Abstract
Purpose
Femoral intertrochanteric fractures are common in the elderly. Appropriate surgical fixation of trochanteric fracture fragments can restore normal anatomical structure and ambulation, and can aid in the recovery of biomechanical function of the hip. We evaluated clinical outcomes of bipolar hemiarthroplasty using a wiring technique for trochanteric fracture fragment fixation.
Materials and Methods
From September 2006 to February 2015, a total of 260 cases underwent simultaneous bipolar hemiarthroplasty and wire fixation. A total of 65 patients (69 hips) with an average age of 78 years and more than one year of follow-up was included in the study. Using pre-, postoperative and follow-up radiograms, we evaluated wire fixation failure and also assessed changes in walking ability.
Results
Loosening or osteolysis around the stem was not observed; however, we did observe bone growth around the stem (54 cases), cortical hypertrophy (6 cases), a wide range of sclerotic lines but no stem subsidence (1 case), wire breakage (9 cases), and fracture fragment migration with no significant functional deficiency (2 cases).
Conclusion
Our study showed that additional wiring for trochanteric fracture fragment fixation following bipolar hemiarthroplasty can help restore normal anatomy. The added stability results in faster rehabilitation, and good clinical and radiographic outcomes. We recommend this procedure in this type of fracture.
The incidence of femoral intertrochanteric fractures, in particular unstable comminuted fractures, is gradually increasing with the recent growth of the elderly population. Patients with this fracture have high rates of complications and mortality due to their higher mean age and a large number of underlying diseases. For this reason, they are associated with increased requirements for appropriate surgical procedures and patient care.
Femoral intertrochanteric fractures occur in the metaphyseal region, unlike femoral neck fractures, and have a much higher rate of bone union. Osteosynthesis with a dynamic hip screw and a proximal femoral intramedullary nail has been considered as the standard fixation method for this fracture type. However, previous studies have documented high fixation failure rates, ranging between 6-32%12345). In particular, a higher failure rate is anticipated in osteoporotic elderly patients with poor bone quality such as varus displacement and femoral head perforation. Moreover, prolonged bedridden status results in worsening of medical and psychiatric problems for patients with multiple underlying diseases, and therefore, bipolar hemiarthroplasty (BPHA), favorable for early ambulation, has been recently suggested as another surgical option for elderly patients678).
There are several technical issues to consider when performing BPHA. First, it is technically challenging to adjust leg lengths because of a fracture involving the greater and lesser trochanters, which are reference points for reconstruction of leg length. Second, it may be difficult to achieve initial fixation due to comminuted fractures of the proximal femur. Lastly, reduction and fixation of trochanteric fragments which serve as attachment points of the iliopsoas and abductor muscles is also challenging. Nonetheless, reduction and fixation of these fragments should be achieved because muscles attached to the trochanters play a pivotal role in restoring walking ability and preventing dislocation postoperatively910).
The authors used several wiring techniques for trochanteric fragments fixation after BPHA for intertrochanteric fractures. This study aimed to introduce our wiring techniques and report the clinical and radiographic outcomes.
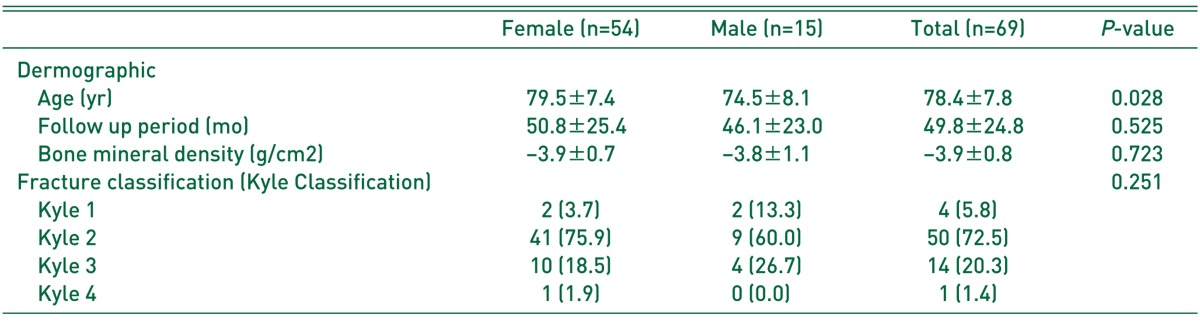
This study retrospectively reviewed 65 patients (69 hips) among 251 of 260 intertrochanteric fracture patients who underwent BPHA with cementless stem and wiring for fixation of trochanteric fracture fragments from October 2006 to February 2015. We excluded 182 cases (including 43 patients who died within 1 year) who could not be follow-up for at least 1 year and 9 cases with preoperative ambulation impairment. Of these, radiographic results were obtained from 55 patients through outpatient observation and clinical results only from 14 patients via telephone calls. The minimum follow-up period was one year, whereas a maximum follow-up period was 7 years and 9 months. The mean patient age was 78 years (range, 64-99 years) and 14 were male and 51 female. According to bone mineral density tests, 25 patients had a mean T-score of −3.9, indicating severe osteoporosis. The Kyle classification was used to classify fracture type. There were 4 Type 1, 50 Type 2, 14 Type 3, and 1 Type 4 fractures (Table 1). Even if the fracture pattern was stable (Type 1) on preoperative radiographs, wiring fixation was performed when further trochanteric fracture was detected intraoperatively.
