Abstract
Purpose
We evaluated long-term clinical and radiographic results in patients underwent primary total hip arthroplasty (THA) using 36-mm metallic femoral head and 1st generation highly cross-linked polyethylene among patients aged 40 years and less, with minimum 10 years follow-up.
Materials and Methods
We retrospectively reviewed 20 hips underwent primary THA by one hip surgeon using 36-mm femoral head and 1st generation highly cross-linked polyethylene from 2004 to 2006. Mean follow up was 131.55 months. Clinical follow-ups included functional measurements. And we evaluated post operative complications, prosthesis loosening, failure, and osteolysis. For radiologic evaluations, together with position of acetabular cup at 6 weeks later of postoperation, we separately calculated the penentrations of femoral heads into polyethylene liners during postoperation and one year later check-ups, and during one year later check-ups and final check-ups. Polywear pro3D 5.10 software was used to measure penetrations of femoral head.
Results
Mean acetabular cup inclination and anteversion were 49.02° and 10.19°, respectively. Mean thickness of the polyethylene liner at 45° was 6.44 mm. There were no major complications such as implant loosening or osteolysis, and one case of dislocation occurred. Average modified Harris hip score at final follow-up was 91, and Merle d'Aubigne and Postel scores 15 were or over. Average femoral head penetration of bedding wear was 0.170±0.039 mm/year. Steady-state wear rates was 0.059±0.006 mm/year.
Nowadays, several materials such as metal-on-polethylene liners, ceramic-on-polyethylene liners, metal-on-metal bearings, and ceramic-on ceramic, are being used as bearing surfaces of total hip arthoplasty. Among all the materials, metal-on-polyethylene liners have been successfully used as bearing surfaces for several decades. However, wear of the polyethylene over time, and the resulting complications such as osteolysis, aseptic loosening have been issued in long-term follow-up studies1). Even though the use of large head have the benefit of stability, it had avoided the fear of higher wear rates, avoidance of the use of larger femoral heads have had influence on the stability of the hip. However, after the introduction of highly cross-linked polyethylene (HXLPE), which shows lower wear rates compared to conventional polyethylen liners, large-sized femoral heads have been available for use in total hip arthroplasty, with expectance of higher hip joint stability23). Through several comparative studies, have reported results of lower wear rates and higher joint stability, with higher levels of satisfaction among patients, using 36 mm diameter femoral heads with 1st generation HXLPE456). However, many studies have still reported large diameter femoral heads to induce wear and mechanical destruction of polyethylene liners, and thus to be more beneficial to the aged patients. Studies on the use of 36 mm diameter femoral heads with 1st generation HXLPE in Korean patients younger than 40 years old, have not been reported. For this reason, we are to report the long term results (minimum 10 years) of the combination of 36 mm diameter femoral heads with 1st generation HXLPE, in patients younger than 40 years of healthy.
Patients under 40 years of age who visited our medical center from 2004 to 2006 and underwent total hip arthroplasty using 36 mm diameter femoral heads and 1st generation HXLPE were enrolled to this study. During this periods, we performed 29 cases of total hip arthroplasty for Patients under 40 years. Two cases operated with 28-mm metal head, and 7 cases were not met of minimum 10-year follow ups. Retrospective analysis included 20 cases from 17 patients (Table 1). The study received the approval by the institutional review board at the author's institution (CR-17-132).
Causes for surgery included 5 cases of rheumatoid arthritis, 5 cases of dysplastic hip, 3 cases of ankylosing spondylitis, 3 cases of avascular necrosis of the femoral head, 2 cases of osteoarthritis, 1 case of pathological fracture of the femoral neck, and 1 case of slipped capital femoral epiphysis (Table 2). Mean age at the time of surgery was 36.2 years (21 to 40 years), and the mean follow-up period was 131.55 months (120 to 162 months). Porous-coated cementless acetabular cups (Trilolgy® Zimmer Inc., Warsaw, IN, USA) and HXLPE acetabular liners (Longevity® Zimmer Inc.) were used for surgery. The Longevity® polyethylene liners were manufactured from GUR 1050 polyethylene (Zimmer Inc.) with compressive-molded techniques. The liners were launched after 9.5 Mrad electron beam irradiation processing for increased cross-linking and strength, remelting processing of the irradiated plastic in order to eliminate the remaining free radicals which may cause oxidation, and aseptic processing using gas plasma technology.
Acetabular components had a mean outer diameter of 54 mm (range, 50–60 mm). Fiber metal stem (Zimmer Inc.) components were used in 14 cases underwent cementless femoral fixation and Heritage Versys (Zimmer Inc.) components in 6 cases underwent cemented femoral fixation. All cementless stems were inserted using standard press fit techniques to insure longitudinal and rotational stability, and all cemented femoral stems were inserted using meticulous third generation cementing techniques. All surgical procedures were performed by one surgeon using a modified Harding's approach with the patient in the lateral position. Prophylactic antibiotics were administrated to all patients within 1 hour from incision. Patients were allowed to sit on the first postoperative day and stand with support, according to ability, after blood drainage removal. There was no range of motion limitation immediately after surgery, and no abduction pillow was used in any patient. Patients were followed at 6 weeks, and at 3, 6, and 12 months postoperatively. After then, we asked patients to visit every 1 year. The clinical radiographic examinations were asked to another orthopedic surgeon. Clinical follow-ups included specific assessments of possible dislocation. In addition, modified Harris hip scores (HHS) and Merle d'Aubigne and Postel score were evaluated. All radiographic examinations included an anteroposterior (AP) view of the pelvis centered over the pubis, and axial view by a shoot through lateral of the hip. In cases that underwent uncemented fixation, the status of fixation of femoral component was assessed using Engh et al.'s method7), and in cases that underwent cemented fixation, femoral components were assessed the amount of cement filling using Barrack et al.'s method8) using immediate postoperative radiographs. Acetabular cup abduction angles were measured using Engh et al.7) and Kennedy et al.'s methods. Acetabular cup anteversion angles and the wear were measured using polyWare pro 3D distal version 5.10 software (Drafware Developers Inc., Vevay, IN, USA).
