Abstract
Purpose
Bipolar hemiarthroplasty (HA) is an option for the treatment of unstable intertrochanteric fracture in elderly patients. There is a raising concern regarding cable-grip related complications for the fixation of trochanteric fragments. Therefore, the aim of this study was to evaluate outcome of cementless HA with fixation for the trochanteric fragments using monofilament wires in unstable intertrochanteric fracture.
Materials and Methods
We reviewed 92 cementless bipolar HAs using a grit-blasted long stem design for unstable intertrochanteric fractures in 91 elderly patients with a mean age of 81.7 years. During the arthroplasty, trochanteric fracture fragments were fixed using 1 or 2 vertical wires and transverse wires. We evaluated the clinical outcomes such as abductor power, ambulatory ability and wire-related complications, and radiologic outcomes including the union of the trochanteric fragment and subsidence of stem.
Results
Sixty-two patients were followed for a minimum of 2 years (mean, 59 months) postoperatively. The mean abductor power and Koval category was 4.1 (range, 3 to 5) and 4.6 (range, 1 to 6). The wire was broken in 3 hips (4.8%) and the nonunion of the greater trochanter occurred in 1 hips (1.6%). Two stems subsided by 3 mm and 8 mm, respectively, during postoperative 6 weeks, after which the subsidence was not progressive.
Treatment of unstable intertrochanteric fracture in osteoporotic elderly patients is challenging, because internal fixation is technically difficult and associated with frequent failure in this type of fracture123). That is why bipolar hemiarthroplasty (HA) has been an option as an alternative treatment for this type of fracture456).
The concern regarding the HA of unstable intertrochanteric fracture is the fixation of comminuted trochanter789). To restore the abductor mechanism, the trochanteric fragment should be fixed. Various fixation techniques have been reported in addition to the technique described by Charnley10). To avoid mechanical failure of monofilament wire, cable grip has been introduced and popularized for the fixation. However, cable-grip related complications appeared as an issue11121314). Silverton et al.11) reported 25% nonunion and 10% osteolysis around the cable of 68 trochanteric osteotomies which were repaired with Dall-Miles cable grip system. Of 51 hips with trochanteric union, fraying or fragmentation of the cable wire was seen in 35%.
Since 2009, we have used cementless stems for the HA of unstable intertrochanteric fractures, and all trochanteric fragments have been fixed with the cerclage method with 16-gauge monofilament wires.
The aim of this study was to evaluate clinical outcomes such as abductor power, ambulatory ability and wire-related complications, and radiologic outcomes including the union of the trochanteric fragment and subsidence of stem after cementless HA using a long stem design in elderly patients who had unstable intertrochanteric fracture.
After approval of Institutional Review Board in Seoul National University Bundang Hospital, we searched a database. From December 2009 to September 2012, 91 elderly (≥ 65 years) patients (92 hips), who were diagnosed as having 31-A2 of AO/OTA classification unstable intertrochanteric fractures, were treated with cementless bipolar HA and cerclage wire fixation of the trochanteric fragments at Seoul National University Bundang Hospital. There were 20 men and 71 women, and their mean age at the time of surgery was 81.7 years (range, 68-95 years). The mean body index was 21.6 kg/m2 (range, 15.2-30.9 kg/m2) and the mean preoperative American Society of Anesthesiologists classification was 2.4 (range, 2-4). The ambulatory ability was informed from patients or their family members and was classified by Koval categories. The mean Koval category before the injury was 2.9 (range, 1-4). The mean duration from admission to operation was 4.6 days (range, 0-23 days), which is the period for the preoperative evaluation and preparation (Table 1). There was a post-hospital surgical delay which is over 2 days from admission to surgery. Post-hospital surgical delay was caused by patient factors such as drug hold (anticoagulants) and the preoperative preparation and by hospital factors such as admission on holiday and delay due to interdepartmental consultation15).
We used a cementless long-stem design (Benfix®; CORENTEC, Cheonan, Korea) in these patients. The design is a straight, double-tapered, rectangular stem, which is made of titanium alloy and has a surface treatment of extensive grit blasting (Fig. 1). The stability of stem was increased by distal fixation using this stem in cases of osteoporotic femur and the comminution of metaphysis.
All operations were performed in a lateral decubitus position through a posterolateral approach by high-volume surgeon. The method of anesthesia was regional in 85 hips and general in the remaining 7 hips. Femoral canal was gradually shaped by rasps, which were used as stem trials to determine the stem size with optimal stability and limb length. We adjusted the leg length with the method described by Lee et al16). We shifted the patient's pelvis to a vertical position, the operated leg was placed on the contra-lateral leg and both heels were placed at the same level. Then, we palpated the level of tibial tuberosity. The optimal stem size and head length were determined by palpating and adjusting the level of the tibial tuberosity of the operated leg to that of the contralateral leg. Once the size was determined, a stem was inserted into the femoral canal with a firm impaction from a gentle tapping to a press fit.