The Kyle classification used in the present study simply categorizes different types of fractures based on anteroposterior (AP) view of preoperative radiographs. Table 1 shows the distribution of fracture type; however, fracture type determined during surgery may be different from radiographic findings. Although Type 1 fractures had almost no displacement on AP views, displaced fracture fragments were laterally detected at the junction of the gluteus medius and external rotator muscles. In Type 2, fracture fragments were often found in the greater trochanter in addition to the lesser trochanter. Bone fragments of the greater and lesser trochanters may be stuck together or separately comminuted, and vary in size and shape. A bone fragment from the greater trochanter including the junction of the gluteus medius and external rotator muscles tended to rotate externally and be displaced posteriorly, whereas a bone fragment from the lesser trochanter tended to be displaced anteromedially.
All operations were performed by a single surgeon using a transgluteal approach in a supine position. BPHA was carried out using Bencox® (Corentec, Seoul, Korea) bipolar cups and cementless femoral stems in all patients. In arthroplasty procedures of the hip, three measuring methods are used in combination for anatomical reconstruction of leg length. The first method is head-lesser trochanter distance. The lengths of the stem and femoral neck were intraoperatively determined according to head-lesser trochanter distance measured preoperatively on the contralateral hip. When the lesser trochanter was broken and displaced, the tip of the lesser trochanter was predicted by extending the shape of lesser trochanter remaining in the distal portion. In cases of fracture fragments involving the entire lesser trochanter, head-lesser trochanter distance restored in the area where a lesser trochanter fragment was separated from the proximal femur was measured after assessing the lesser trochanter fragment size on preoperative radiographs and considering pre-fracture position. Based on preoperative parameters, leg length was reconstructed by adding fragment size and the distance from the head center to the lesser trochanter. The second method involves lower limb tension. Soft tissue tension was assessed using the shuck test by temporally implanting trial components of the femoral stem. The third technique is the direct method for measuring leg length discrepancy. Taking into account temporary reduction without the bipolar cup, true leg-length discrepancy was assessed by measuring the distance between the anterior superior iliac spine and the medial malleolus of ankle.
The lesser trochanter fragment is usually anteromedially displaced by the iliopsoas muscle being broken partially or entirely as one large fragment. Early in our experience, when presented with cases of Incomplete displaced fractures with simple fracture line, ‘simple oblique wiring’ was used by coiling a wire two or three times around superior to the lesser trochanter to prevent gliding down the wire. When the entire lesser trochanter was displaced as one large fragment, stability of ‘simple oblique wiring’ seemed to be insufficient. For this reason, a hole was drilled in the lesser trochanter to provide sufficient rigidity of fixation. However, ‘simple oblique wiring’ is not useful for reduction of displaced or small lesser trochanter fragments because it can only hold the superior to the lesser trochanteric fragment. ‘Wiring using bone hole’ is an uneasy procedure to drill a hole by pulling the lesser trochanter in significantly displaced lesser trochanter fractures and cannot be used in comminuted fragments. Furthermore, lesser trochanter fractures can occur while drilling. For these reasons, we devised ‘candy-package wiring’ (Fig. 1). In this technique, two wires were inserted to the upper and lower portion of psoas involving lesser trochanter fragments before stem insertion, and tied anteroposteriorly in a figure of candy package for holding the bone fragments and the psoas, and then reduction was done by adjusting tied wires after stem insertion11).
