Abstract
Purpose
This study characterizes the short-term outcomes of ceramic coated metal-on-metal (MoM) large head total hip arthroplasty (THA) in prospectively selected patients aged 70 to 75 years.
Materials and Methods
Eighteen patients (18 hips) between the ages of 70 and 75-years old with THA using ceramic-coated MoM large heads between June 2014 and December 2014 were evaluated. We prospectively selected patients younger than 70 years for bipolar hemiarthroplasty and older than 75 years for conventional THA. There were one case of osteoarthritis, 8 cases of femur neck fracture, and 9 cases of intertrochanteric fracture. All patients underwent clinical and radiological follow-up at 6 weeks, 6 and 12 months, and every year postoperatively. The mean duration of follow-up was 24.2 months (range, 18–34 months).
Results
The average Harris hip score at the final follow-up was 81.0, except one case which was ultimately converted to conventional THA due to acetabular cup loosening. Radiographically, mean acetabular cup inclination was 45.8°(range, 38–56°) and anteversion was 20.1° (range, 11–25°). The average femoral head size was 48.7 mm. All stems were neutral-positioned except 1 varus-positioned stem. There was 1 case of a soft tissue infection, 3 patients complained of persistent groin pain, and no dislocations occurred.
Conclusion
Ceramic coated large MOM articulation (ACCIS) have many complications: cup loosening, groin pain, which can lead to fatal outcomes in the elderly patients. Especially in patients with communicated intertrochanter fracture (AO 31-A22, 23), careful attention should be paid to the choice of surgical option.
Total hip replacement arthroplasty (THA) is recognized as an effective treatment for degenerative diseases and hip fractures in the elderly. The application range of THA is gradually increasing with the extension of patient's lifespan and lifestyle changes. However, complications of THA in elderly patients can lead to fatal outcomes. One well-known complication is dislocation (reported incidence of 0.4% to 5.8%)12).
Large femoral heads have been used in THA to reduce the risk of dislocation and are associated with increased jumping distance and range of motion (ROM). Metal-on-metal bearings of these large heads provide theoretical advantages of large articulations that improve joint stability and have a low friction rate and increased wear-resistance345). However, some concerns about metal-on-metal articulation have arisen: i) autoimmune and soft tissue diseases6), ii) DNA break7), and iii) hypersensitivity8).
Metal-on-metal surfaces coated with ceramic providing reduced wear and friction rates are theoretically attractive prostheses in terms of large head with a reduction in released ions. We used ceramic-coated large metal heads and ceramicsurfaced cups in THA.
To our knowledge, this study is the first article focused on ceramic-coated metal-on-metal large head THA. The purpose of this study is to present the safety and efficacy outcomes of ceramic coated metal-on-metal large head THA in prospectively selected patients aged 70 to 75 years.
This study was approved by the institutional review board of The Catholic University of Korea, Daejeon St. Mary's Hospital (DC17RESI0082).
Between June 2014 and December 2014, THA in patients with modified Koval index stage of greater than 3 (under 70-years old) and bipolar hemiarthroplasty (patients over 75-years old) were performed910). During that period, 18 patients (18 hips) aged between 70 and 75 years were enrolled to be operated on with ceramic-coated metal-on-metal large heads910).
There were 8 men and 9 women (mean age of 72.0 years; range, 70–75 years) at the time of surgery. There was one case of osteoarthritis, 8 cases of femur neck fracture, and 9 cases of intertrochanteric fracture.
Basic clinical details included age, gender, etiology, pre & postoperative modified Koval indeces, complications and bone mineral density were collected. Patient activity was recorded with the modified Harris Hip Score (mHHS)11).
The THA implant consisted of acetabular and femoral head components made of Cobalt-Chromium-Molybdenum alloy. A ceramic titanium-niobium-nitride coating is applied on the articular surfaces of both components. Cementless acetabular components of the advanced ceramic coated implant system (ACCIS; Implantcast GmbH, Buxtehude, Germany) have three radii with three distinct areas: i) polar area with no contact between the bone and the component, ii) fit area in contact with the porous coated surface for bone ingrowth, and iii) press fit area with circumferential press fit at the equator (Fig. 1). Femoral components have three parts: i) 12/14 mm cone, ii) cone adapter, and iii) modular head (Fig. 2). The ACCIS guide recommends that if hard bone (e.g., subchondral sclerosis) is encountered, preventing proper seating of the component, an acetabulum reamer larger than 1 mm is needed. Each adapter is available in three different neck lengths in 4 mm increments and suited for three head sizes12).
All patients underwent clinical and radiological follow-up at 6 weeks, 6 and 12 months, and every year postoperatively. The mean duration of follow-up was 24.2 months (range, 18–34 months).
