Abstract
Proximal femoral cephalomedullary nailing is one of the treatments of choice for intertrochanteric fracture. Zimmer Natural Nail® (ZNN; Zimmer) is one of the alternatives. We report two cases of broken tail portion of the ZNN lag screw during the removal procedure. This may be the first reported cases in scientific literature with this pattern of failure. We report these cases to highlight one of the possible problems that could occur during removal of this implant which can possibly prolong the operation time significantly if the required device is not prepared.
Proximal femoral cephalomedullary nailing is one of the treatments of choice for intertrochanteric fracture1). Long-term follow-up after this treatment also showed a satisfactory result2). Several type of implants are available include: the Gamma Nail (Stryker) and Proximal Femoral Nail Antirotation (PFNA; Synthes). Currently, Zimmer Natural Nail (ZNN; Zimmer, Warsaw, IN, USA) has become one of the emerging alternatives. Several cases of broken Gamma Nail (Gamma 3 nail; Stryker, Tokyo, Japan) and PFNA (Synthes, Paoli, Switzerland) have been reported previously3456). We report two cases of broken tail portion of the lag screw during removal of ZNN along with tips on the removal technique. To the best of our knowledge, a case of broken ZNN-particularly with this site of failure-has never been reported previously in scientific literature.
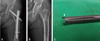
A 56-year-old female presented to our hospital complaining of acute right hip pain after a motorcycle accident. A plain pelvic radiograph revealed a stable intertrochanteric fracture (Fig. 1A). The patient was scheduled for surgical fracture fixation. Fixation of the fracture was performed using a ZNN (Cephalomedullary Asia) with the closed method under image intensifier guidance on an orthopaedic traction table. Intraoperative problems associated with the implant including lag screw insertion were not detected during the operation. Postoperatively, an anteroposterior pelvic radiograph was taken (Fig. 1B). Neither surgical wounds nor neurovascular complications were observed in this patient postoperatively. Complete bone union was obtained within 3 months after the operation. At 14 months postoperatively, the patient came to our hospital and desired removal of the implant. Physical examination revealed no abnormal findings with normal joint range of motion. A plain anteroposterior pelvic radiograph showed complete bone union with no sign of implant failure (Fig. 1C). Then, the operation for removal of the implant was scheduled. Implant removal was planned through the previous incision with the patient in lateral position. Intraoperatively, a problem was detected during removal of the lag screw. According to the manufacturer's protocol, after insertion of the original Zimmer lag screw inserter and retaining shaft (Fig. 2A, B), it was attempted to remove the lag screw by maneuvering it in the counter-clockwise direction. However, an unpredicted breakage of the tail portion of the lag screw occurred. Two pieces of the broken part of the tail portion of the lag screw were removed (Fig. 3A). A wider skin incision was made to obtain a good exposure of the tail of lag screw associated with clearing the bone and soft tissue around it. The use of clamping device was not possible, then removal of the lag screw was successfully performed by making new matched slots for reinserting the original Zimmer lag screw inserter and retaining shaft into the lag screw with use of a high speed burr with a 2 mm size of burr tip (Fig. 3B). Selection of the tip burr size and the burring site was important in order to make new matched slots (Fig. 3C). No significant problem was detected during nail removal after removing the lag screw. A bone allograft was inserted to fill the bone space after removing all implant parts. No complications occurred after the removal operation, and an anteroposterior pelvic radiograph was also taken postoperatively (Fig. 1D).
A 56-year-old female presented to our hospital complaining of left hip pain since 1 month ago. She had history of left intertrochanteric fracture and received surgical fixation at our hospital 1 year before. Previously, fixation of the fracture was also done using a similiar implant and procedure described in the previous case. No history of intraoperative problems detected during the operation. A recent anteroposterior hip radiograph showed a bone union with no sign of hardware failure (Fig. 4A). A lateral protruded tail portion of the lag screw was also noted and maybe causes a soft tissue irritation which induced pain. An operation for removal was planned. During operation, we tried to turn out the lag screw carefully using a Zimmer lag screw inserter and retaining shaft. An incomplete breakage of lag screw tail portion was noted at the similiar site with the previous described case (Fig. 4C). Fortunately the tail portion of the lag screw was more protruded in this case, later removal of the lag screw was successfully done using a clamping device (vise grip).
Only few publications have reported a broken lag screw of the cephalomedullary nail. Two cases of broken lag screws secondary to nonunion of pathologic fracture were reported in a review of 216 patients who underwent proximal femoral nail (PFN; Synthes) fixation by Ballal et al7). The broken site of the lag screw was at the proximal shaft of the lag screw at the junction between the lag screw and the nail. The removal technique was not reported in this study. However, we believe that removal of the broken lag screw in this type of failure would be relatively straight for ward because it is possible to remove the main nail before all parts of the lag screw are removed. A case of broken lag screw of the other type of Zimmer nail (Long IT/ST Nail) has been reported by Tantigate et al.8) along with the removal technique. In this case, the breakage site was similiar to the case reported by Ballal et al7). The author created a costumized removal tool using a used Arbeitsgemeinschaft für Osteosyn these fragen (AO) femoral nail. The lag screw was removed with the above explained device after trephine reaming of the bone-lag screw interface.
A recent publication by Zheng et al.9) reported about the difficulty in removing the lag screw secondary to breakage of an integrated compression screw of a Trigen intertan nail (Smith & Nephew). This reported mechanical failure was also associated with the breakage of the nail at the lag screw hole site. Breakage of the screwdriver during removal of the lag screw was also reported in this case. Difficulty in removing the lag screw occurs due to engagement of the lag screw thread and the compression screw thread. The lag screw was succesfully removed after a disengagement maneuver.
Different from the previously reported cases, in our cases, breakage of the cephalomedullary nail lag screw occurred during the elective implant removal operation. It also has an unpredicted particular breakage site. The implant removal operation is occasionally underestimated as an easy and fast procedure; therefore, special preparation is usually not performed. The lag screw portion is commonly fixed very strongly with the host bone, especially in younger patients; therefore, very strong power is needed to turn out the lag screw. The ZNN is a titanium nail and the tail portion of the lag screw that is engaged into the lag screw inserter and retaining shaft is relatively thin. This condition may explain why this situation occurred in our cases. The other important point to consider in removing this kind of implant is confirmation of perfect engagement of the lag screw tail into the tip of the lag screw inserter and retaining shaft before turning it in the counterclockwise direction for removing the screw. Thus, obtaining good exposure to the tail of the lag screw by making a wider incision and clearing the bone and soft tissue around the tail of the lag screw or a fluoroscopy use are recommended before trying to remove it. In our first case, the operation time was unpredicted to be prolonged. We report these cases to highlight one of the possible problems that may occur during removal of this kind of implant, especially in younger patients.
Figures and Tables
Fig. 1
Preoperative pelvic radiograph showed a stable intertrochanteric fracture (A). (B) Immediate postoperative radiograph. Stable fracture fixation was obtained even though the nail was inserted through the fracture site. (C) Radiograph taken at 14 months postoperatively showed complete bone union, no sign of loosening around the lag screw and showed no breakage previous to removal surgery (arrow). (D) After the nail removal radiograph, bonegraft filling of the bone space was performed.