Early in our experience, simple transverse wiring was performed using a ‘wire passer’ which was tied transversely two or three times over the greater trochanter fragment by making wire knots on the lateral aspect. This technique was then modified to offset muscle force displacing superiorly by the gluteus medius. The modified technique, known as ‘transverse wiring with distal pulling wire’ (Fig. 2). It was performed by tying a wire transversely over the greater trochanter and drilling holes through the anterior cortex to enhance fixation, and then the wire was pulled distally and tied once more to the superior or inferior portion of the lesser trochanter.
When conducting wiring to fix complex or comminuted trochanteric fragments, transverse wiring with distal pulling wire alone is insufficient to fix each fragment and get rigidity due to narrow contact area. In these cases, adding a ‘figure-8 type wiring’ is effective. Figure-8 type wiring (Fig. 3) is conducted by tying two wires over the greater trochanter making a figure-8 anteroposteriorly and then wires were placed again inferior to the lesser trochanter laterally. Additionally, these wires tied over the trochanteric area can be useful in reconstructing the gluteus minimus, gluteus medius and the portion of the vastus lateralis that are split in a transgluteal approach. All wiring techniques were performed after insertion of the stem and reduction of the hip excepting candy-package wiring. Approximately 10 to 20 minutes were taken to complete wiring fixation. Thicker wires (1.5 mm thick) were used in all operations, and several wiring techniques were combined depending on the fracture type (Fig. 4, 5).
Exercise of the knee and hip joints was allowed from the first operative day. Weight-bearing ambulation was started using a walker, ambulation assist device, or crutches to the extent that the patient's condition permitted. All patients were encouraged to ambulate using aids for 3 months after surgery and followed up postoperatively at 6th week, 3rd, 6th month, 1st year, and at annual intervals afterwards.
Postoperative clinical and radiographic results were analyzed. For assessment of clinical results, pre-and postoperative pain was measured using the visual analogue scale (VAS) scale and postoperative ambulatory recovery was evaluated using Clawson's Ambulation Capacity Classification. For assessment of radiographic findings, the radiographs of 55 hips available for a minimum follow-up of 1 year were analyzed at their latest follow-up. By dividing AP and lateral radiographs into seven Gruen zones, biological fixation, osteolysis, femoral cortical thickening, radiolucent lines around the femoral component, sclerotic lines and subsidence were checked. Furthermore, wire breakage, nonunion and fracture migration of trochanteric fragments were also examined. Anterior and posterior radiographs of the pelvis including both hip and femoral radiographs of the surgical site were taken. When taking the films, the distance between the X-ray tube and the pelvic bone was maintained at 1 m, and the bone and film distance was kept at 20 cm. To determine femoral stem stability, vertical subsidence was assessed radiologically. Taking into consideration the magnification ratio of AP radiographs taken immediately after surgery and at the final follow-up, subsidence of the stem was determined by measuring the distance from the proximal tip of the greater trochanter to the superior-lateral shoulder of the stem. When the position of the greater trochanter was unclear, the displacement between the distal end of the fracture and the shoulder of the stem increased by more than 5 mm in radiographs was considered as a significant subsidence. In addition, the presence of complications such as dislocation, infection and wire breakage was examined.
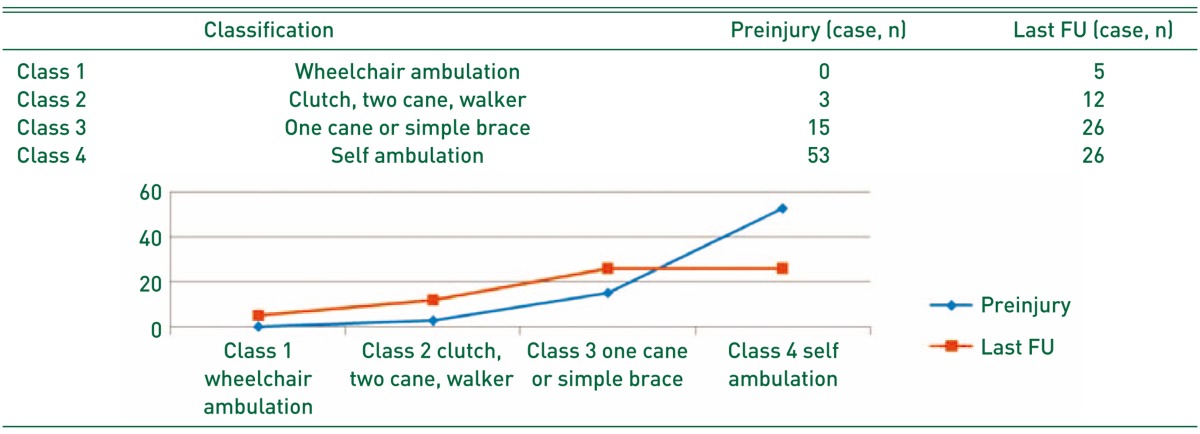
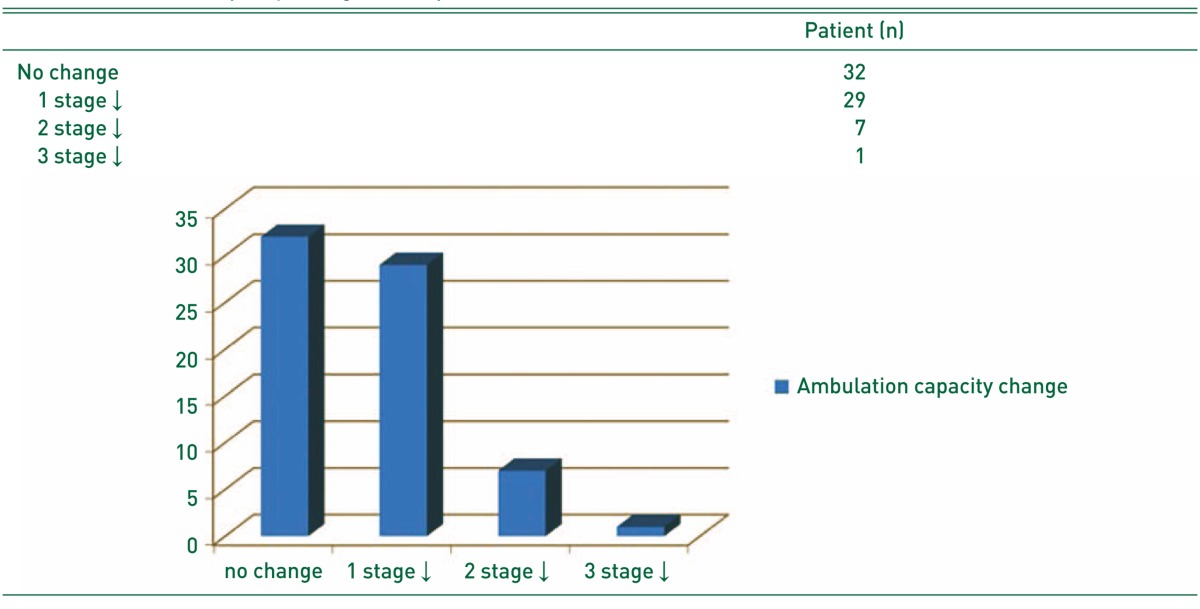
