Abstract
Purpose
The aim of this study was to obtain objective and standardized information on masticatory function and patient satisfaction following second molar single implant therapy.
Methods
Twenty adult patients, who had restored second molar single implants more than 1 month before the study, were enrolled in this study. All patients received a chewing test using peanuts before and after insertion of the implant prosthesis, with a questionnaire and visual analogue scale (VAS) to evaluate the effect of second molar single implant therapy.
Results
This study obtained standardized information on the masticatory function objectively (e.g., P, R, X50) before (Pre-insertion) and after insertion (Post-insertion) of the implant prosthesis. Masticatory performance (P) after insertion of the implant prosthesis significantly increased from 67.8±9.9 to 84.3±8.5% (P<0.0001). With the implant prosthesis, the P value increased by 24%. The masticatory efficiency index (R) of Post-insertion is higher than that of Pre-insertion (P<0.0001). With the implant prosthesis, the R value increased by 29%. The median particle size (X50) of Post-insertion is lower than that of Pre-insertion (P<0.0001). More than 90% of the patients were satisfied with the second molar single implant therapy from a functional point of view.
When a missing tooth is located at the distal free-end, there are only a few treatment options: a conventional fixed partial denture or single implantation [1].
If this type of missing tooth is treated in conventional fixed partial denture therapy, the cantilever has a leverage effect on the second premolar [1]. Many studies have suggested that an implant is a satisfactory choice for posterior single tooth restorations with a good prognosis [2-8]. Becker and Becker [4] reported the results of treatment for single molar replacements. For two years, a 95.7% success rate was shown. Levin et al. [5] reported that the overall survival rate of single molar implants was 92.6%, at an average of 36 months of follow-up. Jung et al. [6] reported that the cumulative survival rate of the second molar single implant was 93.93%.
Unless the missing second molar is restored, complications may occur such as supra-eruption of the opposing tooth [1,9]. Extrusion of an opposing molar may disrupt occlusion [9]. This situation may lead to periodontal problems or heightened risk of caries development [9]. Some have reported that loss of a post-canine tooth results in a loss of chewing ability [10,11]. Others reported that there was not impaired masticatory function when the patient had more than 20 well-distributed teeth [11,12]. Nevertheless, few researchers have focused on the masticatory function with objective parameters in replacing a posterior tooth with a freestanding single implant.
Masticatory function can be evaluated in subjective and objective measures: first, masticatory ability (subjective measure obtained from questionnaires and personal interviews) and second, masticatory performance and masticatory efficiency (objective measure obtained from chewing tests), have been used [11-13]. Masticatory performance is calculated by evaluating the particle size distribution of food when chewed for a given number of strokes. Masticatory efficiency can be assessed by counting the number of masticatory strokes required to reduce food to a certain particle size [11-13]. Masticatory performance has often been measured by determining an individual's capacity to grind or pulverize a test food [10-28]. Masticatory ability assesses a subjective chewing satisfaction [12,22,29].
Most masticatory function studies deal with conventional dentures, implant-supported overdentures and full-arch implant prostheses [11,12,18,25-28,30], whereas a limited number of studies on single implant restoration have been performed [31]. The purpose of this study was to obtain objective and standardized information on masticatory function and patient satisfaction following second molar single implant therapy.
The study covered all patients who were treated with a second molar single implant during the period of July 1, 2002, until August 19, 2009 in the Department of Periodontics, Gangneung-Wonju National University Dental Hospital. Of 114 patients who were screened and treated with a most posterior single implant during this period, 20 patients were recruited (Table 1).
Patients were selected according to the following inclusion criteria: agreement of patient to participate in this chewing test, patient's cooperation status permitting a periodic follow-up, absence of malocclusion, and presence of an opposing tooth with normal periodontal support.
Three implant systems were used, and they are summarized in Table 2.
All implant restorations had gold occlusal surfaces, and the opposing dental status was composed of 7 gold crowns and 13 natural teeth.
All patients were thoroughly informed about the procedure and gave written consent for inclusion in the study. This study was approved by the Institutional Review Board of Gangneung-Wonju National University Dental Hospital (IRB2009-14-1).
The objective masticatory function of the patients was tested with a method using peanuts and an internationally-accepted standard sieve system with filter paper (Whatman Cat No. 1001, Whatman plc, Brentford, UK) before and after insertion of the implant prosthesis (Fig. 1). Peanuts were dried under 60℃ in an incubator for 24 hours. 3.0 g of peanuts were used in the chewing test. Each patient was asked to chew peanuts on the implant side for 20 masticatory strokes. The chewed test portions were expectorated into a paper cup and the patients rinsed their mouth three times with water and spit the remains into a paper cup again. The chewed samples were washed through a stack of 5 sieves of 2.0, 1.0, 0.71, 0.5, and 0.25 mm aperture. While the particles were being washed through the sieve, the sieves were agitated by a dental vibrator set at half speed for 2 minutes. Each sieve was then washed individually with a bottle of water. The particles that were in size between two successive sieves that form an upper and lower boundary was collected and denoted as a size fraction. Each size fraction of particles was dried at 60℃ in an incubator for 24 hours and then weighed.
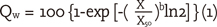
The weight of the particles on each sieve can be represented in a plot which shows the cumulative weight percentages undersize as a function of the sieve aperture [15,18-20,24]. The cumulative weight percentage undersize for a specific sieve aperture is defined as the percentage of the particles by weight that can pass that sieve [15,18-20,24]. Cumulative particle size distribution is adequately described by the following distribution function [15]:
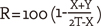
The variables X50 and b were determined by curve-fitting the data on equation (1) using the SigmaPlot 6.0 program [15,20]. X50 can be used as a measure of the average particle size [15,18-20,24]. Moreover, the masticatory efficiency index (R) was calculated by Edlund and Lamm's formula [17,19].
In order to use this method, the sum of the weight in grams of the chewed material accumulated on the sieve with aperture of 2.0 mm was referred to as the coarsest fraction (X). The sum of the weight in grams of the chewed material accumulated on the sieve with aperture of 1.0, 0.71, and 0.5 mm was combined and was referred to as the medium fraction (Y). T was the total weight in grams of the test portion after mastication [17,19]. In addition, the masticatory performance (P) was calculated as the percentage of food passing the sieve with aperture of 2.0 mm at 20 strokes by Manly and Braley's method [10,13,16].
All patients were asked to answer 7 questions concerning aspects of function, chewing comfort, aesthetics, and oral hygiene practices. In addition, the patients were asked to complete a visual analog scale (VAS). The questions were to be evaluated using a five grade categorized scale: 'total satisfaction' to 'total discontent' or, when comparing the implant with teeth, a three-grade categorizing scale: 'teeth', 'the same' or 'implant' was used.
In addition, the patients were asked to mark the respective VAS, a 100 mm straight line with the left end indicating 'total satisfaction' and the right end 'total discontent'. When comparing the implant with teeth, the left end indicated 'teeth', and the right end indicated 'implant'. The distance from the right end of the scale to the mark was measured in millimeters and the VAS was divided into 10 increments of 10 mm for analysis.
Statistical software (SPSS ver. 16.0, SPSS Inc., Chicago, IL, USA) was used for statistical analysis. For the comparison between masticatory performance for pre-insertion of the prosthesis (Pre-insertion) and post-insertion of the prosthesis (Post-insertion), the statistical significance was determined by a paired t-test (P<0.05).
Means of particle size distributions were obtained before and after insertion of prosthetic restoration (Table 3, Fig. 2). A characteristic pattern was observed in the cumulative-frequency curves, and it tended to show a sigmoid shape. The cumulative frequency curve for Post-insertion showed a shift towards smaller particle sizes.
The mean of X50 obtained from Pre-insertion was 0.96 mm, and 0.73 mm from Post-insertion. A considerable difference in the median particle size, X50 was observed between Pre- and Post-insertion with a paired t-test (P<0.0001). Moreover, the mean of R in Pre-insertion was 39.2, but in Post-insertion was 50.6. A significant difference in R was revealed after 20 chewing strokes (P<0.0001).
The mean of P was 67.8% in Pre-insertion and 84.3% in Post-insertion. There was a statistically significant difference between Pre- and Post- insertion (P<0.0001). The results of the masticatory performance parameters are summarized in Table 3.
All the distributed questionnaires were completed by the patients. To assess oral function, four of the questions asked about perception of function and subjective chewing comfort (Table 4). Patients were highly satisfied with chewing ability irrespective of the hardness of food. 45% of patients felt more secure when they chewed on their teeth than on the implants and 55% perceived no difference.
The fifth question dealt with cleansing of implant prosthesis. 70% of the patients were satisfied with their cleansing ability. The sixth question asked about a complication of cheek biting while masticating with the implant. 20% responded with "discomfort sometimes". The last question was about the treatment as an esthetic solution to a sunken cheek as perceived by the patient. 15% were satisfied from an esthetic point of view. A good correlation was found to exist between the results from the categorized questions and the VAS.
To restore the integrity and function of the dentition is the goal of dental care. Mastication is one of the main functions served by the dentition, especially by the posterior teeth. Therefore, masticatory functions are considered to be a critical outcome measurement for dental treatment and are used to evaluate prosthodontic treatment outcomes [11,16,25-27,30,31]. However, we noted that there has been a lack of studies reporting on masticatory performance with objective parameters (e.g., R, P, X50) in second molar single implant therapy. This study assessed masticatory performance before and after insertion of an implant prosthesis. In addition, patient satisfaction after second molar single tooth implant therapy was evaluated with questionnaires and VAS.
Masticatory performance is the most frequently used method of measuring masticatory function. It evaluates the size of food particles after a specified number of chewing cycles [10,13,15-20,24,28]. The test foods have varied and include artificial foods such as Optosil (Condensing Silicon; Heraeus Kulzer, Sao Paulo, Brazil) and a very wide range of natural foods [13]. The types of foods used have led to variations in the results, because of their inherent properties and solubility [13]. Although there is some controversy about what food substance is best for masticatory performance tests, peanuts have been the most common choice, as they are relatively uniform in their size, which facilitates standardization and can be used without any additional manipulation [16,32]. Compared to artificial food, peanuts are advantageous in that they are commonly consumed and people are accustomed to chewing them. Therefore, it seemed to be acceptable when compared with other materials like raw carrots or raisins [16,17].
Kapur et al. [28] have suggested that for a valid performance test, the specified number of chewing strokes for a food must be less than the number of masticatory strokes required by a subject in the preparation of the same food for swallowing. Edlund and Lamm [17] reported that the mean number of masticatory strokes necessary to achieve optimal pulverization of test material was 20.4. In this kind of test, 20 strokes is the number most commonly used [16,17,23,24,30,31]. We used 20 strokes in this study.