Standard anteroposterior pelvic X-rays were used to measure acetabular cup version and inclination. Acetabular inclination was defined as an angle between the line connecting both tear drop and acetabular cup measured on anteroposterior radiographs. Acetabular anteversion was measured on anteroposterior radiograph using Widmer's method13). Femoral stem positioning was measured on anteroposterior radiographs (varus and valgus less than 5° was considered as a neutral position).
The modified Gibson approach was used and after routine approach, the short external rotators were exposed. The insertion of the quadratus femoris was identified and used the quadratus femoris osteotomy approach14). After implanting the prosthesis, the decision to use a cemented or noncemented stem was determined based on bone quality. The bone fragment detached by flap osteotomy was reattached with wires. In cases of proximal femur fractures, Greater Trochanteric Reattachment Devices (DePuy Synthes, Westchester, PA, USA) or wires were used for greater trochanter fixation.
In the immediate postoperative period, the hip is positioned in abduction with a triangular pillow to maintain abduction, and deep breathing exercises, pneumatic pumps and isometrics exercise of lower extremity are begun. On the first postoperative day, if not limited by discomfort, patients can sit up. Gait practicing usually can begin after removal of drain in the physical training (PT) center. Practicing gait without help in older patients has additional risks, (e.g., fall from height), so most gait trains started in the PT room. Most elderly patients required a gait-assistance device to maintain balance. To prevent venous thromboembolic disease, active exercises and intermittent pneumatic compression boots of both lower extremities were applied immediately after surgery. The peak incidence of deep vein thrombosis varies among studies, with a range of 4 to 17 days after surgery. We used low-molecular-weight heparin daily for two weeks postoperatively151617).
The statistical analyses were performed using IBM SPSS Statistics ver. 19.0 (IBM Co., Armonk, NY, USA).
Among the 18 patients included in this study, there was 1 case of osteoarthritis, 8 cases of femur neck fracture, and 9 cases of intertrochanteric fracture. No patients presented with anatomical hip deformity (Table 1).
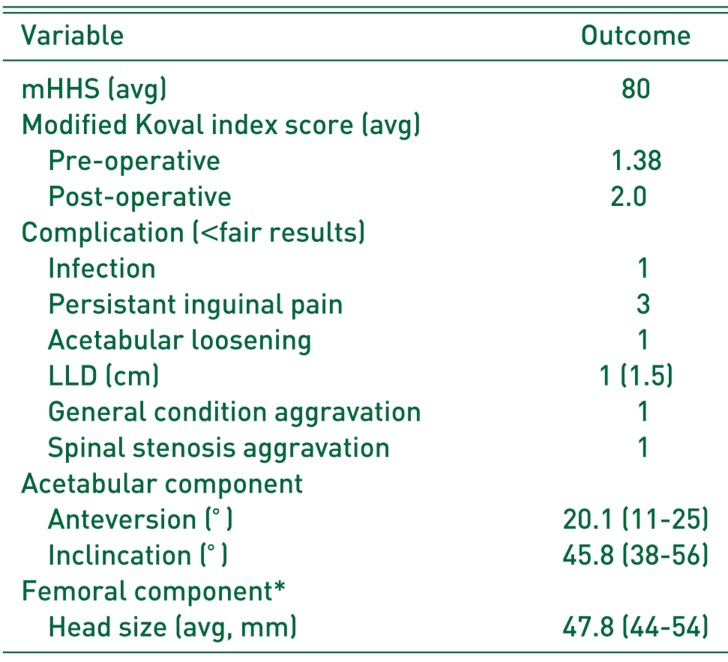
The modified Koval index scores decreased slightly from average pre-operative 1.38 (range, 1–3) to 2 (range, 1–5) at the final follow-up after surgery. For pre-operative and postoperative modified-Koval score evaluation, Wilcoxon signed rank test was performed. The P-value 0.009 (P<0.05) on the test showed that the postoperative Koval score was significantly improved. Ambulatory function was unchanged after THA in 10 cases and deteriorated in 8 cases. In case of deterioration, the patients showed a 1- or 2-stage decline. The average mHHS at the final follow-up was 81.0. The mHHS distribution was bimodal and the difference appears to depend on the degree of fracture. In the mHHS, the pretrauma ROM was not directly measurable, and the scores were measured according to the bus and stair availability. The reason for this was that the flexion in the HHS had the greatest effect on the score. The mHHS above 80 points except a femur neck fracture were intertrochanter fractures of Müller AO Classification 31-A21 (Simple). The mHHS below 80 points were Müller AO Classification 31-A22 or 23 (Comminuted) in the intertrochanter fracture. Three patients complained of persistent hip pain and their femur head size were 46 mm (n=1) and 50 mm (n=2). They did not experience a reduction in pain without treatment; pain relievers were used as necessary, along with rest and non-steroidal anti-inflammatory drugs. One patient experienced a soft tissue infection which required subsequent cement bead and debridement, and was cured within postoperative 2 months (Table 2). In case of osteoarthritis (male, n=56), acetabular-component loosening occurred by un-pressure fitted acetabular cup without screws. As recommended by the ACCIS guide, if subchondral sclerosis due to arthritis occurred, a reamer one size larger than expected acetabular cup size should be used. In this case after revision operation with screw fixation, good results were achieved. Importantly, no dislocations occurred. At the final follow-up, there were no cases of clinical hypersensitivity or allergic reactions.
Radiography indicated a mean acetabular cup inclination of 45.8° (range, 38–56°) and mean anteversion of 20.1° (range, 11–25°). The average femoral head size was 48.7 mm. All stems were positioned neutrally except 1 (varus). Four cases of progressive acetabular osteoporotic changes throughout the follow-up period occurred; however, these radiographic signs were not associated with patients complaints. The mHHS were an average 85 points (range, 84–95). Limb length discrepancy more than 1.5 cm was observed in one case of intertrochanteric fracture and no dislocations occurred (Table 2).