Then, we attached and fixed the greater trochanteric and the medial fracture fragments according to the cerclage fixation method with use of 16-gauge stainless steel wires as described by Harris17). The greater trochanter was fixed with 1 or 2 vertical wires, which was inserted through a hole drilled in the lateral femoral cortex below the abductor tubercle. And each wire was passed through abductor insertion portion anteriorly and posteriorly, which did not compromise adductor muscle power. The medial fragment was fixed with 1 or 2 transverse wires. These wires were tightened and tied with Kirschner wire bows (Fig. 2).
The mean operating time was 93.4 minutes (range, 53-155 minutes). The mean estimated blood loss was 412.5 mL (range, 350-1,000 mL) and 80 patients received a mean of 540 mL (range, 320-1,280 mL) of blood transfusions perioperatively.
Patients were instructed how to stand and walk by our rehabilitation protocols. They were allowed to walk on crutches or a walker with tolerable weight bearing on the second postoperative day. Patients who need further physical therapy were transferred to rehabilitation department or other institutions. As the ambulatory ability improved, the assistive device (walker, crutches, or cane) was changed as determined by a physical therapist. To prevent thromboembolism, patients wore antiembolic stockings and intermittent pneumatic pump was applied in the bed.
Follow-up evaluations were done at six weeks, at 3, 6, 9 and 12 months, and every 6 months thereafter.
The clinical evaluations were done by the Koval categories for walking ability18). At every follow-up, wire related complications corresponding to wire breakage, trochanteric bursitis and trochanteric pain were recorded. At the 2-year follow-up, the abductor power was checked. The power of the abductor was evaluated using Medical Research Council scale19).
The radiologic assessment was performed by two independent orthopedic doctors who did not participate in the operations.
The six-week or three-month radiographs were used as the baseline studies for radiographic comparison. The final radiographic evaluation included an assessment of bony union of the trochanter, wire breakage, osteolysis around the wire, subsidence of the femoral stem20), cortical porosis around the stem21), and heterotopic ossification22).
Our patients were older than 65 years and their mean age was 81.7 years. According to a life chart23), they had a life expectancy of 7.4 years for men and 9.5 years for women. Because of the age characteristics, we included the patients, who had been followed for more than 2 years, in the final analysis.
Descriptive statistics were performed. All analyses were performed using IBM SPSS Statistics, ver. 22.0 (IBM Co., Armonk, NY, USA).
Distal extension of the original fracture occurred intraoperatively in 6 hips (6.5%, 6/92). Five were treated with cerclage wires and the remaining one with a plate fixation. Patients with intraoperative fracture were allowed to walk by a walker with tolerable weight bearing after 4 weeks from operation day (Fig. 3B, C).
Total 16 patients (17 hips) died including 2 patients died during the hospitalization due to problems unrelated with the arthroplasty and 13 patients (13 hips) were lost to follow-up before a minimum follow-up of 2 years. The mean hospital stay was 26.1 days (range, 8-54 days). There was no readmission within 30 days.
The remaining 62 patients (62 hips) were followed for a mean of 59 months (range, 25-79 months).
One hip was dislocated 2 months after the arthroplasty. The dislocation was treated successfully with manual reduction and hip brace for 2 months. Periprosthetic femoral fracture of Vancouver type B1 occurred in one hip of prior intraoperative fracture extension after 3 months postoperatively. The fracture was treated with open reduction and plate fixation (Fig. 3D, E). Otherwise, there was no reoperation or revision.
The wire was broken in three (4.8%) and nonunion of the greater trochanter occurred in 1 hips (1.6%). The nonunion did not affect the abductor power or ambulatory ability. The mean abductor power was 4.1 (range, 3-5) and the mean Koval category was 4.6 (range, 1-6). No patient complained wire-related bursitis such as swelling or trochanteric pain.
A subsidence of stem was observed in two hips at the postoperative 6-week radiographs. Two stems subsided by 3 mm and 8 mm, respectively. However, the subsidence was not progressive (Fig. 4). Although cortical thinning was seen around the stem in 10 hips (16.1%), no stem was loose and there was no osteolysis around the stem or the wire (Fig. 5). Heterotopic ossification was observed in 8 hips (12.9 %); Brooker grade I in 2 hips, grade II in 3 hips, and grade III in 3 hips. Heterotopic ossification did not affect clinical outcome.
Our study presented that the cerclage fixation of the trochanter restored the abductor mechanism and the result of cementless bipolar HA using a grit-blasted long stem design was satisfactory in patients with unstable intertrochanteric fracture. The result of cerclage wiring was compatible with previous results of trochanteric fixation with wiring technique24).