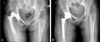
Average modified HHS at final follow-up was 91 (86–95), and it was better than ‘good’ in all cases, and Merle d'Aubigne and Postel scores were more than 15 (15–18) in all cases (Table 3). Radiographic final follow-up exams showed fibrous or bony ingrowth stable fixation in all patients with uncemented femoral components, and Barrack type A or B in all patients with cemented femoral components. Mean acetabular cup abduction and anteversion were 49.02° (42.9°–56.7°) and 10.19° (7.2°–15.0°), respectively. Mean thickness of the polyethylene liner at 45° was 6.44 mm (minimum 5.8 mm). There was no radiographic evidence of osteolysis in the pelvis or proximal femur, and no acetabular cup or femoral stem failing due to aseptic loosening. But, one patient developed a hip dislocation. She sustained car accident and had a injury of femoral head posterior dislocation with acetabular fracture. After acetabular fracture fixation, she underwent total hip arthroplasty due to secondary hip osteoarthritis. After 1 year of operation, she had a dislocation (Fig. 1). In this patient, anteversion of the index cup was 8°. The patient underwent isolated acetabular revision just after second dislocation, and has done routine indoor activity well since then. In all patients, average femoral head penetration during the first postoperative year (predominantly representing polyethylene creep) was 0.170±0.039 mm/year, and the average steady-state wear rate determined using radiographs taken at 1-year postoperatively and at latest follow-up was 0.059±0.006 mm/year.
When considering primary total hip arthroplasty for young patients, two points-that the patient has a long period to on, and that the patient has a high level of activity-should be took into account. In general, younger patients will have higher wear rates than the aged, and may affect the life span of the implants. Continuous development the surface design and implant materials have made the dent in complications due to polyethylene wear. For young and active patients, ceramic-on-ceramic bearing surface materials have shown wear rates lower than 0.001 mm/year in vitro studies, and have been proven to be superior in wear rates9) in vivo studies. However, the problems of squeaking sounds on friction, and fractures of the ceramic head and ceramic liners were still remained10). According an in vitro study, the development of 1st generation HXLPE reduced the wear rates from 74% to 58%, compared to conventional polyethylene liners. Notwithstanding the long- and midterm results of in vivo studies, which showed superior results with low wear rates11), surgical outcomes in young patients have stiil been controversial. During the electron beam irradiation processing and the remelting processing in order to eliminate the remaining free radicals, the decrease in tensile yield strength and fatigue stress raise concern over the polyethylene breakage. The fact that the risk of such breakage is higher in young, active patients has been a major cause for controversy12).
In our study, the long-term results of the wear rates in young, active patients were 0.059±0.006 mm/year in average, and there were no cases of polyethylene fractures. Our cases showed more wear rates compared other studies1314). But, this result was below the threshold of 0.1 mm/year of conventional polyethelene12). One case of hip joint dislocation occurred during the follow-up period, in a patient who underwent total hip arthroplasty due to secondary osteoarthritis after internal fixation for posttraumatic acetabular fracture and posterior dislocation of the hip joint. The dislocation occurred a year after surgery, and the acetabular anteversion was 8°. Though the use of 36 mm diameter femoral head may increase the stability of the hip joint, such case could be an explanation for the importance of precise implant insertion during surgery. Trunnion corrosion, due to increased load to the trunnion, usually occurs in femoral heads with diameter over 40 mm. In terms of hip joint stability, the increase in joint stability with the diameter increase from 40 to 46 mm is not greater compared to the increase in joint stability with diameter increment from 36 to 40 mm, which makes the 40 mm diameter femoral head of less use. In case of 36-mm femoral heads, trunnion corrosion might not be a major problem. Also, trunnion corrosion tends to be more frequent in ceramic-on-ceramic bearing surfaces, rather than metal-on-polyethylene bearing surfaces.
Our study possesses several limitations. Firstly, this study was retrospective and had no control group. Secondly, this retrospective study was limited by small size. Additional studies with a large sample size are warranted. Thirdly, we did not measure the volumetric wear rate. Though we were able to evaluate the volumetric wear by analyzing the plain AP and axial radiographs of the pelvis with the use of the PolyWare 3D software, the measured values in axial radiographs were unreliable due to its irregular results. For this reason, we only evaluated the linear wear rates by analyzing only the AP films. Fourthly, due to the small size of the cohort, the prevalence of inflammatory diseases among the cohort was very high. Eight of 20 cases suffered from inflammatory diseases such as rheumatoid arthritis and anklyosing spondylitis. Since patients with inflammatory diseases tend to have lower level of activity, the high prevalence of inflammatory diseases might lead to measurement error15).
Figures and Tables
References
1. Schmalzried TP, Jasty M, Harris WH. Periprosthetic bone loss in total hip arthroplasty. Polyethylene wear debris and the concept of the effective joint space. J Bone Joint Surg Am. 1992; 74:849–863.