This study helps show that even with ceramic-coated metal-on-metal heads, the results of THA are not always positive, and when choosing between THA or bipolar hemiarthroplasty, the patient's systemic condition, disease characteristic and fracture degree should be carefully considered. Importantly, however, the use of large head femoral components provides a clear advantage of reduced dislocation rate181920).
Indications for the use of large femoral heads (i.e., larger than 36 mm) are increasing in THA. Importantly, implants with large articulation decrease the risk of dislocation21), particularly in elderly patients with weak neuromuscular muscle control, weakness and hip fractures. This decrease in risk of dislocation appears to be the result of the large head size (i.e., large head:neck ratio and increased jump distance of larger articulation leading to an increased range of motion without impingement)22).
Crowninshield et al.23) demonstrated in 2004 that a larger femoral head size can provide the more hip stability by increasing the prosthetic impingement-free range and the inferior head displacement required for hip dislocation. If femoral head size is increased from 22 mm to 40 mm, the required displacement for dislocation is increased by roughly 5 mm with the acetabular inclination at 45°. But increasing acetabular component abduction above 45° considerably decreases this conferred benefit to hip stability by larger femoral heads. The use of large femoral heads has demonstrated the greatest benefit when applied with appropriate acetabular inclination.
Rodriguez and Rathod24) reported in 2012 that there are advantages of THA with large femoral heads (e.g., hip stability and reduced dislocation rates). However, acetabular component alignment is a critical factor in THA stability. Clinical studies have not demonstrated any benefit of large heads (38 mm or 40 mm) and using a large head in THA is associated with a higher incidence of groin pain. Even in our study, the number of subjects was small, but there were no dislocations with an average head size of 49 mm.
However, there are potential risks associated with the use of large heads. There are concerns related to the release of metal ions due to corrosion of the head-neck junction leading to adverse local tissue reactions25). Dyrkacz et al.26) demonstrated higher corrosion scores in patients with a 36-mm bearing compared with a 28-mm bearing. Elkins et al.20) reported that a femoral head larger than 40 mm provides a minimal benefit for joint safety; however, trunnion corrosion seems to increase significantly. Importantly, corrosion of the head-neck junction is a multifactorial problem and cannot be explained as the single factor resulting from the use of a larger head26).
Another problem associated with larger diameter femoral heads is the possibility of groin pain, which is considered to be associated with soft-tissue impingement2728). One recent study demonstrated that larger-diameter heads were associated with a higher rate (18% vs. 7%) of groin pain compared with regular size implants. In the case reports of Browne et al.28), using a larger diameter than the native femoral head was stated to cause anterior iliopsoas and capsular impingement. In this study, 3 patients complained of persistent inguinal pain which was relieved using conservative care.
The advantage of a metal femoral head component minimizes dislocation by using the large head, and since a dislocation can produce fatal results in older age patients with weakness and decreased compliance, reducing dislocation is particularly important.
There is some controversy about the side effects of metal-on-metal, because the potential effects of elevated levels of metal ions are poorly understood. Some authors claim there are concerns (e.g., hypersensitivity, carcinogenicity, and DNA damage) by the use of metal-on-metal articulations7829). But other authors report benefits (e.g., reduced renal insufficiency, malignancy, and even serum metal levels that do not differ from short- and intermediate term follow-up4).
Except for metal ion release from trunnion in older THA patients, large metal-on-metal articulation may be a good mechanical benefit and lower volumetric wear5).
In this study, there are some limitations. First, this was a retrospective study. Second, this is small size study including several etiologies for THA. It means that there is heterogeneity in terms of patient etiology. Thus, the finding of this study must be accepted and generalizing the results should be minimized without further study relating to etiology. Finally, there was no control group and we did not measured the metal ion concentration but only clinical issues and related factors.
Ceramic-coated large metal-on-metal articulations (ACCIS) are associated with a number of complications in elderly patients (e.g., cup loosening, groin pain, and even fatalities). In cases of communicated intertrochanter fracture (AO 31-A22,23) particularly, careful attention should be paid to the surgery approach selected.
References
1. Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982; 64:1295–1306. PMID: 7142237.

