Abstract
A dual mobility acetabular component has a structure that combines a polyethylene liner and a femoral head, unlike the general design of acetabular cups, making the dissociation of a polyethylene liner highly unlikely. In addition, it increases the range of motion and reduces the possibility of dislocations by increasing a jump distance. A fifty-one-year-old male who had received total hip arthroplasty with the dual mobility acetabular component visited a hospital for a posterior hip dislocation 10 weeks after the operation. At the emergency room, closed reduction was performed and the dislocation was reduced. However, plain imaging test revealed polyethylene liner dissociation after the closed reduction. Revision surgery was performed. We will report a rare case of early dislocation of the dual mobility acetabular component and dissociation of polyethylene liner accompanied with a literature review.
The dual mobility acetabular component was first introduced in 1974. The device reduces wear by improving the stability of a replacement and increases the range of motion12). The hemisphere of a polyethylene (PE) liner is bigger than an acetabular cup, causing its PE opening to be smaller than the diameter of a femoral head (Fig. 1). Therefore, the PE liner and the femoral head are held by a snap fit. The dual mobility acetabular component reduces the occurrence of dislocation after total hip arthroplasty and has little possibility of a PE liner dissociation12). Therefore, the implant is being used for patients at high risk of dislocation or patients who complain of continued instability. Only three cases of dislocation of hip and dissociation of PE liner after dual mobility acetabular component have been reported. This is the fourth case.
A 51-year-old male patient visited the hospital for a left femoral neck fracture that resulted from a fall (Fig. 2). He was receiving neurological treatments for epilepsy, alcohol dependence and behavior disorder, and had suffered from several falls and syncopes in the past. Moreover, there was a medical history of four episodes of seizures and syncopes for the past one year. A dual mobility acetabular component was used for this patient to reduce the risk of hip dislocation and to improve the range of motion of the hip joint, because he was a young patient and had a vulnerable condition for hip dislocation (Fig. 3). We used cementless acetabular component (Active Articulation™ E1® Hip System; Zimmer Biomet, Warsaw, IN, USA) and cementless femoral stem (Taperloc® Hip System; Zimmer Biomet). A physical examination carried in an operation room revealed normal range of motion; the joints showed no impingement on the neighboring tissues and no instability. No unusual signs were observed in an imaging test as the anteversion and inclination angles of an acetabular cup were 17° and 43°, respectively. The patient visited the hospital 10 weeks after the surgery in a drunken state, complaining of pain of the left hip joint that had occurred after seizure. In the plain radiograph conducted in the emergency department, a left hip dislocation was observed and reduced with closed reduction (Fig. 4). However, plain radiograph and computed tomography after reduction showed a dissociation of the PE liner that was not observed before closed reduction and eccentric location of femoral head against acetabular cup (Fig. 5). Therefore, we performed revision of acetabular component. During reoperation, the PE liner was found in the gluteus maximus muscles, and the acetabular cup, liner and femoral head were replaced because the acetabular cup and head were injured (Fig. 6). The femoral stem was not replaced since it was stable (Fig. 7). At the moment, he is under observation through the outpatient treatment with no unusual signs apparent.
The dual mobility acetabular component is used for patients at high risk of dislocation from total hip arthroplasty surgery and for patients who have chronic instability resulting from surgery or reoperation3). The component can reduce the wear of a liner, prevalence of dislocation and liner dissociation124). The implants reduce the wear with dual articulation by offering the PE liner mobility in the acetabular cup2567). In addition, it increases jump distance and postoperative stability by having the same effect as using a large femoral head7). The hemisphere of a PE liner in such products is bigger than an acetabular cup, causing its PE opening to be smaller than the diameter of a femoral head. Hence, during surgery, insert devices are used to snap fit and assemble the femoral head and PE liner (Fig. 8). It is rare to observe PE liner dissociation in a dual mobility acetabular component.
There are only a few reports of early dislocation of this implant. Philippot et al.4) reported 15-year results of 384 dual-mobility hips. In their series, 14 hips (3.6%) experienced dissociation between the femoral head and PE liner. The earliest dislocation occurred at 4 years postoperatively and the latest at 16 years (mean, 8.9 years). However according to a recent report8), early liner dissociation occurred at 3 years. In addition, after closed reduction, the patient had a hip joint crepitus and a palpable mass in buttock, but normal ambulation was possible. For this reason, the surgeons were asked to perform a plain radiography after closed reduction to confirm that the femur head is in the concentric position. Samona et al.9) also recently reported two cases dissociation of dual mobility prosthesis. One of the cases used the same product as ours. They described this dissociation as a bottleneck effect in which the PE articulating liner separated from the femoral head, which could have caused damage to the anti-dissociation mechanism into the new designs. In addition, they experienced two similar cases within a short period of time after surgery and were worried that these PE liner dissociations could also develop again in the future. There are two major causes when PE liner dissociation can occur. First, when assembling a femoral head and a PE liner, the femoral head should be inserted by rotating it clockwise with a specific handle until a popping sound is heard, but there are some cases where the femoral head is not inserted in this manner. However, such cases are easy to identify since the PE liner has a lower mobility and the hip joints have a limited range of motion. Secondly, the PE liner dissociation occurs as direct or indirect pressure is consistently applied to the liner from the outside. However, the PE liner hardly receives any direct pressure from the outside. So, the indirect pressure from the outside during forceful closed reduction can cause PE liner dissociation. Experimental results provided by Zimmer Biomet hip products10) required an average 195.3 N force to push the femoral head and PE, and required an average pulling force of 186.33 N pulling out of the head and PE. The authors opined that the latter reason occurred. Generally, forceful closed reduction is performed during dislocation after total hip replacement in the emergency room. However, liner dissociation can occur if closed reduction is imposed. So, gentle closed reduction under local or general anesthesia is necessary. In addition, if the reduction fails despite these attempts, it is considered to be open reduction rather than trying again.
In conclusion, to prevent dislocation for patients who are highly likely to have hip dislocation after total hip arthroplasty surgery, dual mobility acetabular component can be used. In the present case, dislocation occurred 10 weeks after surgery. Even though the femoral head and liner were firmly assembled, they dissociated during closed reduction. It is necessary for reduction of dual mobility cup to gentle reduction or open reduction under general anesthesia rather than forced manual reduction. This case highlights that we should be careful not only about dislocation after surgery but also dissociation of PE liner during closed reduction. Any signs of the PE liner dissociation should be checked through a plain radiograph after performing closed reduction. It is prudent to stay aware of the possibility of the structural problems of these devices.
Figures and Tables
 | Fig. 1A dual mobility acetabular hip implant has a bigger hemispherical polyethylene (PE) liner than an acetabular cup, causing its PE liner opening to be smaller than the diameter of a femoral head. |
 | Fig. 2Anterior-posterior (A) and translateral (B) views of both hip joints shows left femur neck fracture. |
 | Fig. 4Ten weeks from the surgery, posterior dislocation of the left hip joint was observed at the emergency department after slip down on anterior-posterior (A) and translateral (B) views of the hip joints. |
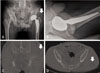 | Fig. 5After closed reduction of the dislocated hip joint, an eccentric position of the femoral head and the dissociation of polyethylene (PE) liner was observed in soft tissue (arrow) on anterior-posterior (A) and translateral (B) radiographs. The images of hip computed tomography. On the axial (C) and coronal (D) views, dissociated PE liner (arrows) was evident in the left gluteus maximus muscles. |
 | Fig. 6Injured articular surfaces of acetabular inner surface (white arrows) and femoral head (black arrow) were observed at removed aceatbular component and femoral head. |
References
1. Philippot R, Adam P, Reckhaus M, et al. Prevention of dislocation in total hip revision surgery using a dual mobility design. Orthop Traumatol Surg Res. 2009; 95:407–413.

