Abstract
This is a retrospective review of two adult siblings with osteogenesis imperfecta (OI) type III (according to Sillence classification), who sustained a spontaneous femoral neck fracture and subsequent nonunion. The diagnosis of OI in these two patients was made based on clinical, radiological and genetic findings. The fracture was most likely caused by femoroacetabular impingement secondary to OI induced acetabular protrusio. A valgus osteotomy according to Pauwels'principles and fixation of the osteotomy and nonunion with a locking plate resulted in healing despite compromised bone quality and limited bone stock. Long-term follow up (4.5 years and 6.5 years, respectively) is provided.
When treating this difficult problem, improving the mechanobiological environment and decreasing the femoroacetabular impingement by a Pauwels type osteotomy should be considered.
Osteogenesis imperfecta (OI), also named “brittle bone disease” is a hereditary disorder that affects the quality and quantity of collagen I12). The manifestations of this disease in the musculoskeletal system vary12). The OI hip often has a varus deformity as well as “pincer” type impingement because of the acetabular protrusio345). With the resulting excessive forces on the femoral neck by the impingement, a “stress” fracture of the femoral neck can develop. Often these femoral neck fractures in OI are non-displaced. The combination of inherent poor bone quality, vertical shear forces because of coxa vara, compromises bone healing. In addition, there is limited room for standard internal fixation devices.
We speculate on an improved healing potential of these challenging fractures and nonunions when the improved mechanobiological load principles of the hip according to Pauwels' are incorporated in the surgery tactic and planning6). Using a customized locking plate adequate internal fixation is possible despite limited bone stock. The patients were informed that these cases would be submitted for publication.
A 55-year-old female (height, 120 cm) with OI type III (Sillence classification) was referred to us 9 months after failed treatment of a spontaneous right femoral neck fracture (Fig. 1A). Diagnosis was based on clinical history, radiological and genetic findings. Clinical diagnosis included short stature, multiple fractures due to minimal or no trauma, delayed healing and nonunion of fractures and progressive deformities. Radiological key findings included deformities of the long bones with multiple fractures, coxa vara, protrusio acetabuli and very thin, deformed and osteopenic bones. Genetic testing showed mutation COL1A1 c.2461G>A p.(Gly821Ser) (heterozygous).
Initial treatment had consisted of two cancellous screws. In addition a small bone biopsy was done at the request of her treating internist (with consent of the patient). Postoperative radiographs noted an iatrogenic fracture at the site of the bone biopsy (Fig. 1B). Initially this was treated non-operatively with bedrest. However, pain was difficult to control and there were no early signs of healing. At 2.5 months she could not tolerate bedrest any longer. She was taken back to the operating room and plate fixation with cerclage wires was done (Fig. 1C). She was followed regularly for 9 months. She then requested a referral to our department where she had been treated many years prior for a left femoral shaft nonunion.
When we saw her she was taking 70 mg morphine orally, with continuous pain in her hip and hardly the ability to stand for transfer. Prior to her femoral neck fracture she was able to perform a short transfer from wheelchair to bed. Since the age of 7 years she was wheelchair bound. The last years taking morphine for progressive and severe pain and neurologic spasms related to spinal cord injury due to many vertebral compression fractures and severe scoliosis. Plain radiographs and a computed tomography (CT) showed a femoral neck nonunion as well as a subtrochanteric nonunion at the previous biopsy site, with additional deformities of pelvis and distal femur. There was very close contact between the posterior wall and the femoral neck nonunion site (Fig. 1D). We planned a Pauwels type osteotomy to address both the femoral neck nonunion as the ipsilateral subtrochanteric iatrogenic nonunion. In addition we planned a distal femoral osteotomy to obtain better alignment of the lower aspect of the femur. She was placed supine on a radiolucent table. A lateral approach was done. All hardware was removed. We did not do a formal debridement of both nonunion sites. We first addressed the varus deformity of the distal femur. A lateral closing wedge osteotomy was done using an oscillating saw under cooling. A pelvic reconstruction plate was used with standard screws. The distal screws were drilled eccentrically to provide compression across the osteotomy site.
Next we addressed the proximal femur with the femoral neck and subtrochanteric nonunion. We anticipated a Pauwels osteotomy of 40°. At the subtrochanteric nonunion site a closing wedge was removed from the lateral cortex. Using K-wires as joy-sticks the osteotomy was aligned. The best available fit for this deformed femur was a titanium Philos plate (DePuy Synthes, Amersfoort, the Netherlands). The plate was customized to fit on the proximal femur. Screws were placed after drilling in the femoral neck using an oscillating to prevent a fausse route. A fibular allograft was wedged in between plate and bone to increase bone stock and stability. The plate was then secured to the shaft (Fig. 2A–D). Post-operatively there were no complications. At 5 months a CT showed healing of the femoral neck nonunion. She was so pleased with the increased range of motion of her right hip that the Pauwels osteotomy had given her that she requested a similar procedure on the left side, which was done 9 months after the right side. This osteotomy also healed with good results for the patient (Fig. 3). Seven months after the left Pauwels osteotomy (and 16 months after the right osteotomy) she sustained a left distal femur fracture for which she was treated with a medial sided Philos plate and allograft bone chips.
At 2.5 years after the last surgery on her right hip a CT was taken because of increasing right hip pain when standing. The CT showed fully healed osteotomies and consolidation of the femoral neck nonunion. The most posterior screw in the right femoral neck was partly out of the neck (before re-entry into the femoral head) and was impinging on the ischium because of increasing protrusion of the femoral head into the acetabulum. This screw was removed in addition to removal of part of the greater trochanter to limit impingement. At four and a halve year she had new onset pain in her left groin during sitting. A CT showed a fresh fracture of the left ramus inferior os pubis. The nonunion of her right femoral neck was noticed to be solidly headed (Fig. 4A). There was full incorporation of the allograft and healing of the subtrochanteric iatrogenic/pathologic fracture (Fig. 4B).