Within the sphere of HA in the unstable intertrochanteric fracture, the trochanteric fragments should be fixed to restore the abductor mechanism. Various techniques have been introduced for the fixation of the trochanter using cerclage wire or cable grip. Meanwhile, few articles were published about wiring technique for bipolar HA. Wiring techniques in previous studies and the present study are summarized in Table 2 7891624). Strength of our technique is to preserve of abductor mechanism, because we did not detach soft tissue from fragment and wires were passed through insertion site of abductor muscle anteriorly and posteriorly. Hence, although nonunion was seen in 1 hip, there was no significant difference in walking ability comparing to union group.
Koval walking ability was decreased from 2.9 to 4.6 in the present study. Although restoration of abductor mechanism by wiring, weakening of walking ability is inevitable in elderly patients. Lee et al.24) reported 53.2% patients demonstrated a decrease of ambulatory capacity in patients treated by HA using various wiring techniques for trochanteric fixation. However, HA for unstable intertrochanteric fracture achieves better result in walking ability than internal fixation because HA facilitates early mobilization25).
The incidence of periprosthetic fracture following cementless HA in large cohort study was 2.5% at 2-year follow-up26). In our study, one periprosthetic fracture (1.6%) occurred during follow-up period. Although it was reported less periprosthetic fracture occurred in cemented stem, we have not been certain for association of periprosthetic fracture and the fixation method because of without control group.
Randomized control trial reported that the incidence of intraoperative fracture (12.1%) in cementless stem was higher than that of cemented stem27). In the case of cementless stem, stem size is determined as big as the width of femoral canal for press-fit. Although expected size is decided by preoperative templating, bigger stem tend to insert due to comminution of proximal femur. Moreover, it is difficult to find anatomical landmark to set the reference point for depth of insertion. Deciding stem size and the depth of insertion is challenging when bipolar HA with cementless stem for unstable intertrochanteric fracture. To protect an intraoperative fracture, transverse wiring before stem insertion is considered. Although we did not perform transverse wiring before stem insertion, intraoperative fracture occurred in 6 hips (6.5%), which is relatively lower than the prior study.
In our study, cortical thinning was observed in 10 hips (16.1%). It could occur after the use of a cementless stem due to an aging phenomenon2829).
We should address several limitations of our study. This was a retrospective study, and we performed a single study without control group. Accordingly, there was no comparison with other stems or fixation method. We also did not examine the thigh pain that is associate with the length of stem30). Meanwhile, although senile patients have a short life expectancy, this study is strengthened by over 2 years of follow-up period in 62 patients (82.7%) except the expired patients within 2 years. Furthermore, novel wiring technique, which vertical wires force opposite to deforming force of greater trochanter, to maintain abductor function is first reported to the best of our knowledge.
This study provides the satisfactory results of an extensively grit blast coated cementless long stem with cerclage wiring. HA using this stem and the fixation method of trochanteric fragments using cerclage wiring by our technique is a safe and satisfactory option to treat unstable intertrochanteric fractures in osteoporotic patients.
Figures and Tables
 | Fig. 1The Benfix stem is a tapered, rectangular extensive grit-blasted titanium stem with a distal slot. |
 | Fig. 2Diagram of cerclage wiring technique. Vertical wires were inserted through a hole below adductor tubercle and then passed through abductor insertion portion anteriorly and posteriorly. For lesser trochanter fragments, transverse wires were passed at the level of lesser trochanter. |
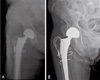
 | Fig. 3(A) An 81-year old woman, who had undergone a hemiarthroplasty for unstable intertrochanteric fracture with Benfix stem and cerclage wires. (B and C) Femoral crack extension occurred intraoperatively, which were treated by cerclage wires. (D) She sustained a periprosthetic fracture at 3 months after a fall from height. (E) On radiograph obtained 3 months after plate fixation. |
 | Fig. 4(A) An 84-year old woman who had undergone a hemiarthroplasty for unstable intertrochanteric fracture with Benfix stem and cerclage wires. (B) On anteroposterior radiographs obtained 6 weeks postoperatively, the stem was subsided about 8 mm. |
 | Fig. 5(A) An 89-year old women who had undergone a hemiarthroplasty for unstable intertrochanteric fracture with Benfix stem and cerclage wires. (B) An anteroposterior radiograph obtained 6 years postoperatively shows cortical stress shielding around the stem. However, there is no loosening sign around the femoral stem. |
References
1. Zhang B, Chiu KY, Wang M. Hip arthroplasty for failed internal fixation of intertrochanteric fractures. J Arthroplasty. 2004; 19:329–333.

