Abstract
Purpose
Periprosthetic joint infection (PJI) after total hip arthroplasty (THA) is a grave complication. Urinary tract infection (UTI) as a source for PJI is controversial. Our purposes were, (1) to evaluate the incidence of PJI after elective primary THA and (2) to determine whether UTI was associated with a risk of PJI after elective primary THA.
Materials and Methods
We retrospectively reviewed the medical records of 527 patients who underwent elective primary THA by using universal aseptic technique from May 2003 to October 2007. UTI group (13 patients) was defined as patients who underwent THA in status of having an UTI, and the remaining patients were defined as control group (514 patients). We compared the incidence of PJI in both groups.
Go to : 
Periprosthetic joint infection (PJI) is one of the most serious complications that could arise after total hip arthroplasty (THA)12). Although the incidence of PJI ranges from 0.2% to 1%34567), the PJI is a significant (or major) cause of implant failure and requires multiple operations including revision arthroplasty89). Moreover, the treatment of PJI is very difficult and recurrence is common1011). Therefore, the prevention of PJI is very important in hip arthroplasty.
Microorganism for PJI could be originated not only from exogenous sources such as intraoperative contamination, but also from endogenous or hematogenous sources including remote site skin infection, urinary tract infection (UTI), and pneumonia in patient themselves1213141516).
Among the endogenous sources, UTI has been considered as a possible source for PJI4171819). UTI is generally categorized into upper and lower UTI. Upper UTI, including acute pyelonephritis and intra- /peri-renal abscess, should be treated prior to THA, because the upper UTI can develop to uro-sepsis, and result in impairment of renal function20). However, the lower UTI as a source for PJI still remains controversial413171819). Some authors reported that hip arthroplasty should be delayed until the treatment of UTI, because patients with UTI had a high risk of PJI412171819). But, others demonstrated that preoperative UTI was not associated with PJI1319).
To prevent an occurrence of PJI, surgeons should identify the patients with high risk factors of PJI2122), and correct the modifiable factors prior to THA323). However, unnecessary delays could result in dissatisfaction from patients who wait for THA2425).
Our purposes were (1) to evaluate the incidence of PJI after elective primary THA at a single institute and (2) to determine whether the lower UTI was associated with a risk of PJI after elective primary THA.
Go to : 
After approval of institutional review board, we retrospectively reviewed the medical records of 544 patients (635 hips), who underwent primary THA by two high volume surgeons at a single institute from May 2003 to October 2007. Fifteen patients (15 hips) who were treated for hip fracture and 2 patients who were treated for pathologic fracture were excluded, because they were not elective. The remaining 527 patients (618 hips) were identified for elective primary THA. Among 91 patients who underwent bilateral THA, 25 patients underwent simultaneous bilateral THA, and remaining 66 patients underwent staged bilateral THAs. Simultaneous bilateral THA was considered as a single procedure in this study. Therefore, 527 patients (593 procedures) were analyzed in this study.
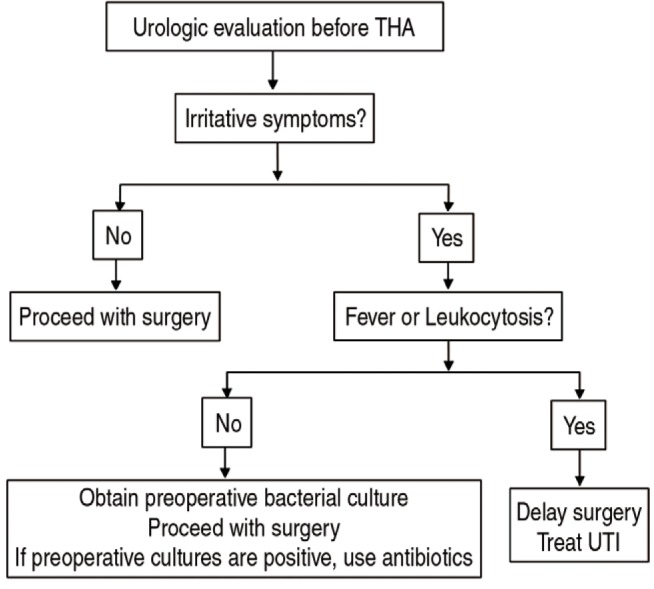
Of the 593 procedures, UTI group was defined as patients who underwent primary THA in status of having an UTI, otherwise, they were defined as control group. During preoperative workups including complete blood count, electrolyte panel and urine analysis, UTI was diagnosed if symptomatic patients have white blood cells greater than 1×104/mL or a bacterial count greater than 1×103/mL14). If a patient was diagnosed with lower UTI, urine culture was performed before THA and prophylactic antibiotics were started at the operation day. It was administered until identification of microorganism. If the patients had fever or leukocytosis, we delayed THA until the control of UTI (Fig. 1).
Thirteen patients (13 procedures) were identified as UTI group. The remaining 514 patients (580 procedures) were classified as control group.
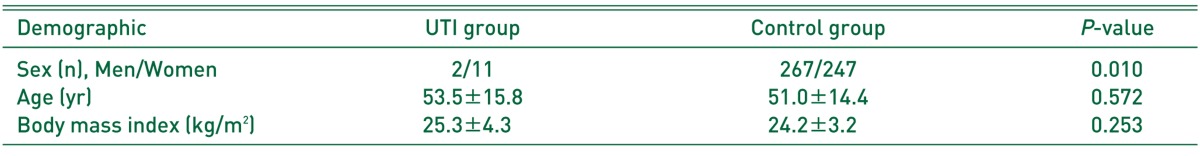
In UTI group, there were 11 females and 2 males with a median age of 57 years (range, 25-74 years). The median of body mass index (BMI) was 26.7 kg/m2 (range, 19.0-33.6 kg/m2). In control group, there were 247 females and 273 males with a mean age of 51.0 years (range, 19-83 years). Their mean BMI was 24.2 kg/m2 (range, 14.6-37.7 kg/m2) (Table 1).
