Abstract
Purpose
The purpose of this study was to evaluate the improvement of periodontal health of generalized aggressive periodontitis (GAgP) diagnosed patients treated with non-surgical periodontal therapy accompanying systemic antibiotics administration.
Methods
Two patients with GAgP were chosen for this study. Clinical indices were taken and a radiographic examination was performed at the baseline of the study and they were treated by periodontal therapy accompanying systemic antibiotics administration. Post-surgical visits were scheduled at regular intervals to check clinical and radiographic changes.
Results
Through non-surgical periodontal therapy accompanying systemic antibiotics administration, GAgP patients showed decreased probing pocket depth, sulcus bleeding index, and increased attachment level and clinical index when comparing the initial and six month follow up data. In the six month follow-up radiographic examination after non-surgical periodontal therapy, resolution of the bony defect was observed.
Generalized aggressive periodontitis (GAgP) is characterized as "generalized interproximal attachment loss affecting at least three permanent teeth other than the first molars and incisors" [1,2].
GAgP affects a minority of patients, but it is highly significant because it is characterized by severe destruction of the supporting apparatus of teeth in a relatively young subjects. Because of its less common occurrence, few studies have evaluated different treatment protocols for this condition. Among those, one study [3] recently applied the principles of full-mouth non-surgical periodontal treatment and found further improvement in clinical parameters when systemically administered antibiotics were added. It has been shown that successful treatment of GAgP is dependent on the reduction of specific pathogenic bacteria.
For example, the adjunctive use of metronidazole plus amoxicillin may control Aggregatibacter actionomycetemcomitans and Porphyromonas gingivalis more efficiently than single antibiotic regimens or mechanical therapy alone [4].
Its etiology is highly correlated to the presence of Aggregatibacter actionmycetencomitans [5-7] and host response defects [8-10] and is possibly related to a genetic inheritance [11-18].
There is no widely accepted treatment protocol for GAgP [19]. Treatment alternatives include scaling and root planing (SRP) alone or in conjunction with systemic antibiotics [20-22] as well as surgical [23] and interdisciplinary approaches [24,25], with adequate outcomes. However, there are only a few reports [19,23,26] of long-term follow-up for these different treatments.
Successful treatment of GAgP is considered to be dependent on early diagnosis, directing therapy towards elimination or suppression of the infecting microorganism and providing an environment conductive to long-term maintenance.
The purpose of this study was to evaluate the improvement of periodontal health of GAgP diagnosed patients treated with non-surgical periodontal therapy accompanying systemic antibiotics administration.
A 28-year-old male patient was referred by a general practitioner to the Institute for Periodontology and School of Dentistry, Kyungpook National University, for treatment of GAgP (Fig. 1). The initial examination revealed deep probing pocket depth (PD) with sulcus bleeding index (SBI). Suppuration was registered at the maxillary right first molar and the mandibular left first molar. Gingival inflammation was observed. The patient was in good general health, had never smoked, and did not take any medications. Familial aggregation of GAgP was denied. PD, tooth mobility (Mob), SBI, and the presence of suppuration were recorded (Fig. 2). A full mouth series of periapical radiographs was obtained (Fig. 3). Deep infrabony defects were evidence of progressing periodontal destruction. After full-mouth scaling, the patient received quadrant root planing four times at 1-weekly intervals over four consecutive sessions. Starting with SRP, systemic antibiotics (amoxicillin/clavulanate 375 mg and metronidazole 250 mg, both three times a day for 7 days) were prescribed. The patient was advised to abstain from mechanical oral hygiene in the treated areas for the first 3 postoperative weeks and to rinse with a 0.2% chlorhexidine solution twice daily. Routine supportive periodontal therapy was performed every 3 months. Whole-mouth clinical measurements were recorded with a manual periodontal probe at 6 month after the initiation of therapy. Measurements demonstrated distinct clinical improvements. PD of the affected sites had decreased to a maximum of 4 mm. Suppuration had been eliminated, and full-mouth SBI was as low as 10%. A negligible increase in recession was observed. Radiographs obtained 1 year after therapy showed fill of the bony defects and sharp contours of the gained hard tissues (Figs. 4, 5, 6).
A 12-year-old male patient was referred by a general practitioner to the Institute for Periodontology and School of Dentistry, Kyungpook National University, for treatment of GAgP (Fig. 7). The initial examination revealed deep PD with SBI. Gingival swelling was observed, especially in both anterior areas. The patient was in good general health and did not take any medications. Familial aggregation of GAgP was denied. PD, Mob, SBI and the presence of suppuration were recorded (Fig. 8). A panoramic radiograph was obtained (Fig. 9). Deep infrabony defects were evidence of progressing periodontal destruction. After full-mouth scaling, the patient received quadrant root planing four times at 1-weekly intervals over four consecutive sessions. Starting with SRP, systemic antibiotics (amoxicillin/clavulanate 375 mg and metronidazole 250 mg, both three times a day for 7 days) were prescribed. At supportive periodontal care six month after initial therapy, measurements demonstrated distinct clinical improvements. PD of the affected sites had decreased to a maximum of 7 mm. Full mouth SBI was as low as 5% (Figs. 10 and 11).
Several antibiotic regimens have been investigated as adjuncts to the mechanical therapy for GAgP. The combination of SRP with systemic administration of amoxicillin/clavulanate/metronidazole suppressed Aggregatibacter actinomycetemcomitans and other tested pathogens to below detectable levels. The concomitant effect on clinical parameters emphasizes the excellent efficacy of amoxicillin/clavulanate/metronidazole against periodontal infections in terms of microbiologic and clinical outcomes reported previously [20-22, 27].
Because persistently high bacterial counts and the presence of periodontal pathogens at surgery adversely affect clinical attachment level gains [28], meticulous initial therapy and good oral hygiene are considered to be prerequisites for successful periodontal surgery [29].
In case 1, postoperative healing was excellent, facilitated by the systemic administration of antibiotics, which has been reported previously. Six month after therapy, distinct clinical improvements were indicated. PD reduction ranged from 3 to 7 mm. Suppuration had been eliminated, and no gingival inflammation signs were observed. The periapical radiographs obtained 1 year after therapy showed fill of the bony defects and stability of the treatment outcome,. Although all sites demonstrated comparable clinical improvements, varying degrees of radiographic defect fill were observed (Figs. 4-6).
In case 2, substantial and stable clinical periodontal status were shown after conventional periodontal therapy and adjunctive administration of antibiotics. Six month after initial therapy, measurements indicated distinct clinical improvements with redection of PD and no suppuration. And full mouth SBI was decreased.
A high "repair potential" of previously untreated young GAgP patients is empirically assumed and has been a regular subject of discussion. However, the noticeably higher age, which was 28 years, of the patient presented here might limit the clinical application of these findings. Furthermore, after repeated attempts at periodontal therapy with concomitant "mechanical damage" to the root surfaces and subsequent bacterial recolonization and disease progression, the individual healing potential after the initial therapy alone could not be certain for the present patient. To improve the unclear prognosis, the depicted course of treatment included regenerative periodontal surgery, performed shortly after SRP and adjunctive antibiotics therapy.
The combination of initial therapy with adjunctive amoxicillin/clavulanate/metronidazole followed by non-surgical periodontal therapy provided a good clinical, radiographic, and esthetic result in the present patients with severe and progressing GAgP. Beyond the limits of these case reports, the significance of regenerative therapy in the evidence-based treatment of GAgP remains to be evaluated.
Figures and Tables
Figure 2
Baseline periodontal scores of case 1 patient. PD: probing pocket depth, SBI: sulcus bleeding index, Mob: tooth mobility.
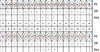
Figure 4
Clinical photographs of case 1 patient after 1 year therapy. Additional orthodontic appliance was attached for malocclusion.