2. Philippeau JM, Durand JM, Carret JP, Leclercq S, Waast D, Gouin F. Dual mobility design use in preventing total hip replacement dislocation following tumor resection. Orthop Traumatol Surg Res. 2010; 96:2–8.

3. Guyen O, Pibarot V, Vaz G, Chevillotte C, Béjui-Hugues J. Use of a dual mobility socket to manage total hip arthroplasty instability. Clin Orthop Relat Res. 2009; 467:465–472.

4. Philippot R, Camilleri JP, Boyer B, Adam P, Farizon F. The use of a dual-articulation acetabular cup system to prevent dislocation after primary total hip arthroplasty: analysis of 384 cases at a mean follow-up of 15 years. Int Orthop. 2009; 33:927–932.

5. Nellensteijn JM, Nellensteijn DR, De Jong T. Case report: Painless chronic liner dissociation of a total hip arthroplasty. Clin Orthop Relat Res. 2013; 471:1769–1772.

6. Langlais FL, Ropars M, Gaucher F, Musset T, Chaix O. Dual mobility cemented cups have low dislocation rates in THA revisions. Clin Orthop Relat Res. 2008; 466:389–395.

7. O'Neill CK, Napier RJ, Diamond OJ, O'Brien S, Beverland DE. Acetabular liner dissociation following total hip arthroplasty: a rare but serious complication that may be easily misinterpreted in the emergency department. Case Rep Emerg Med. 2015; 2015:802753.
8. Banka TR, Ast MP, Parks ML. Early intraprosthetic dislocation in a revision dual-mobility hip prosthesis. Orthopedics. 2014; 37:e395–e397.

9. Samona J, Flanagan B, Walter N. Acute disassembly and dissociation of a dual-mobility next-generation prosthesis. Orthopedics. 2016; 39:e980–e983.

10. Zimmer Biomet. The manual of G7® Acetabular System. Warsaw, IN: Biomet Orthopedics;2017. Available from: http://www.zimmerbiomet.com/medical-professionals/hip/product/g7-acetabular-system.html.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download