Abstract
Purpose
The Korea Veterans Health Service (KVHS) implemented the ‘designated hospital system’ so that veterans can receive prompt medical attention at hospitals near their residences when experience medical emergencies, including hip fractures. We analyzed the hospital-selection process of Korean veterans following a hip fracture. We then evaluated (the validity and considerations) for choosing designated hospitals.
Materials and Methods
The study population consisted of 183 veteran patients (84 treated at a single veterans hospital and the remaining 99 treated at 39 designated hospitals) who underwent hip fracture between January 2010 and February 2015 in the Honam region of South Korea. The subjects were divided into the ‘nearest group’ (those who chose the hospital closest to their residences) and the ‘non-nearest group’ (those who did not choose the hospital closest to their residences). We compared the age, ambulatory status, combined disease and fracture type, factors that we speculated may impact hospital choice.
Results
Although the patients had difficulty moving due to hip fractures, 116 (63.4%) patients choose hospitals that were not closest to their residences. Patients with three or more comorbidities (P=0.028) and older ages (P=0.046) were statistically more likely to fall into the non-nearest group. Ambulatory status and fracture type were shown not to significantly impact choice between nearest and non-nearest hospital. Patients in the non-nearest group tended to seek care at larger hospitals.
Most Korean veterans patients are older aged (over 70 years) and have an increased risk of hip fracture compared to the general public due to falls and osteoporosis. Hip fractures in elderly patients are becoming an increasingly concerning social problem and can have a serious effect on life; beyond being a life-threatening condition, it may also seriously degrade activities of daily living and quality of life1234). Since 1986, the Korea Veterans Health Service (KVHS) has implemented the neighboring designated hospital (hereafter referred to as the designated hospital) system to prevent delays in medical care while getting to veterans hospitals56). This is particularly relevant to those veterans with hip fractures since it can be challenging to transfer over long distances with this condition and since it requires immediate medical attention. In selecting designated hospitals, accessibility has been emphasized for users' need for convenience and there is currently great demand on beneficial facilities near their place of residence. Studies on the designation of appropriate medical care facilities have been carried out in other countries, and the results suggest that it is important to select designated hospitals close to patient's residence to avoid delays in treatment that may occur due to the long traveling distance67891011). However, these kinds of studies have not been performed in Korea and here we aimed to investigate whether Korean patients with hip fractures who are also veterans seek medical care at the hospital nearest to their residences, as mentioned in foreign research. Furthermore, we evaluated (the validity and considerations) for choosing designated hospitals.