2. Turner RS. Postoperative total hip prosthetic femoral head dislocations. Incidence, etiologic factors, and management. Clin Orthop Relat Res. 1994; (301):196–204. PMID: 8156674.

3. Eswaramoorthy V, Moonot P, Kalairajah Y, Biant LC, Field RE. The Metasul metal-on-metal articulation in primary total hip replacement: clinical and radiological results at ten years. J Bone Joint Surg Br. 2008; 90:1278–1283. PMID: 18827235.
4. Grübl A, Marker M, Brodner W, et al. Long-term follow-up of metal-on-metal total hip replacement. J Orthop Res. 2007; 25:841–848. PMID: 17405158.

5. Leslie I, Williams S, Brown C, et al. Effect of bearing size on the long-term wear, wear debris, and ion levels of large diameter metal-on-metal hip replacements-An in vitro study. J Biomed Mater Res B Appl Biomater. 2008; 87:163–172. PMID: 18386846.
6. Signorello LB, Ye W, Fryzek JP, et al. A nationwide followup study of autoimmune and connective tissue disease among hip and knee implant patients. J Long Term Eff Med Implants. 2002; 12:255–262. PMID: 12627787.

7. Davies AP, Sood A, Lewis AC, Newson R, Learmonth ID, Case CP. Metal-specific differences in levels of DNA damage caused by synovial fluid recovered at revision arthroplasty. J Bone Joint Surg Br. 2005; 87:1439–1444. PMID: 16189324.