During the study period, the consistent protocols for infection prophylaxis were used. All patients underwent primary THA using standardized universal aseptic technique. We performed all THA in operating rooms equipped with vertical laminar flow with the use of a HEPA filter. Regional anesthesia was used for all operations unless contraindicated. Patients were positioned in lateral position for surgery. Each member of the surgical team put on a cap cover with string (String Hood cap; KM Healthcare Co., Guri, Korea) and a surgical jacket (KM Healthcare Co.) (Fig. 2). Surgical scrub and skin preparation included the use of 2% chlorhexidine-alcohol and aqueous solutions of 10% povidone-iodine (Povidin; Sung Kwang Pharm, Bucheon, Korea). After then, we used an Incise adhesive drape (Ioban™; 3M Corporation, St. Paul, MN, USA).
We routinely used double gloves for all procedures26). We used prophylactic intravenous antibiotics within 1 hour of the THA and for 7 days postoperatively.
We performed THA through a posterolateral approach in 289 procedures, modified anterolateral approach in 260 procedures, and combined approach in 31 procedures. Closed suction drains were used in all cases, and removed at 2 or 3 days postoperatively.
Postoperative wound management included utilization of a sterile dressing that was applied to the incision in the operating room and usually changed at 2 days postoperatively. The wound was evaluated and the sterile gauze was changed twice a week for 1 week to 2 weeks in the ward. During hospitalization, thigh-length antiembolic stockings were applied and the ankle pump was encouraged without any pharmacological thromboprophylaxis. After discharge, patients were routinely followed up on their 6th week, 3rd, 6th, and 12th month and every 1-year thereafter. Patients who had not returned on these regularly scheduled visits were contacted by telephone.
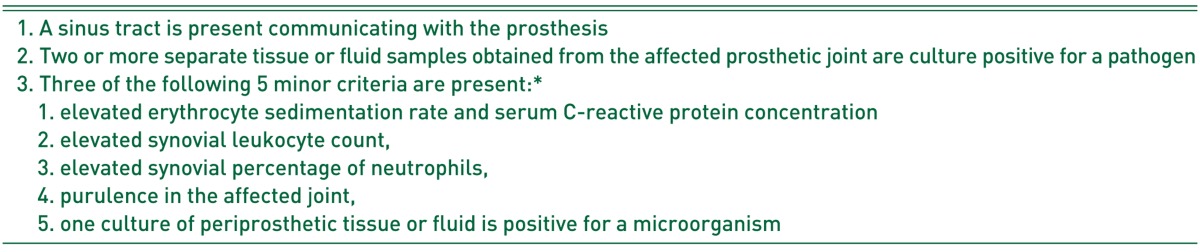
We evaluated the incidence of PJI within 1 year for both groups. The diagnosis of PJI was made by Musculoskeletal Infection Society Criteria, which is gold standard to diagnose PJI (Table 2)27).
We also evaluated Sex, age, BMI, type of anesthesia (regional or general), co-morbidity assessed by American Society of Anesthesiologists (ASA) score, and operation time to determine the relationships between these variables and the development of PJI.
The continuous variables were analyzed by using Mann-Whitney U-test. Chi-square test was used for categorical variables. The SPSS version 16.0 (SPSS Inc., Chicago, IL, USA) was used for the analysis. The statistical significance level was set to 0.05.
Go to : 
Two patients have deceased and 12 patients were lost during follow-up before the minimum 12 months postoperatively. We evaluated 513 patients (579 procedures), who could be followed up at the minimum of 12 months. Among the 579 procedures, overall incidence of PJI was 0% within 1 year postoperatively. The incidence of PJI was 0% in UTI group as well as control group.
Go to : 
We evaluated the overall incidence of PJI and the association of lower UTI and PJI after elective primary THA. The overall incidence of PJI was 0% in our study, regardless of existence of lower UTI.
Many of studies have reported the incidence of PJI ranges from 0.2% to 1%34567). In our series, there was no occurrence of PJI. Universal aseptic technique and well-established facility might be a reason for the absence of PJI in this study. In addition, we did not use routine chemical thromboprophylaxis, which has been considered as a risk of PJI28). Although several studies recommended the use of chemical thromboprophylaxis after THA, we did not do so as venous thromboembolism is uncommon in East Asian patients after THA2930).
Impaired immune status, systematic disease such as rheumatoid arthritis, lupus, diabetes, and malignancy, advanced age, malnutrition, obesity, previous joint infection, longer operation time, and longer preoperative hospitalization have been reported to be associated with a risk of PJI2122). In this study, we could not identify any risk factors because PJI was not encountered.
The presence of remote site infection might be associated with PJI, and we agreed that it should be identified and controlled before surgery, especially in those with fever or leukocytosis. Generally, fever and leukocytosis could be considered as surrogate parameter of systemic bacteremia, which might result in hematogenous PJI20).
This study has several limitations. First, our study was a retrospective study. However, a prospective randomized comparative study is barely possible in this topic, because of ethical issue. Second, the number of patients of UTI group was too small. This means that the power was not enough to determine an association. Third, there might be a selection bias, because our hospital is a referral-only university-hospital with high quality equipment.
Go to : 
Notes
CONFLICT OF INTEREST: The authors declare that there is no potential conflict of interest relevant to this article.
Go to : 
References
1. Springer BD, Fehring TK, Griffin WL, Odum SM, Masonis JL. Why revision total hip arthroplasty fails. Clin Orthop Relat Res. 2009; 467:166–173. PMID: 18975043.