This study collected data from patients with hip fractures who were also veterans between January 2010 and February 2015 in the Honam region (consisting of two provinces and one metropolitan city) of South Korea. Medical records from the subject hospitals and designated hospitals' data submitted to the KVHS-affiliated Referral Hospital Management Organization were retrospectively reviewed. Of the 202 patients who were veterans, 183 cases (84 who were treated at a single veterans hospital and 99 who were treated at 39 other designated hospitals) were reviewed. We excluded those who had hip fractures in places other than residential areas. All subjects were males and there were no cases of bilateral hip fractures.
The institutional review board of authors' hospital approved the design and protocol of this retrospective study (GJVH-IRB No. 2015-11-5). All patients were informed that their medical data could be used in a scientific study and provided their consent.
Patient age and body mass index were examined and fracture types were characterized as either femur neck fracture or intertrochanteric fracture depending on the fracture site. Dementia and comorbid medical illnesses were identified, and patients with more than three comorbidities were grouped into their own category. Pre-injury ambulatory status was evaluated using the Koval classification.
Of the 183 cases included in our analysis, patients who chose the hospital nearest to their residences were placed into the “nearest group”, while those who did not choose the hospital nearest to their residences were placed into the “non-nearest group”. The travel distance from patient's residence to the selected hospital was measured by locating the shortest distance in Naver Map (5 km, 5–10 km, 10–20 km, 20–30 km, 30–40 km, 40–50 km, and longer than 50 km). The number of hospital beds and departments were also considered as possible factors influencing hospital selection and we examined these as possible predictors of patients falling into the non-nearest group. To identify whether surgery was performed more promptly at a hospital with easier accessibility, the waiting time for surgery (the duration from injury to surgery) was compared between the two groups.
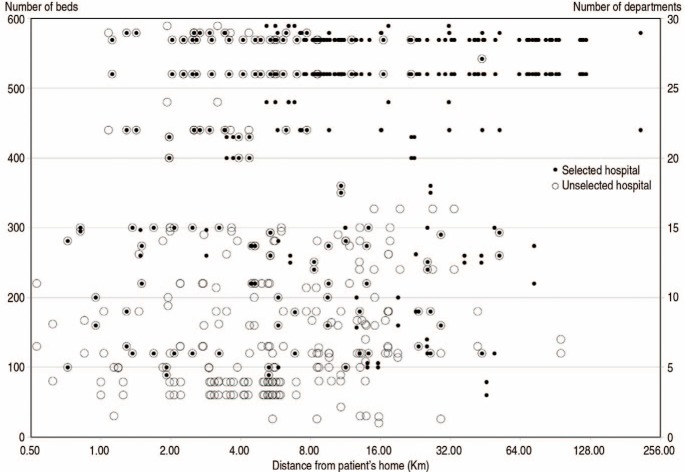
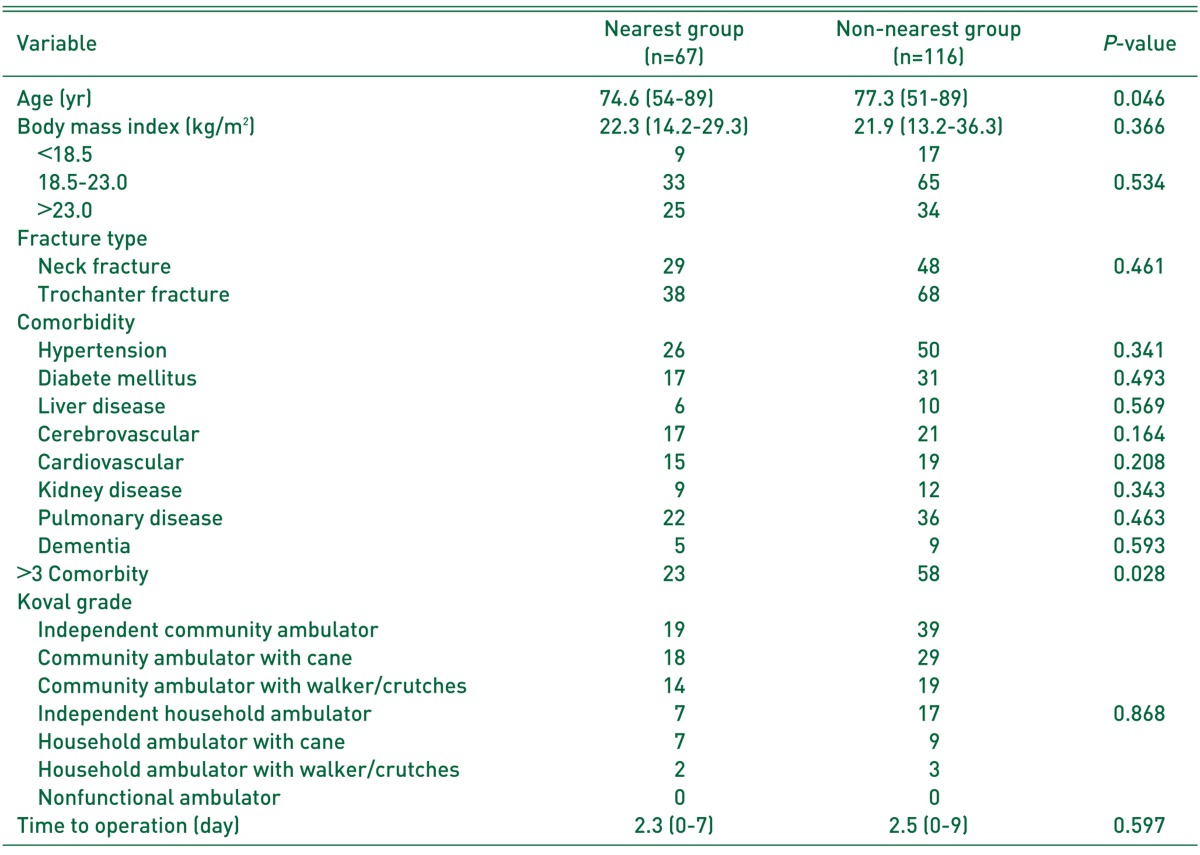
Of the 183 patients included in our study, 67 (36.6%) and 116 (63.4%) were placed into the nearest and non-nearest groups, respectively. We noted that the percentage of patients who did not choose the hospital nearest to their residences was higher. No significant difference was shown in body mass index (P=0.366), fracture type (P=0.461) and pre-injury ambulatory status (P=0.632) between the two groups. No significant difference was observed in 8 comorbidities including dementia, circulatory and respiratory medical problems and others between the two groups. The non-nearest group was older in age (P=0.046), and had more than three comorbidities (P=0.028). There was no significant difference in the mean duration from injury to surgery between the two groups (2.3 days; range, 0–7 days) in the nearest group (2.5 days; range, 0–9 days) in the non-nearest group (P=0.597) (Table 1).
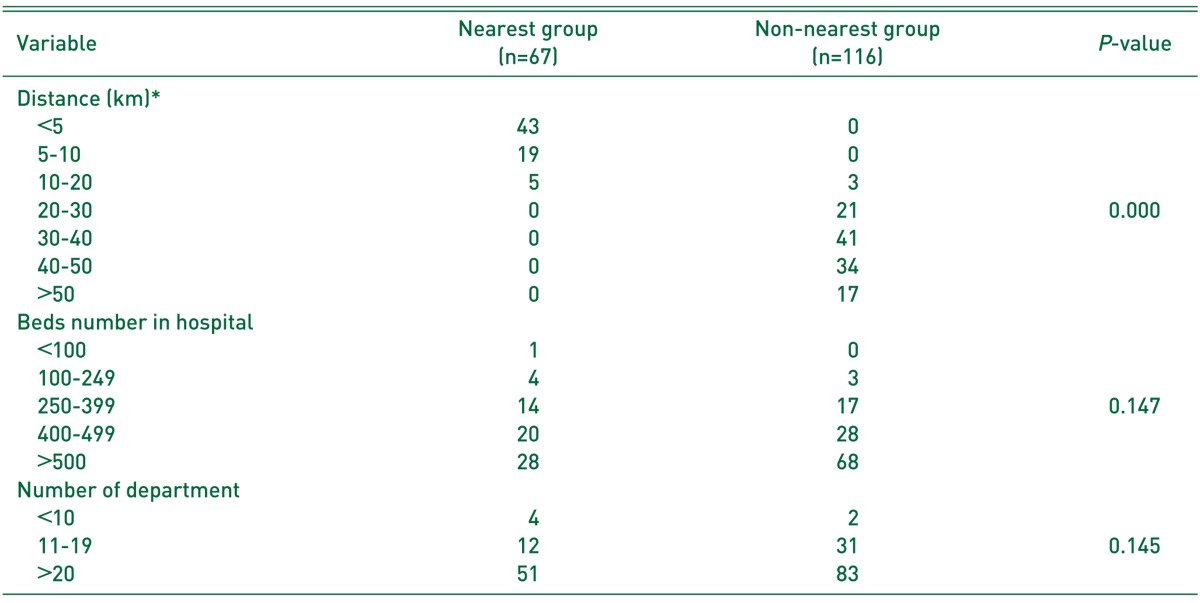
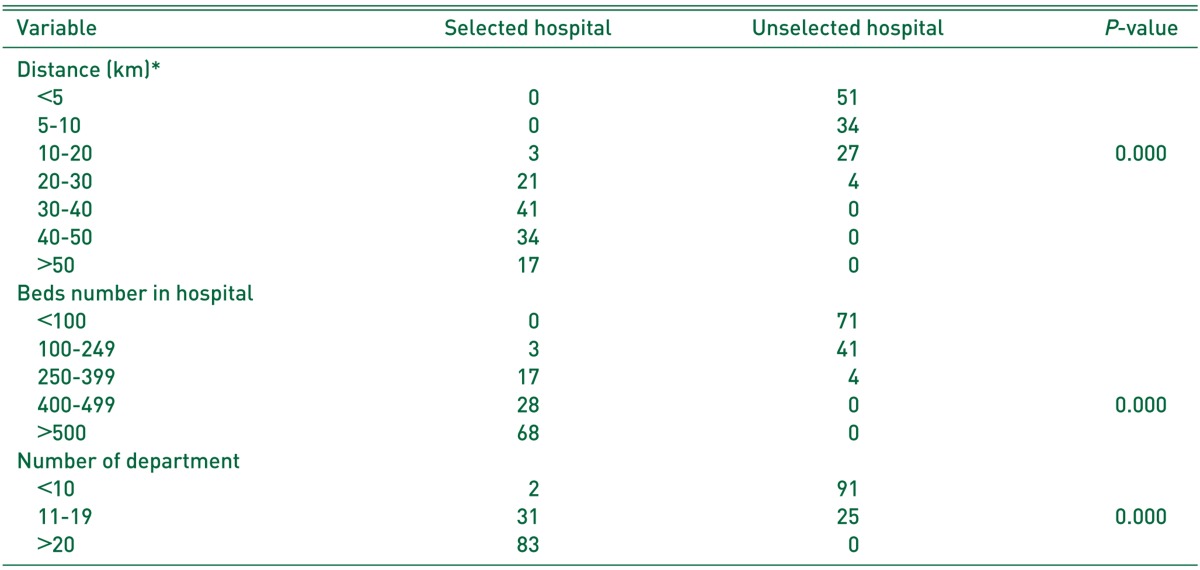
Of all 67 patients in the nearest group, 43 (64.2%) chose hospitals located within a distance of 5 km from their residences, 19 (28.4%) selected a hospital between 5–10 km and 5 (7.5%) chose a hospital between 10–20 km away from their residence. Of the 116 patients in the non-nearest group, 113 (97.4%) chose hospitals located at distances longer than 20 km from their residences (20–30 km, 21; 30–40 km, 41; 40–50 km, 34; and longer than 50 km, 17), and only 3 received treatment at hospitals located at a distance between 10–20 km (Table 2). In the assessment of number of departments, 51 of 67 patients (76.1%) in the nearest group and 