2 mm of labial bone thickness; however, significantly less implant failure was seen in the group with at least 2 mm of labial bone thickness [21,22]. The mean thickness of buccal bone and occurrence of ≥2 mm thick bone measurements increased with increasing depth. This may be related to the shape of the root, resulting in reduced diameter of the roots toward the apex [17]. The frequency of thick bone wall (≥2 mm) showed an increase from the canine to the second premolar. The mean buccal bone thickness was ≥2 mm in the second premolar region and bone resorption following tooth extraction is expected to be less than that of the canine and first premolar.
Januario et al. [16] reported the dimensions of the facial bone wall in the anterior maxillary area (central incisor, lateral incisor, and canine) using CBCT. In their study, the mean buccal bone thickness of the canine at 1, 3, and 5 mm apical to the bone crest was reported to be <1 mm, but according to our measurements, the mean buccal bone thickness was >1 mm at the canine and premolar area. The difference may be from the type of occlusion (normal occlusion in this study and no restrictions on occlusion in Januario's study) and age (18 to 31 for this study vs. 17 to 66 for study done by Januario et al.).
In this study, bone thickness was measured starting at 3 mm from the CEJ. Many authors have suggested vertical depth guidelines for the placement of the fixture and the head of the fixture must be located approximately 2 mm to 3 mm from the natural CEJ of the adjacent teeth, according to these guidelines [23,24]. From the perspective of immediate implant placement, buccal bone thickness at the root apex is also an important factor. Immediate implant placement should be performed over the apex for the maximum primary stability and proper alignment [25,26]. Because of the thin buccal bone plate at the root apex and of buccal slipping in routine drilling, the thin buccal cortical bone may be damaged easily. In our study, at the canine and first premolar area, the mean buccal bone thickness of the root apex was approximately 2 mm. In contrast, the second premolar area had almost twice the buccal bone thickness of the canine and first premolar area, making it safer for implant placement.
The topology (right and left side) and gender did not influence the overall measurements. However, significantly higher buccal bone thickness at 3 mm from the CEJ was observed in females than males at the first and second premolars. This may be related to the bucco-lingual dimensions, and previous reports have found that males had greater bucco-lingual dimensions of teeth than females, with the maxillary canine and first premolar exhibiting statistically significant dimorphism [27].
In conclusion, this study investigated bone thickness on the buccal and palatal aspects of the maxillary canine and premolars using CBCT in subjects with normal occlusion. The alveolar bone thickness at the canine and first premolar in the maxilla was lower than 2 mm and there was relatively thick alveolar bone in the second premolar area compared to that of the canine and first premolar area in the maxilla, which may be relatively safe for immediate implant placement. This result should be considered before tooth extraction and planning of rehabilitation in the canine and premolar area of the maxilla. Careful preoperative analysis with CBCT may be beneficial in diagnosis to assess local risk factors and to achieve high predictability.
Figures and Tables
Figure 1
(A) Buccal bone thickness of canine at 3 mm and 5 mm from the cemento-enamel junction (CEJ) and at the root apex. (B) Buccal bone thickness of the premolar at 3 mm and 5 mm from the CEJ and at the root apex. (C) The buccal cusp and buccal root apex were used as the long axis line when two roots existed.

References
1. Bhola M, Neely AL, Kolhatkar S. Immediate implant placement: clinical decisions, advantages, and disadvantages. J Prosthodont. 2008. 17:576–581.

2. Attard NJ, Zarb GA. Immediate and early implant loading protocols: a literature review of clinical studies. J Prosthet Dent. 2005. 94:242–258.

3. Werbitt MJ, Goldberg PV. The immediate implant: bone preservation and bone regeneration. Int J Periodontics Restorative Dent. 1992. 12:206–217.
4. Barzilay I. Immediate implants: their current status. Int J Prosthodont. 1993. 6:169–175.
5. Froum SJ. Immediate placement of implants into extraction sockets: rationale, outcomes, technique. Alpha Omegan. 2005. 98:20–35.
6. Covani U, Cornelini R, Barone A. Bucco-lingual bone remodeling around implants placed into immediate extraction sockets: a case series. J Periodontol. 2003. 74:268–273.