8. Willert HG, Buchhorn GH, Fayyazi A, et al. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am. 2005; 87:28–36.
9. Huddleston JI, Wang Y, Uquillas C, Herndon JH, Maloney WJ. Age and obesity are risk factors for adverse events after total hip arthroplasty. Clin Orthop Relat Res. 2012; 470:490–496. PMID: 21796477.

10. Whittle J, Steinberg EP, Anderson GF, Herbert R, Hochberg MC. Mortality after elective total hip arthroplasty in elderly Americans. Age, gender, and indication for surgery predict survival. Clin Orthop Relat Res. 1993; (295):119–126. PMID: 8403635.
11. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51:737–755. PMID: 5783851.
12. Advanced Ceramic Coated Implant System. Ceramic coated metal-on-metal large head total hip replacement surgical technique [Internet]. Buxtehude: Implantcast GmbH;cited 2017 Dec 12. Available from: http://oceaniaorthopaedics.com/wp-content/uploads/ACCIS-Large-head-op-tech.pdf.
13. Widmer KH. A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty. 2004; 19:387–390. PMID: 15067657.

14. Lee SW, Kim WY, Kang MS. Primary total hip arthroplasty using modified posterior approach through quadratus femoris flap osteotomy; comparison with conventional posterior approach. Hip Int. 2016; 26:543–549. PMID: 27739570.

15. Davis FM, Laurenson VG, Gillespie WJ, Wells JE, Foate J, Newman E. Deep vein thrombosis after total hip replacement. A comparison between spinal and general anaesthesia. J Bone Joint Surg Br. 1989; 71:181–185. PMID: 2925731.

16. Sikorski JM, Hampson WG, Staddon GE. The natural history and aetiology of deep vein thrombosis after total hip replacement. J Bone Joint Surg Br. 1981; 63-B:171–177. PMID: 7217137.

17. Silbersack Y, Taute BM, Hein W, Podhaisky H. Prevention of deep-vein thrombosis after total hip and knee replacement. Low-molecular-weight heparin in combination with intermittent pneumatic compression. J Bone Joint Surg Br. 1981; 63:171–177. PMID: 7217137.
18. Banerjee S, Pivec R, Issa K, Kapadia BH, Khanuja HS, Mont MA. Large-diameter femoral heads in total hip arthroplasty: an evidence-based review. Am J Orthop (Belle Mead NJ). 2014; 43:506–512. PMID: 25379747.
19. Cooper HJ, Della Valle CJ. Large diameter femoral heads: is bigger always better? Bone Joint J. 2014; 96-B(11 Supple A):23–26. PMID: 25381403.
20. Elkins JM, Callaghan JJ, Brown TD. Stability and trunnion wear potential in large-diameter metal-on-metal total hips: a finite element analysis. Clin Orthop Relat Res. 2014; 472:529–542. PMID: 24218160.

21. Stroh DA, Issa K, Johnson AJ, Delanois RE, Mont MA. Reduced dislocation rates and excellent functional outcomes with large-diameter femoral heads. J Arthroplasty. 2013; 28:1415–1420. PMID: 23602233.

22. Cicek H, Kilicarslan K, Yalcin N, Arslan E, Dogramaci Y, Yildirim H. Primary metal-on-metal total hip arthroplasty with large-diameter femoral heads: a clinical trial of 59 hips. Acta Orthop Belg. 2010; 76:758–765. PMID: 21302573.
23. Crowninshield RD, Maloney WJ, Wentz DH, Humphrey SM, Blanchard CR. Biomechanics of large femoral heads: what they do and don't do. Clin Orthop Relat Res. 2004; (429):102–107. PMID: 15577473.
24. Rodriguez JA, Rathod PA. Large diameter heads: is bigger always better? J Bone Joint Surg Br. 2012; 94(11 Suppl A):52–54. PMID: 23118381.
25. Cooper HJ, Della Valle CJ, Berger RA, et al. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012; 94:1655–1661. PMID: 23289127.
26. Dyrkacz RM, Brandt JM, Ojo OA, Turgeon TR, Wyss UP. The influence of head size on corrosion and fretting behaviour at the head-neck interface of artificial hip joints. J Arthroplasty. 2013; 28:1036–1040. PMID: 23528551.

