Abstract
Purpose
Atypical femoral fractures (AFFs) occur in two distinct part, subtrochanter and diaphysis. The aim of this study was to investigate the relationship between the lateral femoral bowing angle and the location of AFF.
Materials and Methods
This study included a total of 56 cases in 45 patients who underwent surgical treatment between January 2010 and December 2015. For the diaphyseal and subtrochanteric AFFs, we evaluated the relationship between the anatomic location and lateral femoral bowing angle. Lateral femoral bowing angle was measured by two orthopaedic surgeons and average value of two calibrators was used in statistic analysis. Other variables like age, height, weight, body mass index and bone mineral density were also evaluated. We also calculated the cutoff value for the location of the fractures from the raw data.
Results
The average lateral femoral bowing angle was 10.10°±3.79° (3°-19°) in diaphyseal group and 3.33°±2.45° (1.5°-11°) in subtrochanter group. Lateral femoral bowing angle was statistically significant in logistic regression analysis. According to the receiver operating characteristic curve, cutoff value for the location of the fracture was 5.25°. In other words, the femoral diaphyseal fractures are more frequent if the lateral femoral bowing angle is greater than 5.25°.
As the number of the elderly is increasing, the diagnosis and treatment for osteoporosis is also increased. Bisphosphonate (BP) is the most common drugs for the treatment of the osteoporosis. Several important clinical trials showed the effect of BP for the osteoporotic patients such as increased bone mineral density (BMD), decreased fracture incidences and bone turnover markers12345). Several authors reported potential complication of long-term alendronate therapy-atypical femoral fractures (AFFs), there have been growing concerns regarding the potential risk of AFFs among patients who is taking long-term BP678). However, AFFs have also been observed in patients who have never been exposed to BPs910). The American Society of Bone and Mineral Research (ASBMR) released their second report about atypical subtrochanteric and diaphyseal femoral fractures11). According to their report, one of the pathogenesis of the AFFs is stress or insufficiency fractures. These two types of AFFs, subtrochanter or diaphyseal fractures, have similar features except location. Koh et al.12) reported atypical lesions were clustered at the region of maximal tensile loading. We thought AFFs may happen according to the lateral femoral bowing angle in frontal plane. The object of this study was to investigate the correlation between the lateral femoral bowing angle in frontal plane and the location of AFFs.
Retrospectively, we reviewed all femoral fractures which were treated in our hospital from January 2010 to December 2015. Subtrochanteric fracture is femoral fractures where the fractures occur below the lesser trochanter to 5 cm distally in the shaft of the femur. Diaphyseal fracture is under the subtrochanteric region above the supracondylar area. We included the subtrochanteric and diaphyseal femoral fractures which had no or minor trauma, transverse or short oblique feature, non-comminuted shape, complete fractures with medial spike and incomplete fractures associated the lateral cortex hypertrophy10). Our exclusion criteria were as follow, metastatic bone tumor, metabolic bone disease except osteoporosis, femoral neck and trochanter fracture, high energy trauma and the cases which we couldn't have the intact femur antero-posterior radiographs.
According to our study design, a total of 56 cases in 45 patients were included. There were 44 females and one male. The subtrochanter fractures were 16 cases and the diaphyseal fracture were 40 cases. Among the subtrochanter fractures, 14 cases were unilateral fracture and 1 case was bilateral fractures. On the other hand, 10 patients were bilateral and 20 patients were unilateral in the diaphyseal fractures. The complete subtrochanter fractures were 14 patients and 14 cases and incomplete one was 2 patients and 2 cases. The complete diaphyseal fractures were 26 patients and 29 cases, 9 patients and 11 cases were incomplete. A basic number of patients included in current study are summarized in Table 1. The usage period of BP for osteoporosis was variable from 1 month to 162 months. Twenty out of 30 patients (66.7%) in diaphyseal fracture group and 9 out of 15 patients (60.0%) in subtrochanter fracture group were taking a BP. Among 29 patients who took BP, alendronate (14 patients) was the most and risedronate (12 patients), ibandronate (2 patients) and zoledronate (1 patient) follows as in order. Average duration of BP was 53.60±53.20 months in diaphyseal fracture group and 56.33±44.14 months.
