Abstract
Purpose
To investigate the healing pattern of the mucous membrane after tooth extraction necessitated by periodontal disease in the maxillary sinus.
Methods
One hundred and three patients with 119 maxillary sinuses were investigated. Before implant placement, cone-beam computed tomography (CT) scanning was performed. The causes of extraction, the time elapsed since extraction, smoking, periodontal disease in adjacent teeth, and gender were recorded. In addition, the thickness of the mucous membrane of the maxillary sinus and the height of residual alveolar bone at the extracted area were calculated from CT images.
Results
The thickness of the mucous membrane in the periodontal disease group (3.05±2.71 mm) was greater than that of the pulp disease group (1.92±1.78 mm) and the tooth fracture group (1.35±0.55 mm; P<0.05). The causes of extraction, the time elapsed since extraction, and gender had relationships with a thickening of the mucous membrane of the maxillary sinus (P<0.05). In contrast, the height of the residual alveolar bone at the extracted area, periodontal disease in adjacent teeth, and smoking did not show any relation to the thickening of the mucous membrane of the maxillary sinus.
The loss of alveolar bone caused by periodontal disease and pneumatization of the maxillary sinus make it difficult to install implants in the maxillary posterior area. Recently, techniques for maxillary sinus augmentation, the lateral window technique and the alveolar osteotome technique, have been widely used in the clinic and have made surgery highly predictable [1,2]. However, several complications including perforation, bleeding, and inflammation of the mucous membrane may occur during the surgical procedure [3-5]. To minimize these kinds of complications, surgical techniques and materials have been developed and we should clearly determine the relation between the nature of the mucous membrane and oral diseases that may influence to abnormalities of mucous membrane.
Bergh et al. [6] noted that mucosal thickening is not an absolute contra-indication but may constitute a relative contraindication for sinus floor elevation. Worth and Stoneman [7] demonstrated that the acute or chronic infection causes hypertrophy of the maxillary mucosal membrane, a decrease in the volume of the maxillary sinus, and leads to the inflammation of the maxillary sinus due to a decline in the natural drainage of the maxillary sinus.
It has been reported that the average thickness of the normal mucous membrane of maxillary sinus is 0.8 mm, but acute or chronic inflammation can cause thickening of the sinus membrane [7]. Rak et al. [8] reported that abnormalities in the ethmoidal sinuses were occurred only if 3 mm or more of mucous thickening was present. One to 2-mm of mucous thickening in the ethmoidal sinuses occur in 63% of asymptomatic patients.
One of the causes of inflammation in the maxillary sinus is odontogenic infection, the incidence of which is 10-12% [9,10]. If the involved part of the maxillary sinus is close to the root of a premolar or molar, periodontal and endodontic infection can easily affect the sinus membrane. Even if the maxillary sinus is some distance from the root, severe periodontal disease may cause infection around the root that elicits a thickening of the mucous membrane. Vallo et al. [10] reported that periodontitis is related with the severity of the mucous membrane thickening and increases in the prevalence rate.
Many studies have been conducted on the relationship between periodontal disease and mucosal thickening in the sinus membrane [11-13]. However, these reports were usually made at a time when teeth were still present, and there have been no studies conducted on the changes in the mucous membrane after extraction. The purpose of the present study is to investigate the healing pattern of the mucous membrane after tooth extraction necessitated by periodontal disease in the maxillary sinus.
This study involved patients who had computed tomography (CT) scanning prior to the treatment of implants in maxillary posterior teeth at Wonkwang University Dental Hospital from September 1, 2007, to March 10, 2010. A total of 103 patients with 119 maxillary sinuses were investigated. Of the maxillary sinuses, 65 were the right side and 54 were the left. There were 61 males and 42 females and the average age of patients was 51.50 years.