Figure 5
Periodontal scores of case 1 patient after 1 year therapy. PD: probing pocket depth, SBI: sulcus bleeding index, Mob: tooth mobility.
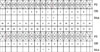
Figure 6
Radiographs of case 1 patient after 1 year therapy. Note that marked fill of the bony defects and sharp contours of the gained hard tissues.

Figure 8
Baseline periodontal scores of case 2 patient. PD: probing pocket depth, SBI: sulcus bleeding index, Mob: tooth mobility.

Figure 9
RInitial radiographs of case 2 pateint. Note the discrete vertical bone defects and missing teeth.

References
1. American Academy of Periodontology. Parameter on aggressive periodontitis. J Periodontol. 2000. 71:5 Suppl. 867–869.
3. Guerrero A, Griffiths GS, Nibali L, Suvan J, Moles DR, Laurell L, et al. Adjunctive benefits of systemic amoxicillin and metronidazole in non-surgical treatment of generalized aggressive periodontitis: a randomized placebo-controlled clinical trial. J Clin Periodontol. 2005. 32:1096–1107.

4. Pavicic MJ, van Winkelhoff AJ, Douque NH, Steures RW, de Graaff J. Microbiological and clinical effects of metronidazole and amoxicillin in Actinobacillus actinomycetemcomitans-associated periodontitis. A 2-year evaluation. J Clin Periodontol. 1994. 21:107–112.

5. Fine DH, Markowitz K, Furgang D, Fairlie K, Ferrandiz J, Nasri C, et al. Aggregatibacter actinomycetemcomitans and its relationship to initiation of localized aggressive periodontitis: longitudinal cohort study of initially healthy adolescents. J Clin Microbiol. 2007. 45:3859–3869.