Fig. 2
The original Zimmer lag screw inserter and retaining shaft; this device was also used for lag screw removal (A). (B) Tip of the device after assembling the two parts.

Fig. 3
Two pieces of the broken part of the lag screw head (large arrow) and new slots were made to match the lag screw removal device tip using a high speed burr (small arrow) (A). (B) After assembling the lag screw removal device tip to the new slots. (C) Ilustration on the original Zimmer Natural Nail® lag screw tail portion for the area of new created slots with size 5×3 mm (dashed line); arrow indicate the area of breakage site.

References
1. Kumar R, Singh RN, Singh BN. Comparative prospective study of proximal femoral nail and dynamic hip screw in treatment of intertrochanteric fracture femur. J Clin Orthop Trauma. 2012; 3:28–36.

2. Tyllianakis M, Panagopoulos A, Papadopoulos A, Papasimos S, Mousafiris K. Treatment of extracapsular hip fractures with the proximal femoral nail (PFN): long term results in 45 patients. Acta Orthop Belg. 2004; 70:444–454.
3. Gómeza PS, Díazb AF, Fernándeza JS. A simple removal method of a broken Proximal Femoral Nail (PFN). Injury Extra. 2006; 37:353–356.

4. Iwakura T, Niikura T, Lee SY, et al. Breakage of a third generation gamma nail: a case report and review of the literature. Case Rep Orthop. 2013; 2013:172352.

5. Park BJ, Cho HM. Removal methods for broken proximal femoral nails using ball tip guide wire: technical note and two cases report. J Korean Fract Soc. 2014; 27:315–320.

6. Kweon SH, Shin CH, Park JS, Choi BS. Breakage of cephalomedullary nail used in the treatment of proximal femur fractures: case report. J Korean Fract Soc. 2016; 29:42–49.

7. Ballal MS, Emms N, Thomas G. Proximal femoral nail failures in extracapsular fractures of the hip. J Orthop Surg (Hong Kong). 2008; 16:146–149.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download