The only function of mastication is to prepare food for swallowing [23]. Yurkstas [23] reported that the swallowing threshold was directly related to masticatory performance. Thus, people with a superior masticatory function attained a finer degree of food pulverization at the swallowing threshold than did people who possessed dentition that was less efficient [23]. Regardless of the method used, finer particles corresponded to more efficient mastication.
In our study, masticatory performance (P) significantly increased in all patients (Table 2, Fig. 1). P after insertion of the implant prosthesis increased from 67.83±9.92 to 84.33±8.45%. With the implant prosthesis, the P value increased by 24%. This is in agreement with data presented by Manly and Braley [16]. They reported that for a person having the first and second molar in occlusion, the average P was 78%.
The masticatory efficiency index (R) after insertion of the implant prosthesis was higher than that before insertion of the implant prosthesis. With the implant prosthesis, the R value increased by 29%. In addition, X50 after insertion of the implant prosthesis was lower than that before insertion of the implant prosthesis. These parameters indicate that particle size distribution after insertion of a second molar single implant prosthesis is finer than that before insertion of an implant prosthesis. When a missing second molar is restored by using an implant, the number of postcanine functional tooth units and the total food platform area are increased [10,11]. According to Yurkstas [10], the second molar provided 28% of the total food platform area. The more occlusal units are restored, the better the masticatory performance obtained [11]. In this study, a statistically significant difference was shown between objective parameters before and after insertion of the implant prosthesis (P<0.0001). These results may be due to the lack of an adaptation period after removal of the implant prosthesis. Yurkstas et al. [27] found that persons supplied with fixed bridges and a removable prosthesis showed an improvement in masticatory performance after 2 weeks [13]. Abel and Manly [26], in a study on patients with partial dentures, describe a learning period with improvement in masticatory performance after insertion of the dentures. Maximum chewing efficiency was attained at about 1 month [26]. Therefore the tested implants were restored with the prosthesis more than 1 month before the study.
The masticatory ability was evaluated with a 4-question survey. In addition, 3 questions assessed the oral hygiene practices, chewing discomfort due to cheek biting, and the esthetic aspect of a sunken cheek. Results of the responses to each question about chewing ability showed that 90% of the patients were completely satisfied with the implants regarding their ability to chew various kinds of food (raw carrots, soft bread, kimchi). Comparing the chewing function with teeth and implants, respectively, revealed 55% of patients preferring neither the former nor the latter for their masticatory function. 45% of patients felt more secure when they chewed with the teeth. Pjetursson et al. [29] reported that 78% of the patients either perceived no difference in masticating with teeth or implants, or preferred implants. Some patients in this study had a shorter loading period (1 month) than patients in the study of Pjetursson et al. [29]. This may partly explain the difference between these results.
In the present study, 70% of the patients stated that they could clean the implant restoration very well. Pjetursson et al. [29] reported that 94% of the patients were satisfied with their own oral hygiene practice. These differences may have been caused by the relative accessibility for cleaning according to the location of implant installation.
Assessing the chewing discomfort due to cheek biting, 20% of patients sometimes felt a chewing discomfort due to cheek biting. Although several studies have reported that lip, tongue, and cheek biting were significantly often observed in the patients who received a fixed implant supported prosthesis in an edentulous jaw [33,34], only cheek biting was observed in the patients who received second molar single implant therapy. Assessing the esthetic improvement of a sunken cheek, 15% of patients were satisfied after insertion of the implant. When Pjetursson et al. [29] assessed the esthetic appearance of the anterior implant restoration, they revealed that more than 97% of patients were satisfied. Therefore it is estimated that patients' perception of the esthetic improvement after insertion of a posterior implant may be lower than that of anterior implant insertion.
Masticatory function is derived from a complex interplay of direct and indirect effects. However, our study focused on only one variable - with and without the implant prosthesis. When the chewing test performed without the prosthesis, patients had already adapted to having the prosthesis. Hence, the differences between objective masticatory function before and after insertion of the prosthesis would be overestimated. Because of the limitation of a retrospective study, this study does not include an adaptation period for removal of the implant prosthesis. The number of subjects was too small to compare the difference between the locations of implants - maxilla vs. mandible.
Therefore, prospective studies with larger numbers of subjects are needed in the future. Multiple variables should be included in further studies to accurately assess the effect of second molar single implant therapy on masticatory function. In spite of such limitations, in accordance with previous reports, the data in the present study showed that a second molar single implant can increase masticatory function.
Figures and Tables
Figure 2
Cumulative weight percentage undersize Qw (percentage) as a function of the logarithm of the sieve aperture X (mm) after 20 chewing strokes. Pre-insertion: before insertion of prosthesis, Post-insertion: after insertion of prosthesis.
ACKNOWLEDGEMENTS
The authors thank Dr. Kyung-Nyun Kim and Dr. Lee-Ra Cho for their valuable discussions and organization of this study. Help with statistical analysis was provided by Dr. Deuk-Sang Ma. No financial or material support was provided by any company to the authors or the patients involved in this study.
References
1. Jung UW, Choi JY, Kim CS, Cho KS, Chai JK, Kim CK, et al. Evaluation of mandibular posterior single implants with two different surfaces: a 5-year comparative study. J Periodontol. 2008. 79:1857–1863.