83 of 116 (71.6%) in the non-nearest group received medical care in hospitals with more than 20 departments. In regards to the number of beds, 48 of 67 (71.6%) in the nearest group and 96 of 116 (82.8%) in the non-nearest group selected hospitals with more than 400 beds (Table 2). Distance from patient's residence and hospital size were compared between selected and unselected hospitals in the non-nearest group that chose the hospital at far distance from residence at the cost of inconvenience, instead of the nearest hospital. The travel distance between unselected hospitals and residences was significantly shorter (P=0.000), but the number of beds (P=0.000) and number of departments (P=0.000) in unselected hospitals were significantly smaller than those of selected hospitals (Table 3, Fig. 1).
The KVHS was established in November 1981 as an affiliated organization of the Ministry of Patriots and Veterans Affairs as a quasi-governmental organization that provides medical care and welfare support for veterans. They perform this function entrusted by the government, and are currently operating 5 veterans hospitals12). As the number of veterans continues to grow (655,580 veterans as of February 2016)12), veterans have difficulties in visiting veterans hospitals located far from their residences along with the rapid aging of the country. In particular, greater difficulties are present in elderly veterans with conditions that require early surgical treatment such as hip fracture. The KVHS has implemented the designated-hospital system so that veterans who experience medical emergencies can receive prompt medical attention at referral hospitals near their residences by designating some medical centers as veterans hospitals6).
Referral hospitals are designated by initially evaluating eligibility criteria including management environment of the voluntary hospitals, accessibility, medical workforce, facilities and equipment, pharmaceutical expenditure, prescription patterns and others and by comprehensively considering the distribution of veterans in a corresponding area. Beginning with 2 hospitals in Jeju in 1986, 314 designated hospitals are being operated nationwide as of September 20166). The United States government has operated a similar system since November 1999, and studies on the use of veterans and designated hospitals for emergency patients have been conducted in order to select appropriate referral hospitals and evaluate their usefulness for veterans7891011). Specifically, many studies have investigated hip fractures891011) that cause difficulty walking after injury and require immediate surgical interventions to lower mortality131415). However, no prior studies have investigated the selection criteria and utilization of designated hospitals in Korea, which implemented the designated hospital system 13 years earlier than the United States.
Death after hip fracture is affected by several factors including: i) the presence and severity of medical illnesses, ii) the length of time from injury to surgery, and iii) others11131415). Richardson et al.10) reported that about 20% of veterans were living at residences greater than 20 miles from their designated veterans hospitals. Of these, more than 1/3 of veterans did not seek treatment at veterans hospitals when experiencing a medical emergency. Since the risk of delayed surgery and mortality were greater when veterans hospitals were located more than 50 miles apart from patient's residence, they suggested that it is important not to delay surgical treatment in veterans patients with hip fracture. To solve these problems, they asserted that more hospitals close to residential areas need to be designated to allow easier access to medical care for veterans patients with hip fracture. In addition to the investigation of Richardson et al.10), previous studies reported that survival rates were lower as the distance between a patient's residence and a veterans hospital increased when hip fractures requiring immediate attention occurred to veterans161718).
