Abstract
Purpose
To analyze the dimensions of the embrasure space between the maxillary central incisors as potential factors influencing interdental papilla fill and height.
Methods
The embrasure dimensions between the maxillary central incisors of 100 subjects (40 females/60 males) were assessed with clinical, study model, and radiographic examinations. Variables of the complete and deficient papilla fill groups were compared. Multiple regression analyses were performed to investigate potential influence of the distance between the contact point and bone crest (CP_BC), horizontal interdental distance (HID), and facio-lingual thickness (FLT) at the papilla base on complete/deficient papilla fill and papilla height (PH).
Results
CP_BC was the only variable that showed a significant difference between the complete and deficient papilla groups (P<0.05). When the CP_BC was less than 5 mm, the embrasure spaces between the maxillary central incisors were completely filled with interdental papilla. Multiple regression analyses revealed that a significant predictor for complete/deficient papilla fill was CP_BC, and significant predictors for PH were CP_BC and HID (P<0.05).
Conclusions
The chances of complete papilla fill increased as CP_BC decreased, while PH increased as CP_BC and HID increased. However, the FLT of the papilla base did not appear to affect papilla fill or PH. From an esthetic perspective, CP_BC as well as HID should be considered as factors influencing the topography of interdental papilla.
Interdental papillae not only protect underlying periodontal tissues, but also play an important role from an esthetic point of view. Incomplete papilla filling of the embrasure space between the teeth often compromises esthetic appearance, especially in the visible maxillary anterior region.
Various dimensions of the embrasure space occupied with interdental papillae were evaluated as potential factors influencing papilla fill (PF) along with other factors such as periodontal disease, tooth shape, and aging [1-7]. The distance between the contact point and bone crest (CP_BC), i.e., the height of the embrasure space, was found to be a strong factor influencing PF, while the effects of the horizontal interdental distance (HID), i.e., the mesio-distal width of the embrasure space on the interdental PF, were contradictory [1-7]. With respect to the facio-lingual depth of the embrasure space, a 3-dimensional analysis of the interproximal area including the facio-lingual dimension has been suggested as a means for evaluating the gingival response to interdental dimensional changes [2]. In addition, the FLT of a papilla base has been suggested as a potential factor influencing PF adjacent implant-supported restorations [8]. However, to date, the facio-lingual dimension of the embrasure space has not been investigated in relation to PF.
Papilla height (PH), i.e., the distance between the tip of the interdental papilla and the bone crest, determines the degree of PF with reference to CP_BC. The PH of a complete papilla fill group has been found to be greater than that of a deficient papilla fill group [5,7]. Among the embrasure dimensions, CP_BC was positively correlated with PH [7], and HID positively influenced PH as well [9]. However, information about the effects of FLT on PF is lacking in the literature. Based on the finding that an increased thickness of gingiva during orthodontic tooth movement resulted in coronal migration of the gingival margin [9], one can assume that the increased FLT may positively influence PH.
The aim of this study was to analyze dimensions of the embrasure space between maxillary central incisors as potential factors influencing interdental papilla fill and height.
One hundred subjects (40 females/60 males) were recruited from among the students at the Chonbuk National University School of Dentistry, Jeonju, Korea. To be eligible for the study, the subjects could not have any proximal restorations or crowns, orthodontic treatment, or gingival inflammation at the maxillary central incisors. They also were not allowed to have taken any medications with known effects on the gingiva. The mean age of the subjects was 28.7 years (range, 24 to 36 years). All subjects provided informed consent, and approval for the study was obtained from the Institutional Review Board of Chonbuk National University Hospital, Jeonju, Korea (CBIRB 0908-84). The study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2000.
At the clinical examination, degree of papilla fill was determined at the proximal areas between the maxillary central incisors using the scoring system of the Papilla Index [10]. Papilla with index scores of 1 and 2 were classified as "deficient papilla," and those with scores of 3 and 4 were classified as "complete papilla."
In study models fabricated at the clinical examination, FLT of the papilla base was measured with the use of a gauge (Iwanson Spring Caliper, Hu-Friedy Chicago, Chicago, IL, USA) as the distance between the facial and lingual mid-point of a line connecting the most apical margins of the two maxillary central incisors (Fig. 1).