A 43-year-old male (brother of case 1; height, 135 cm) with an OI type III phenotype (Sillence classification) was treated for a femoral neck fracture 5 months prior (Fig. 5A). The genetic testing showed mutation COL1A1 c.2461G>A p.(Gly821Ser) (heterozygous). The CT of the fracture suggested a stress-type fracture with abutment of the posterior wall of the acetabulum against the femoral neck. There was bowing of the femoral shaft, varus deformity of the proximal femur with protrusio acetabuli and subsequent femoroacetabular impingement. Initial treatment was a Pauwels valgus subtrochanteric osteotomy of 30° and fixation of the femoral neck with a locking screw in a long spanning 4.5 LCP titanium pelvic reconstruction plate (DePuy Synthes). The osteotomy improved alignment with subsequently a better biomechanical environment for the femoral neck fracture to heal. Although a second more distal femoral shaft osteotomy had been considered to better align the remainder of the shaft, it was felt too risky at that time. Five months later there was no healing of the femoral neck fracture. The Pauwels osteotomy had healed (Fig. 5B). There was ongoing hip pain and he could not ambulate as well as before. As there was no good alternative it was felt that further valgization might provide a more beneficial loading of the nonunion according to Pauwels' philosophy. Under general anesthesia with the patient supine on a radiolucent table we removed the previous hardware. Next, a 40° closing osteotomy at the subtrochanteric level was done. Distal to the osteotomy there was a sagittal deformity (apex anterior). To correct this, a 10° anterolateral closing wedge was done at the apex of the deformity. We now had 4 components: the proximal femoral neck and head, the rest of the femoral neck to the subtrochanteric osteotomy, the proximal femoral shaft and the distal femoral shaft. Despite numerous attempts it was not feasible to use one device to fix all 4 components. We used 2 separate plates to fix the 4 components. We were able to place two screws in the femoral neck for improved fixation and stability. He recovered without complications. At 2 months after surgery plain radiographs and a CT showed healing of the femoral neck and of both osteotomies (Fig. 5C–D). At latest follow up 6.5 years after the last hip surgery he had no or limited pain and was able to walk approximately 10 meters without assistive devices or help. At work as a systems administrator he uses a walker.
OI is a rare inherited connective tissue disease causing bone fragility most often by a type-I collagen mutation. More recently, other mutations in genes that are involved in processing, folding and stability of collagen, as well as in differentiation or function of osteoblasts have been described12). Patients with OI suffer many fractures especially in childhood2). The severity of disease is reflected in the Sillence classification, designated in at least 21 classified subtypes of OI1). Mild forms have occasional fractures, whereas the more severe forms have many fractures, up to 200 in childhood. OI Type II is lethal at birth or shortly after birth. OI type III are most severely affected often suffering multiple fractures that most commonly occur after minor trauma, no trauma or stress fractures, severe bone deformities, kyphoscoliosis and a short stature. Most fractures are in the long bones of the lower extremity2).
We treated two adult siblings with type III OI for a femoral neck nonunion using Pauwels' principles for a presumed mechanobiological problem6). Based on CT evaluation, femoroacetabular impingement because of severe protrusio acetabuli was identified as at least one of the causes of the nonunion. Furthermore, patients with OI Type III, usually have deformities in more than one plane (sagittal, coronal and rotational). In our two patients, there were deformities in both coronal and sagittal planes, but there was no rotational deformity. The sagittal deformities of the femoral diaphysis were addressed in both cases by an additional corrective osteotomy along the femoral diaphysis.
Only few authors have discussed femoral neck fractures in OI. In 2013 a review (spanning the period 1980–2012) by Chow et al.7) found 7 papers on this specific topic. Chow's own series of 5 patients added to a total of 20 reported femoral neck fractures in OI. Papanna et al.8) reported on 7 pediatric patients (11 hips) with OI treated with a cannulated headless screw. All of them had been on bisphosphonates. Difficulties that were noted in these reports were of diagnosis, pre-existing implants, structural abnormalities and distortion and bone fragility and hardware failure. No mention was made of femoroacetabular impingement as a related factor in the development of the fracture and subsequent nonunion. When reviewing our cases we identified a paper by Beck et al.9) who were the first to report this mechanism in 3 otherwise healthy patients. They noted the femoral neck abutting the posterior acetabular rim that acted as a fulcrum with repetitive strain and motion across the fracture. The impingement in their 3 cases was due to a bump on the posterior femoral neck. If a nonunion develops, treatments options are even more challenging. It is unclear in our 2 patients what the role of improved joint clearance (less femoroacetabular impingement) vs. the redirection of the plane of the fracture by valgization (Pauwels' philosophy) was. Surgical alternatives are few for these problems. A customized hip replacement is fraught with other problems such as high costs, infection, loosening and limited bone stock10). A girdlestone would have been an alternative but both patients were both quite mobile and not willing to give up their hip. Many years later, both are very pleased with the outcome while having retained their native hip. It is unclear which patients well benefit from a Pauwels osteotomy in addition to femoral neck fixation. Also, the expectations from the patient are very important. If the patient is mostly sitting (wheelchair bound) then excessive forces will be produced at the femoral neck nonunion. If the patient is standing then coxa vara produces excessive stresses at this junction. The osteotomy should be planned to allow for hip range of motion that minimizes excessive stress with these anticipated activities during daily living. If the patient is mostly sitting, then the focus should be on corrective osteotomy that improves range of motion for sitting.
Increased understanding of the underlying disease mechanism and improved therapies will hopefully improve bone quality in OI. Use of bisphosphonates in OI has become common practice but clear guidelines and evidence are still lacking. Until then we need to optimize our reduction and fixation methods for these challenging fractures and nonunions. Pre-operative CT should be scrutinized for femoroacetabular impingement. Due to the extreme protrusio acetabuli in our patients this was probably a factor in the development of the fractures itself and the subsequent nonunion. Although trimming of the acetabular rim or the femoral neck may be considered in other patients, and may be a treatment for a typical pincher type femoro-acetabular impingement, however, we feel that these procedures should not be recommended in cases of OI because there is a high risk of fracture during these procedures.
Figures and Tables
Fig. 1
(A–C) Anteroposterior radiographs. (A) The right sided femoral neck fracture. A femoral nail is still in situ from previous fixation. (B) Subtrochanteric fracture at 2.5 months after initial surgery. (C) The revision fixation. (D) Axial computed tomography of the hip showing impingement of the acetabulum on the femoral neck.