2. Hsu CJ, Chou WY, Chiou CP, Chang WN, Wong CY. Hemi-arthroplasty with supplemental fixation of greater trochanter to treat failed hip screws of femoral intertrochanteric fracture. Arch Orthop Trauma Surg. 2008; 128:841–845.

3. Haidukewych GJ, Berry DJ. Hip arthroplasty for salvage of failed treatment of intertrochanteric hip fractures. J Bone Joint Surg Am. 2003; 85-A:899–904.

4. Celiktas M, Togrul E, Kose O. Calcar preservation arthroplasty for unstable intertrochanteric femoral fractures in elderly. Clin Orthop Surg. 2015; 7:436–442.

5. Kayali C, Agus H, Ozluk S, Sanli C. Treatment for unstable intertrochanteric fractures in elderly patients: internal fixation versus cone hemiarthroplasty. J Orthop Surg (Hong Kong). 2006; 14:240–244.

6. Parker MJ, Handoll HH. Replacement arthroplasty versus internal fixation for extracapsular hip fractures. Cochrane Database Syst Rev. 2000; (2):CD000086.
7. Abdelkhalek M, Ali AM, Abdelwahab M. Cemented bipolar hemiarthroplasty with a cerclage cable technique for unstable intertrochanteric hip fractures in elderly patients. Eur J Orthop Surg Traumatol. 2013; 23:443–448.

8. Kim Y, Moon JK, Hwang KT, Choi IY, Kim YH. Cementless bipolar hemiarthroplasty for unstable intertrochanteric fractures in octogenarians. Acta Orthop Traumatol Turc. 2014; 48:424–430.

9. Grimsrud C, Monzon RJ, Richman J, Ries MD. Cemented hip arthroplasty with a novel cerclage cable technique for unstable intertrochanteric hip fractures. J Arthroplasty. 2005; 20:337–343.

10. Charnley J. Total hip replacement by low-friction arthroplasty. Clin Orthop Relat Res. 1970; 72:7–21.

11. Silverton CD, Jacobs JJ, Rosenberg AG, Kull L, Conley A, Galante JO. Complications of a cable grip system. J Arthroplasty. 1996; 11:400–404.

