Abstract
Purpose
The aim of this study was to assess the mid-term results of primary cementless total hip arthroplasty (THA) using Summit® stems.
Materials and Methods
One hundred twenty-eight arthroplasties in 121 patients who were performed THA from December 2004 to March 2013, were reviewed retrospectively a minimum of 4 years follow-up (mean age, 60.3 years; mean postoperative follow up period, 86.3 months). For a clinical evaluation, the Harris hip score (HHS) was used to assess outcome. Radiographic evaluation was done through spot welds, subsidence, stress shielding, canal filling.
Results
The mean HHS was 69.8 points preoperatively, and it improved significantly to 96.3 points at the final follow-up. Postoperatively, 10 patients experienced thigh pain and 7 patients showed a moderate limping gait. There was not only early stem subsidence but there was no more subsidence at last follow up. One hundred eighteen hips showed radiographic signs of stem bone ingrowth, and 10 hips showed fibrous ingrowth at the last follow-up. Stress shielding occurred in 85 hips and third degree stress shielding was observed in 6 hips. Complication arose in 10 hips due to dislocation. Although revisions due to recurrent dislocations led to acetabular component revision in one hip, no revisions arose due to isolated aseptic loosening of the femoral component.
Conclusion
The clinical and radiological mid-term results of primary THA using Summit® stems revealed solid initial fixation and bone ingrowth stable fixation. Considering the satisfactory clinical results, Summit® stems may be a good treatment option in Korean patients who were required hip arthroplasty
Total hip arthroplasty (THA) remains one of the most successful operations for pain relief, functional improvement, or overall patient satisfaction1). Because of this reason, Thus, therefore, is due to, result from different kinds of stem were used and different researches following the way of treating surface and the design of the stem were proceeded. The Summit® stems (DePuy Synthes Co., Warsaw, IN, USA.) have been clinically utilized for THA since 2001. The Summit® stems are collarless third generation tapered titanium stems, for which the upper third is POROCOAT® porous coated (DePuy Synthes Co.), the mid-portion is grit blasted, and the distal tip has a polished shine. Such a surface treatment on the stem can improve bony ingrowth and enable strong fixation. Futhermore, ZTT (zeta tau textured) steps provide solid axial and rotational stability, because the radial ZTT steps in the upper stem converts shear hoop stresses to compression loads2).
A previously-reported study in Korean demonstrated that significant difference is observed between combined anteversion and theoretical combined anteversion among Asians3). This anatomical difference in Asians may somehow arouse an inherent deviation on outcome and results compared to former studies carried out in Caucasians. Therefore, the purpose of this study was to investigate Asians outcome, in particular that of Koreans. A retrospective investigation was conducted for a group of Korean patients who had undergone a THA using the Summit® stems at our hospital. This study was to assess the mid-term results of primary cementless THA using Summit® stems (standard off set) for Korean patients with a hip disease, who had been followed for a minimum of 4 years.
We retrospectively studied 121 patients, analyzing 128 hips, who had received primary cementless THA using the Summit® stem (standard off set) from December 2004 to March 2013. Patients were followed for more than 4 years on an outpatient basis. This study was approved by the hospital ethical review board (IRB approval no. 2017-09-014).
The patient average age was 60.3 years (range, 31-97 years) and the cohort comprised 29 males, 31 hips (24.2%) and 92 females, 97 hips (75.8%). The mean height was 153.1 cm (range, 140-181 cm) and the mean body mass index was 23.1 kg/m2 (range, 15.4-34.2 kg/m2). The mean postoperative follow up period was 86.3 months (range, 48-137 months). The demographic data of the patients who receives a Summit® stem are listed in Table 1. The preoperative diagnoses included post-traumatic arthritis for 10 hips, avascular necrosis of the femoral head for 29 hips, a femoral neck fracture for 51 hips, and degenerative arthritis for 38 hips. The Dorr Classification of the bone type was A for 70 hips (54.7%), B for 54 hips (42.2%), and C for 4 hips (3.1%) (Table 1)4). All of the operations were performed by a senior surgeon and a posterolateral approach was used in all hips. A hemispherical, uncemented acetabular component (Pinnacle; DePuy Synthes Co.) was utilized as an acetabular component. Each implant size is shown in Table 2. Postoperatively, partial weight-bearing was allowed after hemovac was removed (at a mean postoperative of 3.1 days) for the first 6 weeks, then progressively increased loading to full weight-bearing over the next 6 weeks. At the final follow-up, patients were assessed clinically with the Harris hip scores (HHSs). Postoperative pain, range of motion, and function were reconstructed retrospectively by interview and patient charts.