2. Bistolfi A, Crova M, Rosso F, Titolo P, Ventura S, Massazza G. Dislocation rate after hip arthroplasty within the first postoperative year: 36 mm versus 28 mm femoral heads. Hip Int. 2011; 21:559–564.

3. Geller JA, Malchau H, Bragdon C, Greene M, Harris WH, Freiberg AA. Large diameter femoral heads on highly cross-linked polyethylene: minimum 3-year results. Clin Orthop Relat Res. 2006; 447:53–59.
4. Choi WK, Cho MR, Lee JH. Results of primary total hip arthroplasty with 36-mm femoral heads on highly cross-linked polyethylene-minimum seven-years follow-up. Hip Pelvis. 2014; 26:220–226.

5. Choi WK, Cho MR, Kim HS, Nam JH, Chae SB. Results of primary total hip arthroplasty using 36 mm femoral heads on 1st generation highly cross linked polyethylene in patients 50 years and less with minimum five year follow-up. Hip Pelvis. 2016; 28:76–81.

6. Cho MR, Lee HS, Lee SW, Choi CH, Kim SK, Ko SB. Results after total hip arthroplasty with a large head and bipolar arthroplasty in patients with displaced femoral neck fractures. J Arthroplasty. 2011; 26:893–896.

7. Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987; 69:45–55.

8. Barrack RL, Mulroy RD Jr, Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review. J Bone Joint Surg Br. 1992; 74:385–389.

10. Jarrett CA, Ranawat AS, Bruzzone M, Blum YC, Rodriguez JA, Ranawat CS. The squeaking hip: a phenomenon of ceramic-on-ceramic total hip arthroplasty. J Bone Joint Surg Am. 2009; 91:1344–1349.

11. Lee JH, Lee BW, Lee BJ, Kim SY. Midterm results of primary total hip arthroplasty using highly cross-linked polyethylene: minimum 7-year follow-up study. J Arthroplasty. 2011; 26:1014–1019.

12. Dumbleton JH, Manley MT, Edidin AA. A literature review of the association between wear rate and osteolysis in total hip arthroplasty. J Arthroplasty. 2002; 17:649–661.

13. Babovic N, Trousdale RT. Total hip arthroplasty using highly cross-linked polyethylene in patients younger than 50 years with minimum 10-year follow-up. J Arthroplasty. 2013; 28:815–817.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download