2. Mayer TM, Hawley CE, Gunsolley JC, Feldman S. The single-tooth implant: a viable alternative for single-tooth replacement. J Periodontol. 2002. 73:687–693.

3. Lee HB, Paik JW, Kim CS, Choi SH, Lee KW, Cho KS. The comparison between the success rates of single implants replacing the mandibular first and second molar. J Korean Acad Periodontol. 2004. 34:101–112.

4. Becker W, Becker BE. Replacement of maxillary and mandibular molars with single endosseous implant restorations: a retrospective study. J Prosthet Dent. 1995. 74:51–55.

5. Levin L, Laviv A, Schwartz-Arad D. Long-term success of implants replacing a single molar. J Periodontol. 2006. 77:1528–1532.

6. Jung SW, Lee JK, Um HS, Chang BS. A retrospective study on survival rate of the most posterior single tooth implant. J Korean Acad Periodontol. 2008. 38:611–620.

7. Muftu A, Chapman RJ. Replacing posterior teeth with freestanding implants: four-year prosthodontic results of a prospective study. J Am Dent Assoc. 1998. 129:1097–1102.

8. Schwartz-Arad D, Samet N, Samet N. Single tooth replacement of missing molars: a retrospective study of 78 implants. J Periodontol. 1999. 70:449–454.