2. Jafari SM, Coyle C, Mortazavi SM, Sharkey PF, Parvizi J. Revision hip arthroplasty: infection is the most common cause of failure. Clin Orthop Relat Res. 2010; 468:2046–2051. PMID: 20195808.

3. Urquhart DM, Hanna FS, Brennan SL, et al. Incidence and risk factors for deep surgical site infection after primary total hip arthroplasty: a systematic review. J Arthroplasty. 2010; 25:1216–1222. 1222.e1–1222.e3. PMID: 19879720.

4. Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res. 2008; 466:1710–1715. PMID: 18421542.

5. Phillips CB, Barrett JA, Losina E, et al. Incidence rates of dislocation, pulmonary embolism, and deep infection during the first six months after elective total hip replacement. J Bone Joint Surg Am. 2003; 85-A:20–26. PMID: 12533567.

6. Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty. 2008; 23:984–991. PMID: 18534466.

7. Blom AW, Taylor AH, Pattison G, Whitehouse S, Bannister GC. Infection after total hip arthroplasty. The Avon experience. J Bone Joint Surg Br. 2003; 85:956–959. PMID: 14516026.
8. Bozic KJ, Ries MD. The impact of infection after total hip arthroplasty on hospital and surgeon resource utilization. J Bone Joint Surg Am. 2005; 87:1746–1751. PMID: 16085614.

9. Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012; 27(8 Suppl):61–65.e1. PMID: 22554729.

10. Fehring TK, Odum SM, Berend KR, et al. Failure of irrigation and débridement for early postoperative periprosthetic infection. Clin Orthop Relat Res. 2013; 471:250–257. PMID: 22552768.

11. Kalra KP, Lin KK, Bozic KJ, Ries MD. Repeat 2-stage revision for recurrent infection of total hip arthroplasty. J Arthroplasty. 2010; 25:880–884. PMID: 20206469.