We measured lateral femoral bowing angle at the contralateral intact femur in case of unilateral fracture. In bilateral fractures, we measured the angle in pre-injury intact femur roentgenogram. If we can't get the pre-injury pictures, these patients were excluded in this study. In the incomplete fractures, the angle was measured at the fractured femur. We got the standard anteroposterior view of the femur with the position of 15° internal rotation of lower extremity. To measure the lateral femoral bowing angle, we used the method described by Yau et al13). According to this method, the lateral femoral bowing angle in the coronal plane was measured by dividing the femoral diaphysis into 4 equal parts. Because Yau et al.13) didn't exactly describe the femoral diaphysis, we had defined the femoral diaphysis from the lower border of the lesser trochanter to upper border of the distal femoral segment which is defined by a square whose sides have the same length as the widest part of the femoral condyle so called rule of square. The overall lateral femoral bowing angle was measured as the angulation between the proximal and distal quarters of the femoral diaphysis (Fig. 1). The lateral femoral bowing angle was measured by two orthopaedic surgeons and average value of two calibrators was used in statistical analysis. Cohen's kappa coefficient to check the interobserver reliability was 0.3.
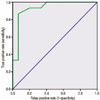
For statistical analysis, we used PASW Statistics version 18.0 (IBM Co., Armonk, NY, USA). After dividing two groups (subtrochanter and diaphyseal fracture), we compared the basic demographic data (age, height, weight, and body mass index [BMI]), the duration of BP use and BMD in spine, femur neck and total femur between two groups. The differences in characteristics between the two groups were compared using the chi-square test for nominal variables and Mann-Whitney U-test for continuous variables. Logistic regression analysis was performed to remove the influences of each variable between subtrochanter and diaphyseal fractures. Receiver operating characteristic (ROC) curves of the lateral femoral bowing angle was analyzed to calculate the sensitivity and specificity of the cutoff value. A P-value of less than 0.05 was considered to be statistically significant.
We compared the significance for the number of variables between the subtrochanter fracture group and diaphyseal fracture group with Mann-Whitney U-test (Table 2). The lateral femoral bowing angle was 10.10°±3.79° (3°-19°) in diaphyseal group and 3.33°±2.45° (1.5°-11°) in subtrochanter group. The average age was 75.30±7.80 years (60-85 years) in diaphyseal fracture group, 68.80±9.02 years (60-83 years) in subtrochanter group. The BMD of the spine was -2.73±0.85 (-0.43 to -3.75) in diaphyseal group and -1.91 ±1.13 (0 to -3.33) in subtrochanter group. These three variables, age, lateral femoral bowing angle, BMD of spine were statistically significant between two groups. Ten of thirty (33.0%) in diaphyseal fracture group and six of fifteen (40.0%) in subtrochanter fracture group had no history of taking a BP. The height, body weight, BMI, duration of BP use and BMD of femur neck and total femur were not significant.
In logistic regression analysis in order to remove the influences of each variable, we couldn't find any statistically significant variables between two groups. We thought this was because sample size is small and all variables were not independent variables especially age and BMD. Generally, it is considered that bone density decreases with age, so age and BMD could be dependent variables. For this reason, the analysis excluding the age and the analysis excluding the BMD were performed respectively (Table 3, 4). In the analysis excluding the age and BMD, as the lateral femoral bowing angle increases by 1°, the probability of a subtrochanteric fracture increases by 0.358 times and 0.389 times, respectively. According to the ROC curve, cutoff value of lateral femoral bowing angle was 5.25° (Fig. 2). In other words, the femoral diaphyseal fractures are more frequent if the lateral femoral bowing angle is greater than 5.25°.
Since the reports of Odvina et al.6) about severe suppression of bone turnover, many clinicians have started to pay attention to the long-term use of BP and its complications78). Among these complications, AFFs have attracted the attention in orthopaedic area. AFFs occur in two different region, subtrochanter and diaphyseal area. The important points in the pathogenesis of the AFFs are failure of the lateral aspect of the femur which has the maximal tensile stress. According to Koch's article14) about tensile and compression stress distribution on femur, subtrochanteric area has the highest tensile stress on lateral cortex. However, this classic model represents the femur without bowing on coronal plane. If the femur has the lateral bowing in coronal plane, this stress distribution may change. Oh et al.15) reported patients with femoral bowing showed the findings of mechanical analysis of the femoral shaft with a marked diffuse stress concentration on the anterolateral surface throughout the length of the femoral shaft.