The following factors, which are suspected of having an influence on mucous thickening, were evaluated for this study: the causes of extraction, the time elapsed since extraction, the height of residual alveolar bone at the extracted area, smoking, periodontal disease in adjacent teeth, and gender. All factors were investigated by analyzing dental records and radiographs. The causes of extraction were divided into three groups: the 'periodontal disease' group were those patients with teeth extracted due to periodontal disease, the 'pulp disease' group were those that had teeth extracted because of caries or endodontic problems, and the 'tooth fracture' group consisted of patients who had teeth extracted because of a fracture of a retained root or crown. Regarding the time elapsed since extraction, 4 months was chosen as the standard cutoff because Huang et al. [14] reported that 4 months was required to recover a normal mucous membrane after surgery for maxillary sinusitis. Patients with less than 4 months elapsed since extraction were classified into Group A, from 4 to less than 12 months were classified into Group B, and those with more than 12 months were classified into Group C. Regarding the height of residual alveolar bone, those with less than 4 mm were classified into Group I, from 4 mm to less than 10 mm were classified into Group II, and those with more than 10 mm were classified into Group III. Periodontal disease in adjacent teeth was diagnosed when pocket depth was more than 3 mm, when there was bleeding on probing, and when alveolar bone loss was visible by radiograph. Patients with periodontal disease in adjacent teeth were classified into the 'disease' group, and patients with no periodontal disease in adjacent teeth were classified into the 'normal' group. Twenty-five cases with insufficient data for diagnosing periodontal disease were excluded from this evaluation. All patients having periodontal disease received scaling and root planing or periodontal flap surgery according to the severity of their disease. Before implant placement, cone-beam CT (Alphard Vega, Asahi Roentgen, Kyoto, Japan) scanning was performed, using the D-mode (scan size 51×51 mm, voxel size 0.1 mm) and I-mode (scan size 102×102 mm, voxel size 0.2 mm) CT formats. The thickness of the mucous membrane was measured at the thickest area using a ruler in PiView STAR software (Infinitt Co., Seoul, Korea). Based on studies by Patel et al. [15] and Rak et al. [8], a mucous membrane thickness under 2 mm was regarded as 'normal,' more than 2 mm was regarded as a 'thickening' of the mucous membrane, and full radiopacity in the whole maxillary sinus was regarded as a 'completely radiopaque' membrane.
Data were statistically analyzed using SPSS 12.0 (SPSS Inc., Chicago, IL, USA). As the data did not have normal distribution, a non-parametric test, the Mann-Whitney U test, was used. A chi-square test was used for the assessment of mucous thickening (more than 2 mm) in relation to the above factors.
One hundred nineteen maxillary sinuses were studied and mucous thickening was observed in 55 (46%) sinuses. In the classification according to the causes of extraction, 82 belonged to the periodontal disease group, 22 belonged to the pulp disease group, and 14 belonged to the tooth fracture group. The average time elapsed after extraction for taking radiographs for the periodontal disease group was 13.6 months, for the pulp disease group was 14.5 months, and for the tooth fracture group was 9.8 months.
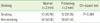
The thickness of the mucous membrane in the periodontal disease group (3.05±2.71 mm) was significantly higher than that of the pulp disease group (1.94±1.78 mm) and the tooth fracture group (1.31±0.52 mm, P<0.05) (Table 1). The prevalence of mucous thickening (more than 2 mm) was 53.85% for the periodontal disease group, which was significantly higher than that of the pulp disease group (27.27%) and the tooth fracture group (21.43%, P<0.05) (Table 2). The percentage of normal mucous membranes (less than 2 mm) was lower in the periodontal disease group than in the pulp disease group and the tooth fracture group. There were 4 cases of a completely radiopaque membrane in the periodontal disease group, but there were no completely radiopaque membranes in the pulp disease group or the tooth fracture group.