12. Hamilton WG, McAuley JP. Sepsis: Etiology, prophylaxis, and diagnosis. In : Calaghan JJ, Rosenberg AG, Rubash HE, editors. The adult hip. 2nd ed. Philadelphia: Lippincott Williams & Wilkins;2007. p. 1257–1270. .
13. Koulouvaris P, Sculco P, Finerty E, Sculco T, Sharrock NE. Relationship between perioperative urinary tract infection and deep infection after joint arthroplasty. Clin Orthop Relat Res. 2009; 467:1859–1867. PMID: 19009324.

14. David TS, Vrahas MS. Perioperative lower urinary tract infections and deep sepsis in patients undergoing total joint arthroplasty. J Am Acad Orthop Surg. 2000; 8:66–74. PMID: 10666654.

15. Blomgren G, Lindgren U. Late hematogenous infection in total joint replacement: studies of gentamicin and bone cement in the rabbit. Clin Orthop Relat Res. 1981; (155):244–248. PMID: 7226617.
16. D'Ambrosia RD, Shoji H, Heater R. Secondarily infected total joint replacements by hematogenous spread. J Bone Joint Surg Am. 1976; 58:450–453. PMID: 1270463.
17. Cruess RL, Bickel WS, vonKessler KL. Infections in total hips secondary to a primary source elsewhere. Clin Orthop Relat Res. 1975; (106):99–101.

18. Ainscow DA, Denham RA. The risk of haematogenous infection in total joint replacements. J Bone Joint Surg Br. 1984; 66:580–582. PMID: 6430907.

19. Glynn MK, Sheehan JM. The significance of asymptomatic bacteriuria in patients undergoing hip/knee arthroplasty. Clin Orthop Relat Res. 1984; (185):151–154. PMID: 6705373.

20. Kalra OP, Raizada A. Approach to a patient with urosepsis. J Glob Infect Dis. 2009; 1:57–63. PMID: 20300389.

21. Namba RS, Inacio MC, Paxton EW. Risk factors associated with surgical site infection in 30,491 primary total hip replacements. J Bone Joint Surg Br. 2012; 94:1330–1338. PMID: 23015556.

22. Jämsen E, Nevalainen P, Eskelinen A, Huotari K, Kalliovalkama J, Moilanen T. Obesity, diabetes, and preoperative hyperglycemia as predictors of periprosthetic joint infection: a single-center analysis of 7181 primary hip and knee replacements for osteoarthritis. J Bone Joint Surg Am. 2012; 94:e101. PMID: 22810408.
23. Soohoo NF, Farng E, Lieberman JR, Chambers L, Zingmond DS. Factors that predict short-term complication rates after total hip arthroplasty. Clin Orthop Relat Res. 2010; 468:2363–2371. PMID: 20428982.

24. Roorda LD, Jones CA, Waltz M, et al. Satisfactory cross cultural equivalence of the Dutch WOMAC in patients with hip osteoarthritis waiting for arthroplasty. Ann Rheum Dis. 2004; 63:36–42. PMID: 14672889.

25. Fielden JM, Cumming JM, Horne JG, Devane PA, Slack A, Gallagher LM. Waiting for hip arthroplasty: economic costs and health outcomes. J Arthroplasty. 2005; 20:990–997. PMID: 16376253.
26. Song KH, Kang YM, Sin HY, et al. Outcome of cefazolin prophylaxis for total knee arthroplasty at an institution with high prevalence of methicillin-resistant Staphylococcus aureus infection. Int J Infect Dis. 2011; 15:e867–e870. PMID: 22019197.

27. Parvizi J, Zmistowski B, Berbari EF, et al. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res. 2011; 469:2992–2994. PMID: 21938532.

28. Saleh K, Olson M, Resig S, et al. Predictors of wound infection in hip and knee joint replacement: results from a 20 year surveillance program. J Orthop Res. 2002; 20:506–515. PMID: 12038624.

29. Kang BJ, Lee YK, Kim HJ, Ha YC, Koo KH. Deep venous thrombosis and pulmonary embolism are uncommon in East Asian patients after total hip arthroplasty. Clin Orthop Relat Res. 2011; 469:3423–3428. PMID: 21748508.

30. Kim YH, Kim JS. The 2007 John Charnley Award. Factors leading to low prevalence of DVT and pulmonary embolism after THA: analysis of genetic and prothrombotic factors. Clin Orthop Relat Res. 2007; 465:33–39. PMID: 17693875.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download