9. Shugars DA, Bader JD, Phillips SW Jr, White BA, Brantley CF. The consequences of not replacing a missing posterior tooth. J Am Dent Assoc. 2000. 131:1317–1323.

10. Yurkstas AA. The effect of missing teeth on masticatory performance and efficiency. J Prosthet Dent. 1954. 4:120–123.

11. van der Bilt A, Olthoff LW, Bosman F, Oosterhaven SP. Chewing performance before and after rehabilitation of post-canine teeth in man. J Dent Res. 1994. 73:1677–1683.

12. Boretti G, Bickel M, Geering AH. A review of masticatory ability and efficiency. J Prosthet Dent. 1995. 74:400–403.

13. Bates JF, Stafford GD, Harrison A. Masticatory function - a review of the literature. III. Masticatory performance and efficiency. J Oral Rehabil. 1976. 3:57–67.
14. Lucas PW, Luke DA. Methods for analysing the breakdown of food in human mastication. Arch Oral Biol. 1983. 28:813–819.

15. Olthoff LW, van der Bilt A, Bosman F, Kleizen HH. Distribution of particle sizes in food comminuted by human mastication. Arch Oral Biol. 1984. 29:899–903.

18. van der Bilt A, Olthoff LW, Bosman F, Oosterhaven SP. The effect of missing postcanine teeth on chewing performance in man. Arch Oral Biol. 1993. 38:423–429.

19. Cho LL, Kim KN, Chang IT, Heo SJ. A Study on the effects of chewing patterns to occlusal contact points and chewing efficiency. J Korean Acad Craniomandib Disord. 1994. 6:125–135.
20. Sierpinska T, Golebiewska M, Lapuc M. The effect of mastication on occlusal parameters in healthy volunteers. Adv Med Sci. 2008. 53:316–320.

21. Gambareli FR, Serra MD, Pereira LJ, Gaviâo MB. Influence of measurement technique, test food, teeth and muscle force interactions in masticatory performance. J Texture Stud. 2007. 38:2–20.

22. Katsuhiko K, Takahiro O, Garrett NR, Minoru T. Assessment of masticatory performance: methodologies and their application. Prosthodont Res Pract. 2004. 3:33–45.
23. Yurkstas AA. The masticatory act: a review. J Prosthet Dent. 1965. 15:248–260.
24. Buschang PH. Masticatory ability and performance: the effects of multilated and maloccluded dentitions. Semin Orthod. 2006. 12:92–101.

25. Vinton P, Manly RS. Masticatory efficiency during the period of adjustment to dentures. J Prosthet Dent. 1955. 5:477–480.

26. Abel LF, Manly RS. Masticatory function of partial denture patients among navy personnel. J Prosthet Dent. 1953. 3:382–392.

27. Yurkstas A, Fridley HH, Manly RS. A functional evaluation of fixed and removable bridgework. J Prosthet Dent. 1951. 1:570–577.

28. Kapur K, Soman S, Yurkstas A. Test foods for measuring masticatory performance of denture wearers. J Prosthet Dent. 1964. 14:483–491.

29. Pjetursson BE, Karoussis I, Bürgin W, Brägger U, Lang NP. Patients' satisfaction following implant therapy. A 10-year prospective cohort study. Clin Oral Implants Res. 2005. 16:185–193.

30. Pera P, Bassi F, Schierano G, Appendino P, Preti G. Implant anchored complete mandibular denture: evaluation of masticatory efficiency, oral function and degree of satisfaction. J Oral Rehabil. 1998. 25:462–467.

31. Woodmansey KF, Ayik M, Buschang PH, White CA, He J. Differences in masticatory function in patients with endodontically treated teeth and single-implant-supported prostheses: a pilot study. J Endod. 2009. 35:10–14.

32. Kim SK, Kin ME, Kim KS. Intra- and inter-examiner reliability on the estimation of masticatory efficincy: by pulverizing peanuts with a sieve-system. J Korean Acad Oral Med. 2002. 27:381–389.
33. Engfors I, Ortorp A, Jemt T. Fixed implant-supported prostheses in elderly patients: a 5-year retrospective study of 133 edentulous patients older than 79 years. Clin Implant Dent Relat Res. 2004. 6:190–198.

34. Jemt T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Brånemark implants in edentulous jaws: a study of treatment from the time of prosthesis placement to the first annual checkup. Int J Oral Maxillofac Implants. 1991. 6:270–276.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download