The VAS score was used to assess clinical status. The mean VAS score was significantly reduced from 8.5 preoperatively to 0.65 at final follow-up. In the evaluation of postoperative ambulatory ability, 26 patients ambulated independently without any assistive device (class 4), 26 patients were graded as ambulatory with a cane (class 3), 12 as ambulatory with a walker (class 2) and 5 as nonfunctional ambulatory status (class 1). In the older age group, with a mean age of 78 years, 32 patients (46.4%) were able to preserve their pre-injury ambulatory ability, 29 (42.0%) dropped their ambulatory ability by one level, 7 (10.0%) dropped by two levels, and 1 (1.4%) dropped by three levels from class 4 to class 1. A case with dropped ambulatory ability by three levels was an 85-year old female patient who was followed up for 2 years, and she was unable to walk due to heart failure, pneumonia and other internal medical problems after maintaining class 4 for the first postoperative year (Table 2, 3).
Radiographic results were analyzed in 55 of 69 patients who were able to get radiographs for a minimum of 1 year after surgery. Aseptic loosening or osteolysis of the femoral component was not detected in any patient. Bone ongrowth was observed in 54 cases (78.3%) and cortical hypertrophy in 6 (8.7%). One case (1.4%) had an extensive sclerotic line surrounding the femoral component, but showed no finding of subsidence of the femoral stem. Breakage of the wire used for trochanteric fragment fixation was detected in 9 cases (13.0%), while nonunion and superior displacement of greater trochanteric fracture fragments was found in only 2 cases (2.9%). These two patients dropped their ambulatory ability by one level from class 4 to 3.
There were concerns about delays in operating time and infection caused by manipulation of soft tissues and bone fragments, but no cases with superficial or deep infection were yet observed. No patient had wire removal due to irritation by wire knot or bursitis following wiring fixation. Furthermore, postoperative dislocations were not observed. Delirium occurred in 10 patients (15.4%), but resolved spontaneously within 4 postoperative days in all cases. Clinical symptoms of pneumonia were detected in 2 cases (2.9%), and relieved after a 2-week course of antibiotic treatment as an interdisciplinary treatment approach. In addition, there were no complications including pulmonary embolism acquired during a hospital stay, myocardial infarction, infarction and others caused by a thrombus.
Femoral intertrochanteric fractures are most common among the elderly and caused by a low-energy injury, but this fracture type has a comminuted fracture pattern. For classification of femoral intertrochanteric fractures, a variety of classification systems have been used including Boyd and Griffin classification, Tronzo classification, Kyle classification, Evans classification and AO classification (currently the most commonly used classification system). However, the AO classification may not reflect real fracture patterns, since this system is a simplified version that guides the determination of treatment options and prognosis12). This study was meaningful in that it introduced a wide range of wiring methods for reduction and fixation of various fracture patterns and documented their clinical outcomes using single or combined wiring techniques.
In the present study, 61 cases (88.4%) demonstrated no change or a decrease in ambulatory ability by one level when walking ability at the final follow up was compared to pre-injury ambulation status, and this study was clinically compatible and achieved better results compared to previous studies that performed internal plate fixation or hip arthroplasty for management of intertrochanteric fractures13141516). In our study, there were no cases of dislocation, and this appears to be attributable to no injury in the external rotator muscles of the hip due to transgluteal approach, effective restoration of leg length, and restoration of soft tissue tension thereby reduction of greater and lesser trochanteric fragments101718). When conducting wiring fixation for reattaching trochanteric fragments, the possibility of extended operating time and infection caused by increased manipulation of bone fragments is expected to increase. However, superficial or deep infections were not observed in this study. This outcome seems to be the result of not requiring wider skin incisions and only 10 to 20 minutes of actual operating time spent for wiring fixation.