27. Ala Eddine T, Remy F, Chantelot C, Giraud F, Migaud H, Duquennoy A. [Anterior iliopsoas impingement after total hip arthroplasty: diagnosis and conservative treatment in 9 cases]. Rev Chir Orthop Reparatrice Appar Mot. 2001; 87:815–819. French. PMID: 11845085.
28. Browne JA, Polga DJ, Sierra RJ, Trousdale RT, Cabanela ME. Failure of larger-diameter metal-on-metal total hip arthroplasty resulting from anterior iliopsoas impingement. J Arthroplasty. 2011; 26:978.e5–978.e8.

29. Visuri T, Pukkala E, Paavolainen P, Pulkkinen P, Riska EB. Cancer risk after metal on metal and polyethylene on metal total hip arthroplasty. Clin Orthop Relat Res. 1996; (329 Suppl):S280–S289. PMID: 8769342.

Fig. 1
Acetabular component design. Polar area: no contact between the bone and the component. Fit area: contact with the porous coated surface for bone ingrowth. Press fit area: circumferential press fit at the equator for primary implant stability.
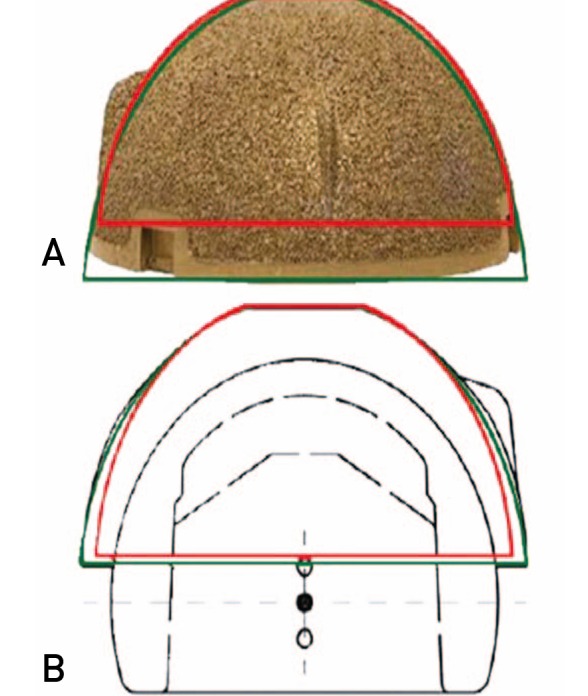
Fig. 2
Femoral heads and cone adapters. Each adapter is available in three different neck lengths in 4 mm increments and adapters are suited for femoral components with a 12/14 mm cone.

Table 1
Demographic Data
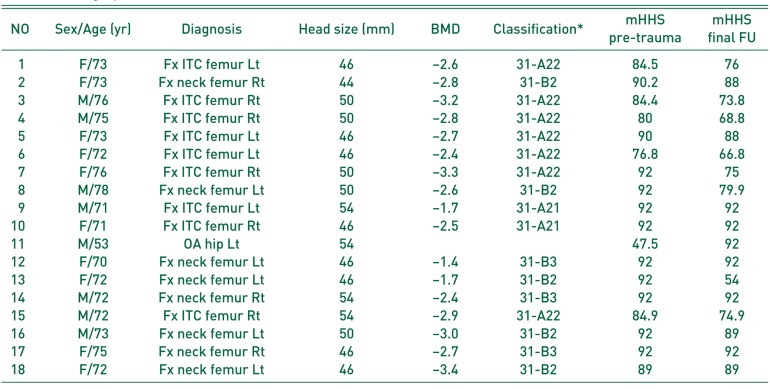
Table 2
Clinical Outcomes and Radiologic Outcomes




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download