12. Yasgur DJ, Stuchin SA, Adler EM, DiCesare PE. Subtrochanteric femoral shortening osteotomy in total hip arthroplasty for high-riding developmental dislocation of the hip. J Arthroplasty. 1997; 12:880–888.

13. Klinge SA, Vopat BG, Daniels AH, Bariteau JT, Rubin LE, Limbird R. Early catastrophic failure of trochanteric fixation with the Dall-Miles Cable Grip System. J Arthroplasty. 2014; 29:1289–1291.

14. Kim IS, Pansey N, Kansay RK, Yoo JH, Lee HY, Chang JD. Greater trochanteric reattachment using the third-generation cable plate system in revision total hip arthroplasty. J Arthroplasty. 2017; 32:1965–1969.

15. Cha YH, Ha YC, Yoo JI, Min YS, Lee YK, Koo KH. Effect of causes of surgical delay on early and late mortality in patients with proximal hip fracture. Arch Orthop Trauma Surg. 2017; 137:625–630.

16. Lee YK, Ha YC, Chang BK, Kim KC, Kim TY, Koo KH. Cementless bipolar hemiarthroplasty using a hydroxyapatitecoated long stem for osteoporotic unstable intertrochanteric fractures. J Arthroplasty. 2011; 26:626–632.

17. Harris WH. Revision surgery for failed, nonseptic total hip arthroplasty: the femoral side. Clin Orthop Relat Res. 1982; (170):8–20.
18. Koval KJ, Aharonoff GB, Rosenberg AD, Bernstein RL, Zuckerman JD. Functional outcome after hip fracture. Effect of general versus regional anesthesia. Clin Orthop Relat Res. 1998; (348):37–41.
19. Compston A. Aids to the investigation of peripheral nerve injuries. Medical Research Council: Nerve Injuries Research Committee. His Majesty's Stationery Office: 1942; pp. 48 (iii) and 74 figures and 7 diagrams; with aids to the examination of the peripheral nervous system. By Michael O'Brien for the Guarantors of Brain. Saunders Elsevier: 2010; pp. [8] 64 and 94 Figures. Brain. 2010; 133:2838–2844.

20. Meijerink HJ, Gardeniers JW, Buma P, Lemmens JA, Schreurs BW. Hydroxyapatite does not improve the outcome of a bipolar hemiarthroplasty. Clin Orthop Relat Res. 2004; (421):143–150.

21. Capello WN, D'Antonio JA, Geesink RG, Feinberg JR, Naughton M. Late remodeling around a proximally HAcoated tapered titanium femoral component. Clin Orthop Relat Res. 2009; 467:155–165.

22. Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973; 55:1629–1632.
23. Korea National Statistical Office. Abridged Life Tables[Internet]. Daejeon: Korean Statistical Information Service;2014. updated 2016 Dec 02. cited 2017 Mar 1. Available from: http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B41&conn_path=I2/:2014.
24. Lee JM, Cho Y, Kim J, Kim DW. Wiring techniques for the fixation of trochanteric fragments during bipolar hemiarthroplasty for femoral intertrochanteric fracture: clinical study and technical note. Hip Pelvis. 2017; 29:44–53.

25. Yoo JI, Ha YC, Lim JY, Kang H, Yoon BH, Kim H. Early rehabilitation in elderly after arthroplasty versus internal fixation for unstable intertrochanteric fractures of femur: systematic review and meta-analysis. J Korean Med Sci. 2017; 32:858–867.

26. Grosso MJ, Danoff JR, Murtaugh TS, Trofa DP, Sawires AN, Macaulay WB. Hemiarthroplasty for displaced femoral neck fractures in the elderly has a low conversion rate. J Arthroplasty. 2017; 32:150–154.

27. Inngul C, Blomfeldt R, Ponzer S, Enocson A. Cemented versus uncemented arthroplasty in patients with a displaced fracture of the femoral neck: a randomised controlled trial. Bone Joint J. 2015; 97-B:1475–1480.
28. McCalden RW, McGeough JA, Barker MB, Court-Brown CM. Age-related changes in the tensile properties of cortical bone. The relative importance of changes in porosity, mineralization, and microstructure. J Bone Joint Surg Am. 1993; 75:1193–1205.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download