Unlike femoral neck fractures, technical challenges may be experienced when performing BPHA in unstable intertrochanteric fractures. First, it is difficult to restore a leg length because the greater and lesser trochanters, a reference point for restoration of leg length, are not in their normal anatomical positions. Accurately reconstructing the leg length is an important factor for implant stability and postoperative ambulation. We used head-lesser trochanter distance measured the contralateral hip preoperatively19), and in the case of an inaccurate parameter, adjusted leg length by examining proper soft tissue tension after reduction and measuring true leg length. Second, another difficulty is achieving initial stability. Although the use of a cemented stem has been proposed to solve this problem202122), this is limitedly used because of a high mortality risk caused by fat embolism, cement embolism, vasodilation due to autonomic reflex and others in elderly patients with cardiovascular diseases23). We ensured solid fixation by using a cementless, double tapered, rectangular wedge-shaped, straight stem (Bencox®), and obtained excellent clinical and radiographic results at 2-year follow up2425).
Finally, reduction and fixation of fractures in the greater or lesser trochanters are challenging. The gluteus minimus and medius being responsible for abduction attach to the greater trochanter of the femur. When these muscles are insufficiently fixed, pain may persist and the Trendelenburg gait may occur because the center of the head cannot serve as a lever at the leverage point of the abductor migrates. A previous study suggested that abductor weakness and the displaced greater trochanter fragment are profoundly linked and that fragment displacement of greater than 2 cm may result in significant abductor weakness26). Moreover, since the lesser trochanter is an attachment site for the psoas and flexor muscles, and gait disturbances resulted from abnormal hip flexion and dislocation caused by a decrease of soft tissue tension around the hip may occur if the lesser trochanteric fragment is not reduced. Several studies have addressed a variety of surgical techniques and instruments by paying attention to the importance of fixation of the greater and lesser trochanters272829). However, these instruments have led to unsatisfactory outcomes, and a study reported that complication rates were 30% for nonunion and 25.8% for irritation symptoms after using a grip plate28). Wiring fixation of the greater trochanter originated from a study on trochanteric osteotomy. Amstutz et al.26) stated a nonunion rate of 4.9% after trochanteric osteotomy. In order to achieve stable fixation, Amstutz et al.26) recommended using more than two wires, and Boardman et al.30) suggested using more than three wires. Likewise, strong stable fixation is required to offset abductor muscle strength. For this reason, we used a wire with a thickness of more than 1.5 mm and combined 2 to 3 wiring techniques depending on fracture patterns and severity. As a result, nonunion was detected in only 2 cases (2.9%), and this was considered as a relatively satisfactory clinical outcome.
This retrospective study was limited by the relatively small sample size and the relatively short follow-up period (as little as 1 year). Further studies with long-term follow-up and larger sample sizes are warranted to more clearly and objectively confirm the effectiveness of wiring fixation and identify potential postoperative complications including infection, nonunion and dislocation and others.
In our study, wiring fixation is considered a good surgical option for trochanteric fracture fragment fixation when performing BPHA for the treatment of femoral intertrochanteric fractures as it promotes rehabilitation and prevents dislocation in elderly patients. Choice of appropriate wiring techniques will depend on the fracture type and is thought to be crucial for achieving favorable clinical outcomes.
References
1. Kyle RF, Gustilo RB, Premer RF. Analysis of six hundred and twenty-two intertrochanteric hip fractures. J Bone Joint Surg Am. 1979; 61:216–221. PMID: 422605.