In the current study, diaphyseal femoral fracture group have the average lateral femoral bowing angel of 10.10°±3.79° (3°-19°). On the other hand, subtrochanter fracture group have the average lateral femoral bowing angle of 3.33°±2.45° (1.5°-11°). The lateral femoral bowing angle in diaphyseal fracture group is statistically higher than subtrochanter fracture group. These data says the lateral femoral bowing angle is the main determinant for the location of the AFFs. It also supports the known pathogenesis of the AFFs, failure for the tensile stress.
Average age in diaphyseal fracture group is slightly higher than subtrochanter fracture group. This is statistically significant in Mann-Whitney U-test but not in logistic regression analysis. We couldn't make sure that lateral femoral bowing angle increases with age. However, we can guess the patients have the bowed femur are more likely to have a greater risk of diaphyseal femoral fractures over time due to the concentration of the stress on the apex of the bowing. In other words, aging itself is not a risk factor for diaphyseal AFFs, but if the patients have the bowed femur, fracture risk may increase over time.
In this study, the average BMD of the spine was -2.73±0.85 (-0.43 to -3.75) in diaphyseal group and -1.91±1.13 (0 to -3.33) in subtrochanter group. The BMD of the spine in diaphyseal AFFs is lower than subtrochanter ones (P<0.05). This is also statistically significant in Mann-Whitney U-test but not in logistic regression analysis. This also can be explained by the aging process. As we mentioned previously, disphyseal fracture group is slightly older than subtrochanter one. The BMD may decrease with age if the patients don't have the appropriate osteoporosis treatment.
A BP is well known risk factor for AFFs78910111617). The incidence of the patients taking a BP with AFFs was varying from 41.6% to 97%9171819). Our study showed about 60% of the patients had taken BP in both groups. We can't confirm the causal relationship between developments of AFFs and BP because about 40% of the patient didn't have the history of exposure to BP. In particular, we thought diaphyseal AFFs are strongly associated with femoral geometry and accumulation of the tensile stress. This is especially important pathomechanism in Asian ethnicity20). The absolute risk of a patient with AFFs being on BP is uniformly low from 0.006% to 1.1%212223). A careful approach is needed to say that the BP is a cause of AFFs. ASBMR task force also released revised case definition of AFFs. One of things that had changed is elimination of the use of pharmaceutical agents such as BP, glucocorticoids and proton pump inhibitors in minor features. Pathogenesis of AFFs with or without BP should be clarified by well-designed prospective randomized controlled study in the future.
Duration of the taking a BP is also known risk factor917). Average duration that patients had taken BP was about 53 months (1-120 months) in both groups. Though AFFs is associated with the BP, we don't know its causal relationship. So the osteoporosis treatment should be individualized and the clinicians should consider the risk and benefit of the treatment of BP. In many cases, the osteoporotic fractures including vertebral, hip and other fractures have been reduced with BP treatment12345). Patients should be carefully monitored the hip and thigh pain which may be a prodromal symptom of AFFs during the BP treatment.
A ROC curve is a graphical plot that illustrates the performance of a binary classifier system as its discrimination threshold is varied. We made a ROC curve with raw data. According to the ROC curve, cutoff value of lateral femoral bowing angle was 5.25°. In other words, the femoral diaphyseal fractures are more frequent if the lateral femoral bowing angle is greater than 5.25°.
This study has several limitations. The first is small number of enrolled patients and one surgeon's data. Considering the absolute low incidence of AFFs, multicenter study may be needed for large group of patients in the future. The second is only one ethnicity. AFF is more prevalent in Asian ethnicity. Because one of the contributing factors in development of AFF is bowing of the femur, this study doesn't represent the all ethnicity. Third, there is no reference for normal femoral bowing. We failed to find the article about normal bowing angle in adult femur. However, when we check the roentgenogram of the femur in young active general population, we can usually find the straight femur. In the current study, we thought the reference value of the lateral femoral bowing angle is zero. Fourth, the femur has also a bowing in the sagittal plane which may play a role in development of AFF. However, we didn't take this point in account because of normal anterior bowing of the femur. These limitations should be studied in the future. Although these limitations, the current study presented strong relationship between the degree of lateral femoral bowing and the location of AFFs, also showed the cutoff value of the lateral femoral bowing angle according to the location of AFFs.
Figures and Tables
Fig. 1
Femoral bowing was measured as the angulation between the proximal and distal quarters of the femoral diaphysis.