The results of our study demonstrate that patients who were presumed to be at higher risk for traveling long distances due to older age, poorer ambulatory ability and more comorbid conditions chose hospitals with the higher number of beds and departments, instead of the nearest hospital. Unlike similar studies in other countries, no significant difference was found in the waiting time for surgery between the nearest and non-nearest groups. The authors propose that the distance between the medical care facility and patient's residence is not a critical factor associated with delays to surgery in Korea, since a relatively small land area and excellent public transit and road systems enable more convenient travel. According to an overseas study, the mortality rate was lower when hospitals at which the fracture surgery was performed was located in an urban area19) and a teaching hospital20). Therefore, it may be considered necessary to select a teaching hospital within an urban area designated as a teaching hospital first. Our study results were comparable to those of domestic and international studies in which patients were more concerned about the size of a hospital rather than accessibility to medical facilities in hospital selection2122). Our study results are expected to provide an excellent reference base for offering treatment efficiency and convenience in a traumatic or critical condition of each patient seeking for treatment at a designated hospital and will be a good standard to cope with the needs of each region in the selection of designated hospitals in the future.
This study was limited by the relatively small sample size and the relatively short follow-up period. This study population was limited to those who live in the Honam region, instead of comprising the general Korean population. Furthermore, out study analyzed only limited criteria including the number of beds and department, and there are a wide variety of other conditions that may be important to veterans when choosing a hospital. Additional studies are warranted to further identify other critical conditions requiring emergent medical care such as cardiovascular and cerebrovascular diseases by comprising a much larger sample size nationwide.
We identified multiple considerations that may be taken into account when selecting hospitals meeting the designated standard. Multiple medical clinics near residential areas should be designated for simple outpatient care, and at least one medical facility with more than 10 departments and 400 beds within a distance of 30 km from patient's residence should be designated. Considering hospital size (the number of beds or departments) rather than accessibility for patients requiring hospital admission and surgery was deemed important. This study only consisted of veterans who were receiving government-funded medical care from designated hospitals and has no association with selection criteria for medical services of general patients.
References
1. Sterling DA, O'Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma. 2001; 50:116–119. PMID: 11231681.