2. Haentjens P, Casteleyn PP, De Boeck H, Handelberg F, Opdecam P. Treatment of unstable intertrochanteric and subtrochanteric fractures in elderly patients. Primary bipolar arthroplasty compared with internal fixation. J Bone Joint Surg Am. 1989; 71:1214–1225. PMID: 2777850.

3. Lu-Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am. 1994; 76:15–25. PMID: 8288658.

4. Hardy DC, Descamps PY, Krallis P, et al. Use of an intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures. A prospective, randomized study of one hundred patients. J Bone Joint Surg Am. 1998; 80:618–630. PMID: 9611022.

5. Kim WY, Han CH, Park JI, Kim JY. Failure of intertrochanteric fracture fixation with a dynamic hip screw in relation to pre-operative fracture stability and osteoporosis. Int Orthop. 2001; 25:360–362. PMID: 11820441.

6. Rodop O, Kiral A, Kaplan H, Akmaz I. Primary bipolar hemiprosthesis for unstable intertrochanteric fractures. Int Orthop. 2002; 26:233–237. PMID: 12185526.

7. Kayali C, Agus H, Ozluk S, Sanli C. Treatment for unstable intertrochanteric fractures in elderly patients: internal fixation versus cone hemiarthroplasty. J Orthop Surg (Hong Kong). 2006; 14:240–244. PMID: 17200522.

8. Green S, Moore T, Proano F. Bipolar prosthetic replacement for the management of unstable intertrochanteric hip fractures in the elderly. Clin Orthop Relat Res. 1987; (224):169–177.

9. McGrory BJ, Morrey BF, Cahalan TD, An KN, Cabanela ME. Effect of femoral offset on range of motion and abductor muscle strength after total hip arthroplasty. J Bone Joint Surg Br. 1995; 77:865–869. PMID: 7593096.

10. Bourne RB, Rorabeck CH. Soft tissue balancing: the hip. J Arthroplasty. 2002; 17(4 Suppl 1):17–22. PMID: 12068397.

11. Lee JM, Lee JH, Lee CW, Kim HM. New wiring method for lesser trochanter fixation in unstable intertrochanteric dractures: technical note. J Korean Fract Soc. 2005; 18:209–212.
12. Jin WJ, Dai LY, Cui YM, Zhou Q, Jiang LS, Lu H. Reliability of classification systems for intertrochanteric fractures of the proximal femur in experienced orthopaedic surgeons. Injury. 2005; 36:858–861. PMID: 15949488.

13. Anglen JO, Weinstein JN. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am. 2008; 90:700–707. PMID: 18381305.
14. Aros B, Tosteson AN, Gottlieb DJ, Koval KJ. Is a sliding hip screw or im nail the preferred implant for intertrochanteric fracture fixation? Clin Orthop Relat Res. 2008; 466:2827–2832. PMID: 18465180.

15. Kim SY, Kim YG, Hwang JK. Cementless calcar-replacement hemiarthroplasty compared with intramedullary fixation of unstable intertrochanteric fractures. A prospective, randomized study. J Bone Joint Surg Am. 2005; 87:2186–2192. PMID: 16203881.
16. Lee YK, Ha YC, Chang BK, Kim KC, Kim TY, Koo KH. Cementless bipolar hemiarthroplasty using a hydroxyapatite-coated long stem for osteoporotic unstable intertrochanteric fractures. J Arthroplasty. 2011; 26:626–632. PMID: 20637559.

17. Masonis JL, Bourne RB. Surgical approach, abductor function, and total hip arthroplasty dislocation. Clin Orthop Relat Res. 2002; (405):46–53. PMID: 12461355.

18. Mukka S, Lindqvist J, Peyda S, et al. Dislocation of bipolar hip hemiarthroplasty through a postero-lateral approach for femoral neck fractures: a cohort study. Int Orthop. 2015; 39:1277–1282. PMID: 25557759.

19. Lim YW, Chang YJ, Kwon SY, Kim YS. A simple method using a PACS to minimize leg length discrepancy in primary THA: a method to minimize leg length discrepancy. J Arthroplasty. 2013; 28:1791–1795. PMID: 23540533.
20. Chan KC, Gill GS. Cemented hemiarthroplasties for elderly patients with intertrochanteric fractures. Clin Orthop Relat Res. 2000; (371):206–215.

21. von Roth P, Abdel MP, Harmsen WS, Berry DJ. Cemented bipolar hemiarthroplasty provides definitive treatment for femoral neck fractures at 20 years and beyond. Clin Orthop Relat Res. 2015; 473:3595–3599. PMID: 26186915.

22. Hong CC, Nashi N, Makandura MC, Krishna L. Cemented hemiarthroplasty in traumatic displaced femoral neck fractures and deep vein thrombosis: is there really a link? Singapore Med J. 2016; 57:69–72. PMID: 26892829.

23. Qi X, Zhang Y, Pan J, Ma L, Wang L, Wang J. Effect of bone cement implantation on haemodynamics in elderly patients and preventive measure in cemented hemiarthroplasty. Biomed Res Int. 2015; 2015:568019. PMID: 26413535.