Table 2
The Statistical Significance for the Number of Variables between the Subtrochanter Fractures and Diaphyseal Fractures

References
1. Black DM, Cummings SR, Karpf DB, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996; 348:1535–1541.

2. Harris ST, Watts NB, Genant HK, et al. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. JAMA. 1999; 282:1344–1352.

3. McClung MR, Geusens P, Miller PD, et al. Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med. 2001; 344:333–340.

4. Black DM, Delmas PD, Eastell R, et al. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007; 356:1809–1822.

5. Chesnut CH 3rd, Skag A, Christiansen C, et al. Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J Bone Miner Res. 2004; 19:1241–1249.

6. Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab. 2005; 90:1294–1301.

7. Thompson RN, Phillips JR, McCauley SH, Elliott JR, Moran CG. Atypical femoral fractures and bisphosphonate treatment: experience in two large United Kingdom teaching hospitals. J Bone Joint Surg Br. 2012; 94:385–390.
8. Kang JS, Won YY, Kim JO, et al. Atypical femoral fractures after anti-osteoporotic medication: a Korean multicenter study. Int Orthop. 2014; 38:1247–1253.

9. Schilcher J, Michaëlsson K, Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med. 2011; 364:1728–1737.

10. Giusti A, Hamdy NA, Dekkers OM, Ramautar SR, Dijkstra S, Papapoulos SE. Atypical fractures and bisphosphonate therapy: a cohort study of patients with femoral fracture with radiographic adjudication of fracture site and features. Bone. 2011; 48:966–971.

11. Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014; 29:1–23.

12. Koh JS, Goh SK, Png MA, Ng AC, Howe TS. Distribution of atypical fractures and cortical stress lesions in the femur: implications on pathophysiology. Singapore Med J. 2011; 52:77–80.
13. Yau WP, Chiu KY, Tang WM, Ng TP. Coronal bowing of the femur and tibia in Chinese: its incidence and effects on total knee arthroplasty planning. J Orthop Surg (Hong Kong). 2007; 15:32–36.

15. Oh Y, Wakabayashi Y, Kurosa Y, Fujita K, Okawa A. Potential pathogenic mechanism for stress fractures of the bowed femoral shaft in the elderly: Mechanical analysis by the CT-based finite element method. Injury. 2014; 45:1764–1771.

16. Goh SK, Yang KY, Koh JS, et al. Subtrochanteric insufficiency fractures in patients on alendronate therapy: a caution. J Bone Joint Surg Br. 2007; 89:349–353.
17. Meier RP, Perneger TV, Stern R, Rizzoli R, Peter RE. Increasing occurrence of atypical femoral fractures associated with bisphosphonate use. Arch Intern Med. 2012; 172:930–936.

18. Beaudouin-Bazire C, Dalmas N, Bourgeois J, et al. Real frequency of ordinary and atypical sub-trochanteric and diaphyseal fractures in France based on X-rays and medical file analysis. Joint Bone Spine. 2013; 80:201–205.

19. Lo JC, Huang SY, Lee GA, et al. Clinical correlates of atypical femoral fracture. Bone. 2012; 51:181–184.

20. Sasaki S, Miyakoshi N, Hongo M, Kasukawa Y, Shimada Y. Low-energy diaphyseal femoral fractures associated with bisphosphonate use and severe curved femur: a case series. J Bone Miner Metab. 2012; 30:561–567.

21. Park-Wyllie LY, Mamdani MM, Juurlink DN, et al. Bisphosphonate use and the risk of subtrochanteric or femoral shaft fractures in older women. JAMA. 2011; 305:783–789.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download