There was no significant difference between Group A (less than 4 months) and Group B (4 to 11 months) regarding the thickness of the mucous membrane according to the elapsed time after extraction, but there were significant differences between Group A and Group C, and between Group B and Group C (more than 12 months, P<0.05) (Table 3). In Group C, the average thickness of the mucous membrane (1.87±1.62 mm) was lower than 2 mm, which was considered to be the standard for mucous thickening. However, there were no significant differences regarding the prevalence of mucous thickening according to the time elapsed since extraction (Table 4).
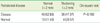
In Group I, where the height of residual alveolar bone at the extracted area was less than 4 mm, the thickness of the mucous membrane was 2.93±2.42 mm. In Group II, where the height of residual alveolar bone was over 4 mm but less than 10 mm, the thickness of the mucous membrane was 2.73±2.73 mm. In Group III, where the height of residual alveolar bone was more than 10 mm, the thickness of the mucous membrane was 2.13±1.70 mm. There were no significant differences between groups (Table 5). The difference in the prevalence of mucous thickening according to the different heights of residual alveolar bone at the extracted area was not significant among all groups (Table 6).
The thickness of the mucous membrane in smokers was 2.85±2.54 mm, while that of non-smokers was 2.55±2.44 mm (Table 7). There was no significant difference between the groups. Mucous thickening was more frequent in smokers (54.55%) than non-smokers (41.94%) (Table 8), but the difference was not significant. However, patients who had severe mucous thickening were almost all smokers. Five of the 7 patients who had mucous thickening of more than 10 mm were smokers (71%), and all patients who had a completely radiopaque membrane were smokers.
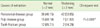
The mucous membrane of the maxillary sinus was thicker in the periodontal disease group (2.69±2.40 mm) than in the normal group (1.70±1.37 mm), but there was no significant difference between the groups (Table 9). Mucous thickening was more frequent in the disease group (47.37%) than in the normal group (28.57%), but the difference was not significant (Table 10).
This study assessed whether periodontitis, the most common infectious disease of the maxillary posterior teeth, affects the thickening of the mucous membrane in the maxillary sinus after tooth extraction. The group with periodontal disease as the cause of extraction showed a thicker mucous membrane than the pulp disease group and the tooth fracture group. These results also showed that a thickened mucous membrane needs more time than a normal mucous membrane after extraction.
In the present study, a diagnostic standard of 2 mm mucous membrane thickening by radiopacity was chosen. Rak et al. [8] reported that a thickness of less than 2 mm was a normal finding in the ethmoidal sinus. Patel et al. [15] reported that 2 mm was used as the cutoff because a thickness of less than 2 mm is difficult to measure on most magnetic resonance imaging scans. Based on these studies, we established 2 mm of mucous membrane as the threshold of mucous membrane thickening. We chose 4 months as the standard for the elapsed time after the extraction based on the observation by Huang et al. [14] that when treating patients with chronic maxillary sinusitis, most maxillary sinus mucosa recovered within 4 months.
There have been no studies conducted on the thickening of the mucous membrane in the maxillary sinus in relation to the cause of extraction, although several studies have reported on the relation between periodontal disease and abnormalities in maxillary sinus mucosa when teeth are still present. Tözüm et al. [16] reported that periodontitis may produce generalized sinus mucous membrane hyperplasia. Worth and Stoneman [7] reported that the thickness of a normal membrane of the maxillary sinus is under 0.8 mm, but periodontitis may lead to an increase in the size of the sinus membrane. These findings were supported by histopathological observations that severe periodontitis of the maxillary molars was clearly related to a thickening of the mucous membrane in the maxillary sinus [17]. Several studies using conventional radiography (periapical X-ray, panorama) reported that periodontitis was related with the severity and prevalence of mucous abnormality in maxillary sinus [10-13]. Bomeli et al. [18], who studied acute odontogenic inflammation of the maxillary sinus by CT, reported that oral maxillary sinus fistula and periodontitis were distinct causes of inflammation compared with that of caries or periapical abscess. As has been shown in previous studies, periodontitis has a close relation with the abnormality of maxillary sinus mucosa. In the present study, periodontitis is an important factor in the thickening of the mucous membrane even after extraction, this result was similar to previous studies evaluating the thickening of mucous membrane before extraction.