24. Lee JM, Nam HT, Lee SH. Bipolar hemiarthroplasty with cementless femoral stem for unstable intertrochanteric fractures. J Korean Orthop Assoc. 2012; 47:79–85.

25. Lee JM, Jeon JB. Result of a minimum five-year follow-up of hip arthroplasty using the Bencox(R) hip stem. J Korean Orthop Assoc. 2014; 49:126–132.
26. Amstutz HC, Mai LL, Schmidt I. Results of interlocking wire trochanteric reattachment and technique refinements to prevent complications following total hip arthroplasty. Clin Orthop Relat Res. 1984; (183):82–89.

27. Barrack RL, Butler RA. Current status of trochanteric reattachment in complex total hip arthroplasty. Clin Orthop Relat Res. 2005; 441:237–242. PMID: 16331009.

28. Koyama K, Higuchi F, Kubo M, Okawa T, Inoue A. Reattachment of the greater trochanter using the Dall-Miles cable grip system in revision hip arthroplasty. J Orthop Sci. 2001; 6:22–27. PMID: 11289581.

29. Kim WY, Han CH, Ji JH, Kim YY, Lee KS, Lee SW. Fixation for reattachment of trochanteric fragment in pertrochanteric fracture treated with bipolar hemiarthroplasty. J Korean Hip Soc. 2006; 18:67–72.

30. Boardman KP, Bocco F, Charnley J. An evaluation of a method of trochanteric fixation using three wires in the Charnley low friction arthroplasty. Clin Orthop Relat Res. 1978; (132):31–38. PMID: 679549.