Digital radiographs (Heliodent vario, Sirona Dental Systems GmbH, Bensheim, Germany) were taken with the digital X-ray sensor parallel and the X-ray beam perpendicular to the proximal area between the maxillary central incisors. The tip of the interdental papilla between the maxillary central incisors was defined with a radio-opaque endodontic canal sealer (Sealapex, Kerr Co., Orange, CA, USA). PH, i.e., the distance from the tip of the papilla to the bone crest level, HID, i.e., the horizontal distance between the maxillary central incisors at the level of bone crest, and the distance between the CP_BC, i.e., the vertical distance from the apical border of the contact area between the maxillary central incisors to the bone crest, were measured on the digitized images (Fig. 1). A 5×5 mm metal strip placed on the facial surface of a maxillary central incisor was used for calibration of the radiographic assessments. All linear measurements were performed with a software program (NIH Image, The National Institutes of Health, Bethesda, MD, USA).
A single examiner (S.A.K) who was trained and calibrated during the pilot study performed all assessments. Measurement errors of the clinical, study model, and radiographic assessments were estimated by repeated assessments of 20 randomly selected cases with an interval of two weeks. The papilla index score was the same in 18 of 20 cases (90%). The mean difference between the repeated assessments was 0.04 mm (SD, 0.10) for HID, 0.15 mm (SD, 0.23) for CP_BC, 0.15 mm (SD, 0.20) for FLT of the papilla base, and 0.01 mm (SD, 0.12) for PH.
The subject was used as a statistical unit for the analysis of the data. The median and 25th and 75th percentiles were calculated for data description since the data were non-normally distributed. The primary outcome variable of the data analysis was "complete/deficient papilla." The differences between the complete papilla and deficient papilla groups were compared with the use of the Mann-Whitney U test for continuous variables and the chi-square test for gender. A multiple logistic regression analysis was performed to investigate potential influences of the three embrasure dimensions on the binary outcome variable "complete/deficient papilla."
The secondary outcome variable of the data analysis was "PH." A multiple regression analysis was performed to investigate potential influences of the three embrasure dimensions on PH.
Statistical analyses were performed with a statistical software program SPSS ver.16 (SPSS Inc., Chicago, IL, USA). A P-value<0.05 was regarded as statistically significant.
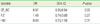
On the photographic assessments, 66 subjects were judged as having a complete papilla between the maxillary central incisors, while 32 subjects had a deficient papilla. Two subjects with an open proximal contact were excluded from the judging. Neither age nor gender was significantly different between the complete papilla and deficient papilla groups. The embrasure dimensions and PH at the maxillary central incisors were compared between the complete papilla and deficient papilla groups, as shown in Table 1. CP_BC was the only variable that showed a statistically significant difference between the complete and deficient papilla groups (P< 0.05).
A 3D scatter plot including three dimensions of the embrasure space (CP_BC, HID, and FLT) illustrated that a complete papilla was more frequently observed with a small CP_BC (Fig. 2).
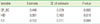
Multiple logistic regression analysis including the three embrasure dimensions as explanatory variables revealed that CP_BC was the only predictor significantly influencing the dependent variable "complete/deficient papilla" (Table 2).
The present study evaluated for the first time the FLT of the papilla base as a potential factor influencing interdental PF or PH in addition to HID and CP_BC, which have been extensively evaluated in previous studies [1-7]. The results revealed that FLT of the papilla base failed to show a significant influence on PF or PH; however, CP_BC as well as HID were found to be significant factors influencing PF or PH.
The FLT of the papilla base was thicker in the complete papilla group than in the deficient papilla group (mean 8.6 mm vs. 8.4 mm), but the difference was not statistically significant (Table 1). A recent study reported that the facial gingiva thickness was significantly greater at the interproximal area with a complete papilla fill than with a deficient papilla fill [7]. The authors of that previous study measured the interproximal gingival thickness at the facial aspect, while we measured the FLT of the papilla base as the distance between the facial and lingual mid-point of a line connecting the most apical margins of the two maxillary central incisors in the study model. Consequently, the FLT of the papilla base was highly correlated with the facio-lingual dimension of the maxillary central incisor crowns (r=0.76, P<0.01). The FLT assessment level set at the line connecting the most apical margins of the two maxillary central incisors is similar to the proximal bone crest considering the highly scalloped cement-enamel junctions of the maxillary central incisors (i.e., the proximal bone crest level is higher than the facial/lingual bone level) [11]. However, in future studies, dental cone beam computed tomography could be used for a more accurate and reliable assessment of various embrasure dimensions than can be achieved with conventional radiography or the study model assessments used in the present study.