Fig. 2
Sequential fluoroscopic images showing the Pauwels osteotomy, (A, B); fixation and interposition of fibular allograft (C, D).

Fig. 3
Anteroposterior pelvic radiograph at 2.5 years postoperatively shows the healed nonunion and osteotomies of the right femur as well as the healed reconstruction of the left proximal femur.

Fig. 4
Coronal computed tomographic images at 4.5 years after the Pauwels osteotomy. (A) The healed femoral neck. (B) The healed proximal femur.
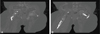
Fig. 5
(A–C) Anteroposterior radiographs. (A) Femoral neck fracture with severe acetabular protrusion and coxa vara. (B) Initial fixation with a long plate and one locking screw in the neck. (C) After osteotomies and revision fixation. (D) Axial computed tomographic image confirms healing of the femoral neck nonunion at 2 months after the last surgery.

ACKNOWLEDGEMENTS
The authors thank to Dr. Alessandra Maugeri, Laboratory for Clinical Genetics, VU University Medical Center, Amsterdam, the Netherlands.
References
1. Van Dijk FS, Sillence DO. Osteogenesis imperfecta: clinical diagnosis, nomenclature and severity assessment. Am J Med Genet A. 2014; 164A:1470–1481.

2. Gil JA, DeFroda SF, Sindhu K, Cruz AI Jr, Daniels AH. Challenges of fracture management for adults with osteogenesis imperfecta. Orthopedics. 2017; 40:e17–e22.

3. Violas P, Fassier F, Hamdy R, Duhaime M, Glorieux FH. Acetabular protrusion in osteogenesis imperfecta. J Pediatr Orthop. 2002; 22:622–625.

4. Aarabi M, Rauch F, Hamdy RC, Fassier F. High prevalence of coxa vara in patients with severe osteogenesis imperfecta. J Pediatr Orthop. 2006; 26:24–28.

5. Trehan SK, Morakis E, Raggio CL, Twomey KD, Green DW. Acetabular protrusio and proximal femur fractures in patients with osteogenesis imperfecta. J Pediatr Orthop. 2015; 35:645–649.

6. Pauwels F. [Basics of indication and technique of rearrangement in femoral neck pseudarthrosis]. Arch Klin Chir. 1949; 262:404–422. German.
7. Chow W, Negandhi R, Kuong E, To M. Management pitfalls of fractured neck of femur in osteogenesis imperfecta. J Child Orthop. 2013; 7:195–203.

8. Papanna MC, Tafazal S, Bell MJ, Giles SN, Fernandes JA. Femoral neck fractures in osteogenesis imperfecta treated with bisphosphonates. J Child Orthop. 2017; 11:191–194.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download