6. Haraszthy VI, Hariharan G, Tinoco EM, Cortelli JR, Lally ET, Davis E, et al. Evidence for the role of highly leukotoxic Actinobacillus actinomycetemcomitans in the pathogenesis of localized juvenile and other forms of early-onset periodontitis. J Periodontol. 2000. 71:912–922.

7. DiRienzo JM, Slots J, Sixou M, Sol MA, Harmon R, McKay TL. Specific genetic variants of Actinobacillus actinomycetemcomitans correlate with disease and health in a regional population of families with localized juvenile periodontitis. Infect Immun. 1994. 62:3058–3065.

8. Page RC, Sims TJ, Geissler F, Altman LC, Baab DA. Abnormal leukocyte motility in patients with early-onset periodontitis. J Periodontal Res. 1984. 19:591–594.

9. Lavine WS, Maderazo EG, Stolman J, Ward PA, Cogen RB, Greenblatt I, et al. Impaired neutrophil chemotaxis in patients with juvenile and rapidly progressing periodontitis. J Periodontal Res. 1979. 14:10–19.

10. Page RC, Sims TJ, Geissler F, Altman LC, Baab DA. Defective neutrophil and monocyte motility in patients with early onset periodontitis. Infect Immun. 1985. 47:169–175.

11. Hart TC, Kornman KS. Genetic factors in the pathogenesis of periodontitis. Periodontol 2000. 1997. 14:202–215.

12. Kinane DF, Shiba H, Hart TC. The genetic basis of periodontitis. Periodontol 2000. 2005. 39:91–117.

13. Boughman JA, Astemborski JA, Suzuki JB. Phenotypic assessment of early onset periodontitis in sibships. J Clin Periodontol. 1992. 19:233–239.

14. Beaty TH, Boughman JA, Yang P, Astemborski JA, Suzuki JB. Genetic analysis of juvenile periodontitis in families ascertained through an affected proband. Am J Hum Genet. 1987. 40:443–452.
15. Saxen L, Nevanlinna HR. Autosomal recessive inheritance of juvenile periodontitis: test of a hypothesis. Clin Genet. 1984. 25:332–335.

16. Hart TC, Marazita ML, Schenkein HA, Diehl SR. Re-interpretation of the evidence for X-linked dominant inheritance of juvenile periodontitis. J Periodontol. 1992. 63:169–173.

17. Melnick M, Shields ED, Bixler D. Periodontosis: a phenotypic and genetic analysis. Oral Surg Oral Med Oral Pathol. 1976. 42:32–41.

18. Page RC, Vandesteen GE, Ebersole JL, Williams BL, Dixon IL, Altman LC. Clinical and laboratory studies of a family with a high prevalence of juvenile periodontitis. J Periodontol. 1985. 56:602–610.

19. Buchmann R, Nunn ME, Van Dyke TE, Lange DE. Aggressive periodontitis: 5-year follow-up of treatment. J Periodontol. 2002. 73:675–683.

20. Berglundh T, Krok L, Liljenberg B, Westfelt E, Serino G, Lindhe J. The use of metronidazole and amoxicillin in the treatment of advanced periodontal disease. A prospective, controlled clinical trial. J Clin Periodontol. 1998. 25:354–362.

21. Winkel EG, van Winkelhoff AJ, van der Velden U. Additional clinical and microbiological effects of amoxicillin and metronidazole after initial periodontal therapy. J Clin Periodontol. 1998. 25:857–864.

22. Sigusch B, Beier M, Klinger G, Pfister W, Glockmann E. A 2-step non-surgical procedure and systemic antibiotics in the treatment of rapidly progressive periodontitis. J Periodontol. 2001. 72:275–283.

23. Renvert S, Nilveus R, Dahlen G, Slots J, Egelberg J. 5-year follow up of periodontal intraosseous defects treated by root planing or flap surgery. J Clin Periodontol. 1990. 17:356–363.

24. Worch KP, Listgarten MA, Korostoff JM. A multidisciplinary approach to the diagnosis and treatment of early-onset periodontitis: a case report. J Periodontol. 2001. 72:96–106.

25. Passanezi E, Janson M, Janson G, Sant'Anna AP, de Freitas MR, Henriques JF. Interdisciplinary treatment of localized juvenile periodontitis: a new perspective to an old problem. Am J Orthod Dentofacial Orthop. 2007. 131:268–276.

26. Kamma JJ, Baehni PC. Five-year maintenance follow-up of early-onset periodontitis patients. J Clin Periodontol. 2003. 30:562–572.

27. van Winkelhoff AJ, Tijhof CJ, de Graaff J. Microbiological and clinical results of metronidazole plus amoxicillin therapy in Actinobacillus actinomycetemcomitans-associated periodontitis. J Periodontol. 1992. 63:52–57.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download