In the multiple logistic regression analysis, CP_BC was a significant factor for "complete/deficient papilla," but FLT and HID were not found to be significant factors (Table 2). The finding for CP_BC is in agreement with previous studies [1-7]. The effects of HID on the interdental PF in the literature are contradictory. An association between HID and PF has been found in some studies [3-6], but not in others [7]. Furthermore, HID was a statistically significant factor for PF on univariate analysis, but it was not a significant factor on multivariate analysis after controlling for age and CP_BC [5-6]. In fact, the effect of an increase in HID on PF became more prominent with increased CP_BC [3], and an increase in CP_BC corresponded to a marked increase in the distance between the contact point and papilla tip when the HID was less than 2.4 mm [4]. Hence, it would be beneficial to include all relevant factors in a multivariate model to better understand the role of each factor in the outcome [12].
In terms of clinical application, square-shaped crowns with broad and flat proximal surfaces as well as contact points positioned as apical as possible favored by restorative dentists would increase the probability of a complete papilla fill, and consequently achieve more predictable soft tissue aesthetics [13]. On the other hand, crestal bone resorption caused by periodontal disease would decrease the chances of complete papilla filling due to the increased CP_BC.
The mean PH from the bone crest was 4.4 mm (SD, 0.9) for the complete papilla group and 4.2 mm (SD, 0.8) for the deficient papilla group, but the difference was not statistically significant (Table 1). While PH has previously been found to be significantly greater in the papilla presence group than in the papilla recession group [5], the difference can be attributed to the different ages of the subject samples between the two studies. The age of subjects in the referenced study ranged from 18 to 73 years, while the subjects in the present study were young dental students (mean, 28.7 years; range, 24 to 36 years). Aging was one of the factors influencing papilla recession [5], and PH decreased by 0.012 mm/year in subjects aged from 18 to 73 years [7]. In fact, the mean age of subjects in the present study did not differ between the complete and deficient papilla groups, and the mean difference in PH between the complete and deficient papilla groups (4.4 mm vs. 4.2 mm) was small in comparison to that of the other study (5.2 mm vs. 3.7 mm) [5].
It has been claimed that increased thickness of the gingiva results in coronal migration of the gingival margin [14]. In a similar way, one can expect that PH would be increased when the thickness of the papilla base increases. However, FLT of the papilla base failed to show a significant influence on PH, while, HID was found to be a significant factor for PH in the multiple regression model (Table 3). This corroborates a previous finding that HID was a significant factor influencing PH, although FLT was not included as an explanatory variable in the regression models [9]. The author interpreted the finding based on the same hypothesis we had about the effect of FLT on PH, i.e., "a greater width at the papilla base could support greater PH."
The majority of the embrasure spaces of the current study were completely filled with interdental papilla (66 of 98 subjects), and all subjects with a deficient papilla were assigned a papilla index score of 2, i.e., greater than half of the height of the interdental papilla was present [11]. Furthermore, as mentioned above, the effect of aging on PH, which can cause papilla recession, was minimal in the current study. Hence, it appeared that PH increased when CP_BC increased in the multiple regression analysis (Table 3). The finding is also in line with other studies which observed a positive correlation between PH and CP_BC [7,15].
The present study focused on the analysis of embrasure dimensions between only the maxillary central incisors. Additionally, the study subjects were young dental students with good periodontal health and of similar age, and this less inclusive sample may have increased the statistical precision. On the other hand, our results have limited application to the general population as well as for different tooth positions. Only linear measurements of the embrasure dimensions were performed in the present study, though embrasure area [2,6] and volume [16] assessed with advanced techniques should be considered as potential factors affecting PF and PH in future studies.
Within the limitations of this study, it can be concluded that the chances of complete PF increased as CP_BC decreased, while papilla height increased as CP_BC and HID increased. However, FLT of the papilla base did not appear to affect PF or PH. Hence, from an esthetic perspective, CP_BC as well as HID should be considered factors influencing the topography of interdental papilla.
Figures and Tables
Figure 1
Radiographic and study model assessments of various embrasure dimensions between the maxillary central incisors. HID: horizontal interdental distance, BC: bone crest, PH: papilla height, PT: papilla tip, CP: contact point, CP_BC: distance between the contact point and bone crest, FLT: facio-lingual thickness of the papilla base.