For a clinical evaluation, using HHS, as well as interpret complications during and after surgery in all patients5). Radiographic evaluation was done through comparison between immediate postoperative radiographs and last follow-up radiographs. To evaluate femoral and acetabular components, we assessed all using published criteria6). The stability of the femoral components was assessed according to the criteria of Engh's classification for biologic fixation of bone ingrowth, stable fibrous fixation, and unstable fixation7). The canal filling of the stem seen on the anteroposterior radiograph was measured at the following levels: the upper border of the lesser trochanter, 1 cm below the lesser trochanter, and 1 cm proximal to the tip of the prosthesis89). Subsidence was measured using a perpendicular line drawn from the greater trochanter to the lateral border of the implant, as well as from the collar to the lesser trochanter as a reference. A difference of 3 mm in both measurements is considered significant10). Location of bone reaction around the femoral components including radiolucent lines, osteolysis, cortical hypertrophy, presence/absence of spot welds were rated according to the Gruen criteria1112). Stress shielding was classified as grade I when only resorption of the medial edge of the resection line appeared. Grade II meant additional proximal medial bone resorption, while grade III findings extended more distally. Thigh pain (8.3%) and cortical hypertrophy (92.2%) were detected in the Summit® stem, and that wound would be caused by surface treatment methods of the femoral stem, and morphological differences.
The stem survival rate was analyzed using the Kaplan Meier method. The end point was the time of revision for any reason. Preoperative and postoperative HHSs were compared using a two-sample t-test. A P-value <0.05 was considered statistically significant for all differences.
The mean HHS was 69.8 points (range, 58-97 points) preoperatively, and it improved significantly to 96.3 points (range, 82-100 points) at the final follow-up. Postoperatively, 10 patients (8.3%) experienced thigh pain, and 7 patients (5.8%) felt a moderate limping gait. There was no early stem subsidence and no more subsidence in any patient after postoperative 6 weeks. Of the 128 hips, 118 hips (92.2%) showed radiographic signs of stem bone ingrowth including Gruen zone 3 and 5, and 10 hips (7.8%) showed thin lucent zones along the bone-metal interface due to fibrous ingrowth at the last follow-up, while none was considered to be loose. Cortical hypertrophies (92.2%) were detected in the final follow up radiographs (Fig. 1).
None of patients in this study showed unstable stem fixation. Partial resorption of the calcar femoris with signs of stress shielding rated grade I was observed in 51 hips (39.8%). Bone resorption in the proximal portion of the femur (Gruen zones 1 and 7), which was regarded as Grade II Stress shielding occurred in 28 hips (21.9%). Third degree stress shielding which bone resorption extended distally was observed in 6 hips (4.7%). Complications were noted in 8 hips (6.3%) which had calcar crack sustained during stem insertion. There were required circumferential wirings. However, these intraoperative cracks were healed without migration of the stems and other additional problems. Further, 10 hips (7.8%) had dislocated. The relatively high rate of dislocation of hip joint of 7.8% of this research might be due to its only use of posterolateral approach by one medical team. After report from instructional course lectures, the rate of dislocation of hip joint might start from 0.2% and arise up to 9.5% when posterolateraly approached.
Although revision because of recurrent dislocation led to acetabular component revision in one hip (0.8%), there were no revisions because of isolated aseptic loosening of the femoral component. The Kaplan-Meier survival analysis showed a survival rate of 99.1% at 4 years, with failure defined as revision for any reason (Table 3).
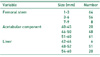
As Summit® stem is tapered and collarless, it can wedge into the femoral canal making an arrangement that provides sufficient rotational stability to ensure bone ingrowth fixation. Also, the circumferential porous coating area extends up to zone 6 of the Summit® stem and ZTT steps of the proximal coated portion enables a strong fixation. Requirements for stable fixation of the porous coating implants have been studied extensively and many principles are well accepted. Initial stability of the implant is critical to minimize the micro-motion and to allow bone ingrowth. The porous surface must be biocompatible, resist abrasion and corrosion, and form a strong bond with the implant substrate. Cementless implants have shown a high success rate in primary THA and relatively fine outcomes on long-term follow-up. In comparison of the two implant types, superiority has yet to be determined, however, a choice made based on the objective of the surgery, the function of the joint, the quality of the bone, and the surgeon's experience will result in a good outcome. Till now, many studies of patient groups in Europe and the U.S. reported postoperative results of THA using the Summit® stems., whereas studies of Korean patients have been rather scarce1314). Nevertheless, a previouslyreported study in Korean demonstrated that significant difference is observed between combined anteversion