Inflammation will disappear if the cause of infection is removed. Therefore, the time elapsed since extraction can influence the thickening of the mucous membrane. In the present study, the average time elapsed since extraction was 13.6 months in the periodontal disease group, 14.5 months in the pulp disease group, and 9.8 months in the tooth fracture group. The thickness of the mucous membrane in the periodontal disease group was thicker than that of the pulp disease group considering the time elapsed since extraction. The tooth fracture group showed less thickening of the mucous membrane even though they had a shorter time elapsed since extraction than the other groups. In other words, a thicker mucous membrane remained where inflammation was present, and disappeared where no inflammation was present.
The thickness of the mucous membrane gradually decreased with increasing time since extraction (from Group A to Group C). The thickening of the mucous membrane in Groups A and B showed no significant difference. These results show that when thickening of the mucous membrane is maintained up to 11 months, it recovers to normal thickness after 12 months.
In the previous studies mentioned above, periodontal disease affected maxillary sinus mucosa. In the present study, the mucous membrane at the extracted area was thicker in the group with periodontal disease in adjacent teeth than in the group with no periodontal disease. However, it seems that periodontal disease in adjacent teeth had no influence on the thickening of the mucous membrane because there was no statistically significant difference between the two groups.
Several studies reported that mucous abnormality in the maxillary sinus was more frequent in males than females [19,20]. In contrast, Patel et al. [15] reported that there was no difference between the two genders. The present study found males to have thicker sinus mucosa than females.
No significant relationship was revealed between the height of residual bone around the extracted teeth and the thickening of the mucous membrane. This is similar to the findings of a study on the maxillary sinus using CT conducted by Cheong et al. [21]. We did not evaluate the relationship between age and the thickness of the mucous membrane because most of patients in the present study were elderly.
Smoking did not show a relationship with a thickening of the mucous membrane in the present study. This result is similar to studies of Tarp et al. [22], which investigated abnormalities of the maxillary sinus without otolaryngological disease, and Beaumont et al. [23], which studied maxillary sinus disease. However, 5 of 7 patients (71%) whose mucous thickness was more than 10 mm were smokers, and all patients with a completely radiopaque membrane were smokers. Therefore, we can reasonably conclude that severe thickening of the mucous membrane in the maxillary sinus was undoubtedly influenced by smoking.
The present study revealed that the causes of extraction, the time elapsed since extraction, and gender had significant relationships with the thickness of the mucous membrane in the maxillary sinus. After teeth were extracted, periodontal disease resulted in more severe thickening of the mucous membrane. In the future, a prospective study with a large population is needed to evaluate the relationship between changes in the thickness of the mucous membrane of the maxillary sinus and extraction. These findings reinforce the fact that careful history taking and radiographic evaluation prior to a sinus elevation technique are important for implant installation.
Figures and Tables
Table 1
Comparison of the thickness of the mucous membrane in the maxillary sinus according to the causes of extraction.