Figure 2
Relationships between complete/deficient papilla and the three embrasure dimensions. CP_BC: distance between the contact point and bone crest, HID: horizontal interdental distance, FLT: facio-lingual thickness at the papilla.
Figure 3
Relationships between papilla height (PH) and 3 embrasure dimensions. (A) Distance between the contact point and bone crest (CP_BC), (B) Horizontal interdental distance (HID), (C) Facio-lingual thickness at the papilla base (FLT). Dotted lines indicate 95% confidence interval for the regression line.

Table 1
Embrasure dimensions and papilla height between the maxillary central incisors in relation to complete papilla and deficient papilla.

References
1. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992. 63:995–996.

2. Kurth JR, Kokich VG. Open gingival embrasures after orthodontic treatment in adults: prevalence and etiology. Am J Orthod Dentofacial Orthop. 2001. 120:116–123.

3. Cho HS, Jang HS, Kim DK, Park JC, Kim HJ, Choi SH, et al. The effects of interproximal distance between roots on the existence of interdental papillae according to the distance from the contact point to the alveolar crest. J Periodontol. 2006. 77:1651–1657.

4. Martegani P, Silvestri M, Mascarello F, Scipioni T, Ghezzi C, Rota C, et al. Morphometric study of the interproximal unit in the esthetic region to correlate anatomic variables affecting the aspect of soft tissue embrasure space. J Periodontol. 2007. 78:2260–2265.

5. Chang LC. Assessment of parameters affecting the presence of the central papilla using a non-invasive radiographic method. J Periodontol. 2008. 79:603–609.

6. Chen MC, Liao YF, Chan CP, Ku YC, Pan WL, Tu YK. Factors influencing the presence of interproximal dental papillae between maxillary anterior teeth. J Periodontol. 2010. 81:318–324.

7. Chow YC, Eber RM, Tsao YP, Shotwell JL, Wang HL. Factors associated with the appearance of gingival papillae. J Clin Periodontol. 2010. 37:719–727.

8. Gastaldo JF, Cury PR, Sendyk WR. Effect of the vertical and horizontal distances between adjacent implants and between a tooth and an implant on the incidence of interproximal papilla. J Periodontol. 2004. 75:1242–1246.

9. Chang LC. Factors Associated With the Interdental Papilla Height Between Two Maxillary Central Incisors: A Radiographic Study. J Periodontol. 2011. 05. 04. [Epub]. DOI:10.1902/jop.2011.100574.

10. Jemt T. Regeneration of gingival papillae after single-implant treatment. Int J Periodontics Restorative Dent. 1997. 17:326–333.
11. Ash MM. Ash MM, editor. The Permanent Maxillary Incisors. Wheeler's dental anatomy, physiology and occlusion. 1993. Philadelphia: W.B. Saunders;128–149.
12. Teughels W, Merheb J, Quirynen M. Critical horizontal dimensions of interproximal and buccal bone around implants for optimal aesthetic outcomes: a systematic review. Clin Oral Implants Res. 2009. 20:Suppl 4. 134–145.

13. Phillips K, Kois JC. Aesthetic peri-implant site development. The restorative connection. Dent Clin North Am. 1998. 42:57–70.
14. Wennström JL. Mucogingival considerations in orthodontic treatment. Semin Orthod. 1996. 2:46–54.

15. Chang LC. Effect of bone crest to contact point distance on central papilla height using embrasure morphologies. Quintessence Int. 2009. 40:507–513.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download