and theoretical combined anteversion among Asians3). The average measurement of anteversion of the acetabular cup was 15.9±2.9° and anteversion of the femoral stem was 15.2±11.9°. Then, the combined anteversion was calculated to 24.0±8.2°. This anatomical difference in Asians may somehow arouse an inherent deviation on outcome and results compared to former studies carried out in Caucasians. Therefore, this study focused on Asians outcome, in particular that of Koreans. Yang et al.13) have also published papers previously about Summit® stem. Though, the subject patients were 31 and 36 respectively, relatively small patient groups, but our paper has performed an analysis on 121 patients thus having merits over former papers. Titanium is 50% less stiff than chromium-cobalt, thereby increasing the proximal transfer of stress. In experimental studies and in studies on canine models, titanium stems produced much less bone resorption than equivalent chromium-cobalt stems, lately verified histologically and with dual-energy X-ray absorptiometry scans. Limiting the extent of porous coating has also been shown to be a factor in the reduction of stress shielding. However, the most challenging issue is the stress shielding effect that can manifest in the proximal fit stem. Nishino et al.5) found that even with proximally fixed type stems, severe stress shielding occurred because of distal fixation. Engh et al.15) reported that stress shielding itself does not strongly affect the long-term results of THA, while Noble et al.16) found that the range and degree of stress shielding augmented during the postoperative course. Other reports found no case of severe stress shielding using the Summit® stems in American and European patients41317). Conversely, third degree stress shielding occurred in 15% of Japanese patients with hip diseases. In order to compare and verify postoperative stress shielding and spot welds, we drew comparisons between radiographs taken 2 weeks and 4 years after surgery. Based on this current study, third degree stress shielding was observed in 6 hips (4.7%) (Fig. 2). It shows a low rate similar to the result of studies brought on American and European patients. Controversial cause by stress shielding in THA using Summit® stems is therefore unnecessary, whereas severe stress shielding can lead to a high risk of fracture and careful follow-up may be mandatory. In this study, stem subsidence was not detected during the follow-up period of a minimum of 4 years. Moreover, spot welds were observed in 104 hips (81.3%) (Fig. 3). The rate of spot welds was higher than that reported by others using proximally fixed, Synergy® cementless tapered stem (35%; Smith &Nephew, Inc., Memphis, IN, USA)18). In this recent study, 8 hips (6.3%) required circumferential wiring due to a calcar crack sustained during stem insertion. There were 8 intraoperative cracks; 7 and 1 occurred in Dorr types B and C femurs versus none in Dorr type A femurs. All calcar cracks had occurred in the early learning period. However, these intraoperative cracks were healed without migration of the stems and other additional problems. THA using Summit® stems, which is composed of collarless tapered titanium stems and POROCOAT® porous coating showed excellent mid-term results in the present study.
In this study, the ratio of postoperative dislocation of Korean was high. Since most of dislocation happened within 3 months after operation, it is important for patients to adapt to preventive education. The patients have to be trained to avoid excessive flexion, adduction, internal rotation after operation. It is necessary to give a guideline through the picture of sitting posture in their daily life. The risk of dislocation is influenced by the position of the components, the surgical approach, the surgical techniques, the design of the prosthesis, the underlying diagnosis and the patient's compliance with restrictions. In particular, sedentary lifestyles in Koreans may have affected the result. This study's object was Koreans, nevertheless of its nonsufficient sample size, further analysis and studies with bigger sample size for Koreans and their lifestyles should be investigated.
This study has limitations in that 1) the sample sizes of included cases are relatively small to make proper assessment of the validity of the Summit® stems, and that 2) the necessary long-term outcomes, such as fractures secondary to stress shielding, are not available.
Through this investigation, the results of a solid initial fixation of Summit® stems are attained from Korean patients. Considering the satisfactory clinical results, Summit® stems may be a good treatment option in Korean patients who were required hip arthroplasty. The future studies with larger sample sizes and careful long-term follow-up are necessary in order to validate our findings.
Figures and Tables
References
1. Burnett RSJ. Total hip arthroplasty: Techniques and results. B C Med J. 2010; 52:455–464.
2. Engh CA, Massin P. Cementless total hip arthroplasty using the anatomic medullary locking stem. Results using a survivorship analysis. Clin Orthop Relat Res. 1989; (249):141–158.
3. Oh KJ, Lee JG. Usefulness of a modular hip system for combined anteversion in cementless total hip arthroplasty. Hip Pelvis. 2013; 25:30–36.

4. Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993; 14:231–242.

5. Nishino T, Mishima H, Miyakawa S, Kawamura H, Ochiai N. Midterm results of the Synergy cementless tapered stem: stress shielding and bone quality. J Orthop Sci. 2008; 13:498–503.

6. Callaghan JJ, Salvati EA, Pellicci PM, Wilson PD Jr, Ranawat CS. Results of revision for mechanical failure after cemented total hip replacement, 1979 to 1982. A two to five-year followup. J Bone Joint Surg Am. 1985; 67:1074–1085.

7. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51:737–755.

8. Sakai T, Sugano N, Nishii T, Haraguchi K, Ochi T, Ohzono K. Stem length and canal filling in uncemented custom-made total hip arthroplasty. Int Orthop. 1999; 23:219–223.

9. Kim YH, Kim VE. Uncemented porous-coated anatomic total hip replacement. Results at six years in a consecutive series. J Bone Joint Surg Br. 1993; 75:6–13.

10. Mulliken BD, Bourne RB, Rorabeck CH, Nayak N. A tapered titanium femoral stem inserted without cement in a total hip arthroplasty. Radiographic evaluation and stability. J Bone Joint Surg Am. 1996; 78:1214–1225.

11. Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; (141):17–27.
12. Engh CA, Glassman AH, Suthers KE. The case for porous-coated hip implants. The femoral side. Clin Orthop Relat Res. 1990; (261):63–81.
13. Yang IH, Park SH, Han CD. Cementless total hip arthroplasty using ceramic-on-ceramic summit(R) system: 3 years follow up. J Korean Hip Soc. 2007; 19:9–15.

14. Lim YW, Lee KH, Bae SH, Kwon SY. Comparative analysis of two cementless stems in total hip arthroplasties in patients with osteonecrosis of femoral head: summit(R) stem and bencox(R) stem. J Korean Hip Soc. 2012; 24:25–31.

15. Engh CA, Bobyn JD. The influence of stem size and extent of porous coating on femoral bone resorption after primary cementless hip arthroplasty. Clin Orthop Relat Res. 1988; (231):7–28.

16. Noble PC, Alexander JW, Lindahl LJ, Yew DT, Granberry WM, Tullos HS. The anatomic basis of femoral component design. Clin Orthop Relat Res. 1988; (235):148–165.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download