Table 3
Comparison of the thickness of the mucous membrane of the maxillary sinus according to the time elapsed since extraction.

Table 4
Prevalence of mucous thickening (more than 2 mm) according to the time elapsed since extraction.
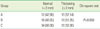
Table 5
Comparison of the thickness of the mucous membrane of the maxillary sinus according to the height of residual alveolar bone at the extracted area.
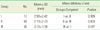
Table 6
Prevalence of mucous thickening (more than 2 mm) according to the height of residual alveolar bone at the extracted area.

Table 7
Comparison of the thickness of the mucous membrane of the maxillary sinus according to smoking.

Table 9
Comparison of the thickness of the mucous membrane of the maxillary sinus according to periodontal disease in adjacent teeth.

Table 10
Prevalence of mucous thickening (more than 2 mm) according to periodontal disease in adjacent teeth.
References
1. Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980. 38:613–616.
2. Hirsch JM, Ericsson I. Maxillary sinus augmentation using mandibular bone grafts and simultaneous installation of implants. A surgical technique. Clin Oral Implants Res. 1991. 2:91–96.

3. Schwartz-Arad D, Herzberg R, Dolev E. The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. J Periodontol. 2004. 75:511–516.

4. Maksoud MA. Complications after maxillary sinus augmentation: a case report. Implant Dent. 2001. 10:168–171.

5. Barone A, Santini S, Sbordone L, Crespi R, Covani U. A clinical study of the outcomes and complications associated with maxillary sinus augmentation. Int J Oral Maxillofac Implants. 2006. 21:81–85.
6. van den Bergh JP, ten Bruggenkate CM, Disch FJ, Tuinzing DB. Anatomical aspects of sinus floor elevations. Clin Oral Implants Res. 2000. 11:256–265.

7. Worth HM, Stoneman DW. Radiographic interpretation of antral mucosal changes due to localized dental infection. J Can Dent Assoc (Tor). 1972. 38:111–116.
8. Rak KM, Newell JD 2nd, Yakes WF, Damiano MA, Luethke JM. Paranasal sinuses on MR images of the brain: significance of mucosal thickening. AJR Am J Roentgenol. 1991. 156:381–384.

9. Abrahams JJ, Glassberg RM. Dental disease: a frequently unrecognized cause of maxillary sinus abnormalities? AJR Am J Roentgenol. 1996. 166:1219–1223.

10. Vallo J, Suominen-Taipale L, Huumonen S, Soikkonen K, Norblad A. Prevalence of mucosal abnormalities of the maxillary sinus and their relationship to dental disease in panoramic radiography: results from the Health 2000 Health Examination Survey. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010. 109:e80–e87.

11. Casamassimo PS, Lilly GE. Mucosal cysts of the maxillary sinus: a clinical and radiographic study. Oral Surg Oral Med Oral Pathol. 1980. 50:282–286.

12. Falk H, Ericson S, Hugoson A. The effects of periodontal treatment on mucous membrane thickening in the maxillary sinus. J Clin Periodontol. 1986. 13:217–222.

13. Engström H, Chamberlain D, Kiger R, Egelberg J. Radiographic evaluation of the effect of initial periodontal therapy on thickness of the maxillary sinus mucosa. J Periodontol. 1988. 59:604–608.

14. Huang HM, Lee HP, Liu CM, Lin KN. Normalization of maxillary sinus mucosa after functional endoscopic sinus surgery in pediatric chronic sinusitis. Int J Pediatr Otorhinolaryngol. 2005. 69:1219–1223.

15. Patel K, Chavda SV, Violaris N, Pahor AL. Incidental paranasal sinus inflammatory changes in a British population. J Laryngol Otol. 1996. 110:649–651.

16. Tözüm TF, Dursun E, Tulunoglu I. Sinus floor elevation from a maxillary molar tooth extraction socket in a patient with chronic inflammation. J Periodontol. 2009. 80:521–526.

17. Moskow BS. A histomorphologic study of the effects of periodontal inflammation on the maxillary sinus mucosa. J Periodontol. 1992. 63:674–681.

18. Bomeli SR, Branstetter BF 4th, Ferguson BJ. Frequency of a dental source for acute maxillary sinusitis. Laryngoscope. 2009. 119:580–584.

19. Havas TE, Motbey JA, Gullane PJ. Prevalence of incidental abnormalities on computed tomographic scans of the paranasal sinuses. Arch Otolaryngol Head Neck Surg. 1988. 114:856–859.

20. Nam EC, Lee BJ. Prevalence of sinus abnormality observed in the cranial computed tomograms taken to evaluate head injury patients. Korean J Otolaryngol-Head Neck Surg. 1998. 41:488–492.
21. Cheong CS, Cho BH, Hwang DS, Jung YH, Naa KS. Evaluation of maxillary sinus using cone-beam CT in patients scheduled for dental implant in maxillary posterior area. J Korean Assoc Oral Maxillofac Surg. 2009. 35:21–25.
22. Tarp B, Fiirgaard B, Christensen T, Jensen JJ, Black FT. The prevalence and significance of incidental paranasal sinus abnormalities on MRI. Rhinology. 2000. 38:33–38.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download