Abstract
Purpose
The purpose of this study is to report the short-term outcomes of revision total hip arthroplasty (THA) using tantalum augments in patients with severe acetabular bone defects.
Materials and Methods
We retrospectively analyzed 15 revision THAs performed in 15 patients using tantalum augments between June 2010 and December 2013. Acetabular bone defects were Paprosky type IIIA in 7 hips, type IIIB in 7, and type IV in 1. The causes of revision surgery were aseptic loosening in 12 hips and deep infection in 3. Revisions were first in 1 hip, second in 3, and third in 11. Six patients were male and 9 female with a mean age of 59 years (range, 48-75 years). Mean follow-up was 29 months (range, 24-48 months).
Results
Mean Harris hip score was improved from 34 points (range, 12-54 points) preoperatively to 84 points (range, 38-90 points) at final follow-up. On the final follow-up radiographs, there were 12 hips (80.0%) with stable fixation of the acetabular cup, 2 (13.3%) with secondary stability after mild acetabular protrusion, and 1 (6.7%) with radiolucency around the acetabular cup without mechanical symptoms. Complications included one patient with acute hematogenous infection managed by surgical debridement and long-term antibiotic therapy. There were no cases with nerve palsy or dislocation during the follow-up period.
Total hip arthroplasty (THA) has proved to be effective procedure for reducing pain and improving joint function and is considered one of the greatest surgical achievements of the 20th. The numbers of revision THA procedures performed are on the rise despite technologic developments1). Prior to revision, surgeons should be prepared for what prosthesis types should be used depending on the severity of potential bone defects based on accurate preoperative radiographic measurements. Revision THA still remains highly controversial in terms of choice of devices and surgical procedures in patients with severe acetabular bone defects of Paprosky type III and IV2). To overcome these challenges, a variety of prostheses are being developed. Of these, tantalum metal augments introduced in 1997 possess a higher porosity and coefficient of friction than titanium alloy, and offer good bioactive and biological bond to bone. The high degree of porosity of tantalum metal augments appears to allow for optimal ingrowth, and their roughened surface microtexture provides a scratch fit for better initial stability upon implantation3). This material is increasingly used in revision THA with severe acetabular bone defects and its remarkable bone ingrowth properties have been demonstrated in recent short-term follow-up studies345).
The purpose of this study is to report the clinical and radiographic outcomes of revision THA using tantalum augments in patients with severe acetabular bone defects (Paprosky type III or IV) at a minimum follow-up of 2 years.
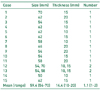
This study was performed after receiving an approval from the institutional review board of Samsung Medical Center (SMC 2016-02-093-002, Seoul, Korea). Of the 16 patients who underwent revision THA using tantalum augments, a total of 15 were retrospectively reviewed from June 2010 to December 2013 after excluding one patient who was lost because of a lack of follow-up. The severity of acetabular bone defects was evaluated preoperatively and categorized according to the Paprosky classification using X-rays and computed tomography scans2). Acetabular bone defects were Paprosky type IIIA in 7 hips, type IIIB in 7, and type IV in 1. The initial diagnosis was avascular necrosis of the femoral head in 6 hips, hip fractures in 3, sequelae of hip tuberculosis in 1, rheumatoid arthritis in 1, developmental dysplasia of hip in 1, and unknown cause in 3. The causes of revision surgery were aseptic loosening in 12 hips and deep infection in 3. Revisions were first in 1, second in 3, and third in 11. There were 6 men and 9 women with a mean age of 59 years (range, 48-75 years). Mean follow-up was 29 months (range, 24-48 months) (Table 1).