7. Botticelli D, Berglundh T, Lindhe J. Hard-tissue alterations following immediate implant placement in extraction sites. J Clin Periodontol. 2004. 31:820–828.

8. Araujo MG, Sukekava F, Wennstrom JL, Lindhe J. Ridge alterations following implant placement in fresh extraction sockets: an experimental study in the dog. J Clin Periodontol. 2005. 32:645–652.

9. Araujo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005. 32:212–218.

10. Qahash M, Susin C, Polimeni G, Hall J, Wikesjo UM. Bone healing dynamics at buccal peri-implant sites. Clin Oral Implants Res. 2008. 19:166–172.

11. Miracle AC, Mukherji SK. Conebeam CT of the head and neck, part 2: clinical applications. AJNR Am J Neuroradiol. 2009. 30:1285–1292.

12. Kaya S, Adiguzel O, Yavuz I, Tumen EC, Akkus Z. Cone-beam dental computerized tomography for evaluating changes of aging in the dimensions central superior incisor root canals. Med Oral Patol Oral Cir Bucal. 2011. 16:e463–e466.
13. Howerton WB Jr, Mora MA. Advancements in digital imaging: what is new and on the horizon? J Am Dent Assoc. 2008. 139:Suppl. 20S–24S.
14. Yilmaz HG, Tozum TF. Are gingival phenotype, residual ridge height, and membrane thickness critical for the perforation of maxillary sinus? J Periodontol. 2012. 83:420–425.

15. Braut V, Bornstein MM, Belser U, Buser D. Thickness of the anterior maxillary facial bone wall-a retrospective radiographic study using cone beam computed tomography. Int J Periodontics Restorative Dent. 2011. 31:125–131.
16. Januario AL, Duarte WR, Barriviera M, Mesti JC, Araujo MG, Lindhe J. Dimension of the facial bone wall in the anterior maxilla: a cone-beam computed tomography study. Clin Oral Implants Res. 2011. 22:1168–1171.

17. Ghassemian M, Nowzari H, Lajolo C, Verdugo F, Pirronti T, D'Addona A. The thickness of facial alveolar bone overlying healthy maxillary anterior teeth. J Periodontol. 2012. 83:187–197.

18. Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994. 151:1132–1136.

19. Kim Y, Park JU, Kook YA. Alveolar bone loss around incisors in surgical skeletal Class III patients. Angle Orthod. 2009. 79:676–682.

20. Kook YA, Kim G, Kim Y. Comparison of alveolar bone loss around incisors in normal occlusion samples and surgical skeletal class III patients. Angle Orthod. 2012. 82:645–652.

21. Spray JR, Black CG, Morris HF, Ochi S. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol. 2000. 5:119–128.

22. Cho YB, Moon SJ, Chung CH, Kim HJ. Resorption of labial bone in maxillary anterior implant. J Adv Prosthodont. 2011. 3:85–89.

23. Funato A, Salama MA, Ishikawa T, Garber DA, Salama H. Timing, positioning, and sequential staging in esthetic implant therapy: a four-dimensional perspective. Int J Periodontics Restorative Dent. 2007. 27:313–323.
24. Salama H, Salama MA, Garber D, Adar P. The interproximal height of bone: a guidepost to predictable aesthetic strategies and soft tissue contours in anterior tooth replacement. Pract Periodontics Aesthet Dent. 1998. 10:1131–1141.
25. Gelb DA. Immediate implant surgery: three-year retrospective evaluation of 50 consecutive cases. Int J Oral Maxillofac Implants. 1993. 8:388–399.
26. Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989. 9:332–343.
27. Prathibha Rani RM, Mahima VG, Patil K. Bucco-lingual dimension of teeth: an aid in sex determination. J Forensic Dent Sci. 2009. 1:88–92.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download