2. Hall SE, Williams JA, Senior JA, Goldswain PR, Criddle RA. Hip fracture outcomes: quality of life and functional status in older adults living in the community. Aust N Z J Med. 2000; 30:327–332. PMID: 10914749.

3. French DD, Werner DC, Campbell RR, et al. A multivariate fall risk assessment model for VHA nursing homes using the minimum data set. J Am Med Dir Assoc. 2007; 8:115–122. PMID: 17289542.

5. Radcliff TA, Henderson WG, Stoner TJ, Khuri SF, Dohm M, Hutt E. Patient risk factors, operative care, and outcomes among older community-dwelling male veterans with hip fracture. J Bone Joint Surg Am. 2008; 90:34–42. PMID: 18171955.

6. Ministry of Patriots & Veterans Affairs. The treatment guide and the list of trust hopitals [Internet]. Sejong: Ministry of Patriots & Veterans Affairs;2014. cited 2017 Jan 1. Available from: http://www.mpva.go.kr/support/support250_view.asp?id=1982&ipp=10.
7. Gordon HS, Aron DC, Fuehrer SM, Rosenthal GE. Using severity-adjusted mortality to compare performance in a Veterans Affairs hospital and in private-sector hospitals. Am J Med Qual. 2000; 15:207–211. PMID: 11022367.
8. Lapcevic WA, French DD, Campbell RR. All-cause mortality rates of hip fractures treated in the VHA: do they differ from Medicare facilities? J Am Med Dir Assoc. 2010; 11:116–119. PMID: 20142066.