Fig. 1
(A) This wiring is performed before insertion of prosthesis components. Each wire is inserted into the superior and inferior aspects of the displaced lesser trochanter and wire knots are placed at the posterior aspect of the bone fragment. (B) Hip prosthesis insertion is conducted after making bone fragments movable with the wires by fixing them using knots anteriorly. (C) After inserting all hip prostheses, lesser trochanteric fragments are reduced using wires and fixed by making knots laterally. (D) A schematic diagram representing the relationship of lesser trochanteric fragments and the iliopsoas, and candy package wiring (named because wiring shape resembles a candy package).
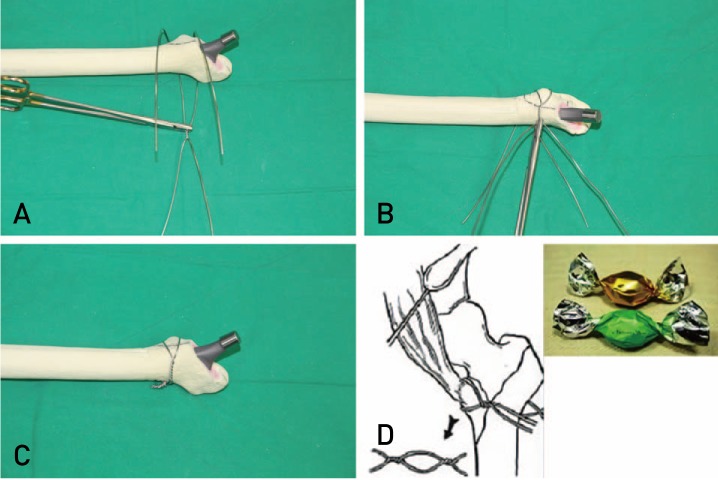
Fig. 2
(A) To enhance rigidity of fixation, a 1.5-mm wire was tied two or three times transversely over the greater trochanter and knots are made laterally. Tying the wire using holes drilled into the anterior portion of greater trochanter can add the additional stability. (B) After making the primary knot, the wire is tightened to the inferior to the lesser trochanter. (C) After tying the wire below the lesser trochanter, the secondary knot is made at the lateral aspect.
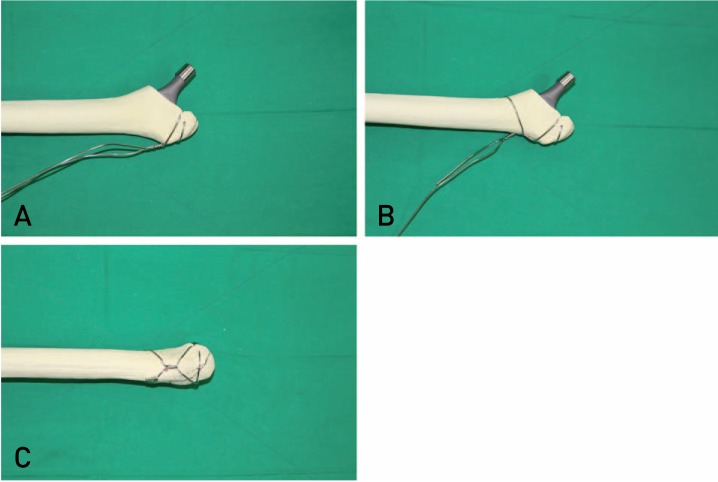
Fig. 3
(A) A double-strand wire is tied to the greater and lesser trochanters using a figure-8 wiring. (B) A wire knot is made rigidly at the lateral aspect. Using this wiring method, fixation can be accomplished by adjusting the position of wires depending on the pattern and location of fracture lines.
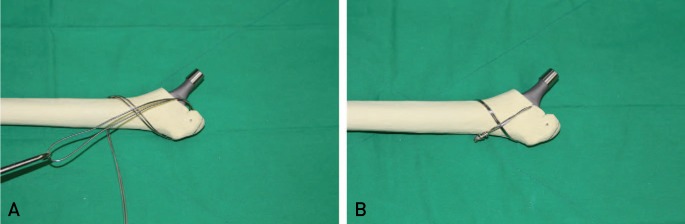
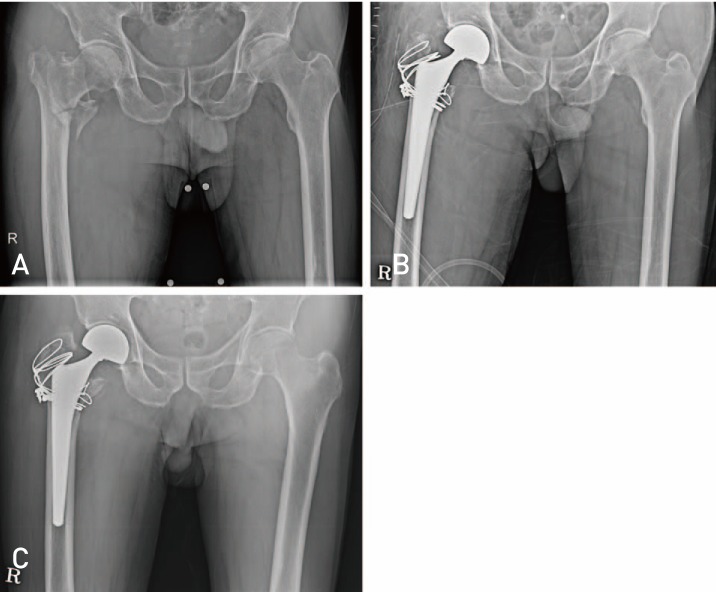
Fig. 4
(A) A 72-year old female patient visited our hospital due to intertrochanteric fracture of left femur after fall down from a height of 1 m. (Preoperative Clawson's Ambulation Capacity: Class 4). (B) Images after performing bipolar hemiarthroplasty and wiring fixation (transverse wiring with distal pulling wire ×2, candy-package wiring). (C) Postoperative 1-year follow-up; no limping gait, restoration of pre-injury ambulatory ability (Clawson's Classification: Class 4) and radiological signs of bone union.
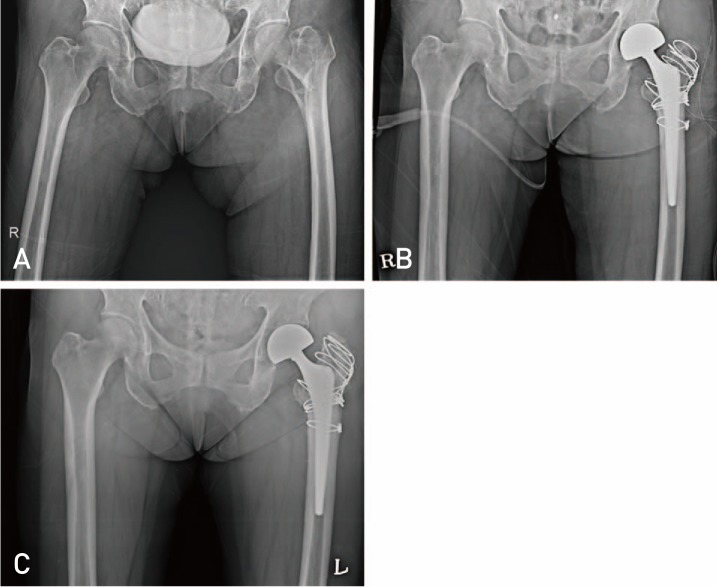
Fig. 5
(A) An 88-year old male patient visited our hospital due to intertrochanteric fracture of right femur after slip down on the way to the toilet. (Preoperative Clawson's Ambulation Capacity: Class 3). (B) Images after performing bipolar hemiarthroplasty and wiring fixation (transverse wiring with distal pulling wire, figure-8 wiring, candy package wiring). (C) Postoperative 1-year follow-up; restoration of pre-injury ambulatory ability (Clawson's Classification: Class 3) and radiological signs of bone union despite slight displacement.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download