9. Hutt E, Radcliff TA, Henderson W, Maciejewski M, Cowper-Ripley D, Whitfield E. Comparing survival following hip fracture repair in VHA and non-VHA facilities. Geriatr Orthop Surg Rehabil. 2015; 6:22–27. PMID: 26246949.

10. Richardson KK, Cram P, Vaughan-Sarrazin M, Kaboli PJ. Fee-based care is important for access to prompt treatment of hip fractures among veterans. Clin Orthop Relat Res. 2013; 471:1047–1053. PMID: 23322188.

11. Bass E, French DD, Bradham DD, Rubenstein LZ. Risk-adjusted mortality rates of elderly veterans with hip fractures. Ann Epidemiol. 2007; 17:514–519. PMID: 17420142.
12. Ministry of Patriots & Veterans Affairs. Basic status of Veterans subject to end of July 2016 (including area) [Internet]. Sejong: Ministry of Patriots & Veterans Affairs;2016. cited 2017 Jan 1. Available from: http://www.mpva.go.kr/info/info600_view.asp?id=5621&ipp=50.
13. Orosz GM, Magaziner J, Hannan EL, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004; 291:1738–1743. PMID: 15082701.

14. Bottle A, Aylin P. Mortality associated with delay in operation after hip fracture: observational study. BMJ. 2006; 332:947–951. PMID: 16554334.

15. Lefaivre KA, Macadam SA, Davidson DJ, Gandhi R, Chan H, Broekhuyse HM. Length of stay, mortality, morbidity and delay to surgery in hip fractures. J Bone Joint Surg Br. 2009; 91:922–927. PMID: 19567858.

16. Bernstein J. Fee-based care is important for access to prompt treatment of hip fractures among veterans. Clin Orthop Relat Res. 2013; 471:2036. PMID: 23546849.
17. Wallace AE, Weeks WB, Wang S, Lee AF, Kazis LE. Rural and urban disparities in health-related quality of life among veterans with psychiatric disorders. Psychiatr Serv. 2006; 57:851–856. PMID: 16754763.

18. Wallace AE, West AN, Booth BM, Weeks WB. Unintended consequences of regionalizing specialized VA addiction services. Psychiatr Serv. 2007; 58:668–674. PMID: 17463348.

19. Marshall T, Suthersan M, Chan MK, et al. Mortality and morbidity of neck of femur fractures: A comparison between Orange and peripheral centres. Aust J Rural Health. 2016; 24:253–257. PMID: 26691875.

20. Weller I, Wai EK, Jaglal S, Kreder HJ. The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg Br. 2005; 87:361–366. PMID: 15773647.

21. Lane PM, Lindquist JD. Hospital choice: a summary of the key empirical and hypothetical findings of the 1980s. J Health Care Mark. 1988; 8:5–20.
22. Cho WH, Kim HJ, Lee SH. A study on the criteria for selection of medical care facilities. Korean J Prev Med. 1992; 25:53–63.
Fig. 1
Scatter plots according to distance traveled, number of beds and number of department in selected and unselected hospitals between the nearest and non-nearest groups.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download