All operations were performed by a single surgeon using a posterolateral approach in 13 hips and anterolateral approach in 2. Previous acetabular components were removed, and then 1-2 tantalum augments were used based on the depth and size of the defect region after acetabular reaming using an acetabular reamer. Trabecular Metal™ augments (Zimmer, Warsaw, IN, USA) were used in all hips. The tantalum augment was fixed to fully intact acetabular bone with screws and fixed to the Trabecular Metal™ acetabular cup (Zimmer) with cement. In cases of osteolysis around the femoral stem on preoperative radiographs and intraoperative findings of instability, a femoral stem revision was performed together. Acetabular revision was done in 5 hips with concurrent femoral stem revision and 10 hips without. The bearing surfaces used were ceramic-on-ceramic in 5 hips and metal-on-polyethylene in 10. The femoral head sizes were 36 mm in 10 hips and 28 mm in 5.
Clinical and radiographic evaluations were performed preoperatively and at 6 weeks, 3 months, 6 months, and 1 year postoperatively, and then annually. Clinical evaluations were performed using the Harris hip-scoring system6). Radiographic analyses were performed using standardized anteroposterior and lateral radiographs of affected hips taken postoperatively, during hospitalization, and at each follow-up visit. All radiographs were digitized using PathSpeed software (General Electric Inc., Milwaukee, WI, USA) and reviewed by a single independent observer, who did not participate in clinical care. Radiolucent lines of >2 mm around the acetabular component were identified and assigned to one of the 3 zones described by DeLee and Charnley7). Acetabular cup loosening was defined as one of the following: i) any progression of radiolucent lines, ii) acetabular screw breakage, or iii) >2 mm of acetabular cup migration and a change in cup inclination angle of >4° degrees8). To evaluate the restoration of the hip joint center following the index revision THA, we measured the vertical shifts of the postoperative center of femoral head from the estimated center of femoral head referring to the contralateral intact hip joint9).
Statistical analysis was performed using PASW Statistics version 23.0 (IBM Co., Armonk, NY, USA). The paired t-test was used to compare Harris hip scores at last follow-up with scores prior to index procedures. Statistical significance was accepted for P-values <0.05.
The mean Harris hip score improved from 34 points (range, 12-54 points) preoperatively to 84 points (range, 38-90 points) postoperatively. The average size of Trabecular Metal™ augments used was 59.4 mm (range, 54-70 mm), the average thickness was 14.4 mm (range, 10-20 mm), and the mean number of augments used was 1.1 (range, 1-2) (Table 2). On the final follow-up radiographs, there were 12 hips (80.0%) with stable fixation of the acetabular cup (Fig. 1). Although 2 (13.3%) showed a mild acetabular protrusion, superolateral and inferomedial buttressing, and radial trabeculae indicated secondary stability. One hip (6.7%) with radiolucency around the acetabular cup and no symptoms is being followed up. When restoration of hip joint center was assessed postoperatively using radiographic measurements, assessment was impossible in 6 patients with a previous history of THA on the contralateral side. Excluding these patients, preoperative hip joint center was higher compared with the normal side in 9 patients. The average measurement of hip joint center restored from 26.6 mm (range, 12.9-45.6 mm) preoperatively to 10.38 mm (range, 0.4-19.0 mm) postoperatively. In regards to complications, one patient underwent debridement and insertion of an antibiotic-impregnated cement spacer as the first-stage revision and long-term antibiotic use due to acute hematogenous infection. There were no other complications or revisions, and no cases with nerve palsy or dislocation observed during follow-up.
Over the next 20 years, the rates of primary and revision THA in the United States are projected to rise to 174% and 137%, respectively10). This implies that surgical techniques and prosthetic choice will be emphasized even more in revision situations. Prior to revision, surgeons should be prepared for what prosthesis types should be used depending on the severity of potential bone defects based on accurate preoperative radiographic measurements. Aseptic loosening is known to be the most frequent cause of revision after THA, even after revision THA11). Aseptic loosening is associated with polyethylene wear debris that can stimulate an adverse local host response, resulting in bone resorption leading to severe bone defects and aseptic loosening of the prosthesis2). Revision THA still remains highly controversial in terms of choice of devices and surgical procedures in patients with Paprosky type III and IV severe acetabular bone defects2). To overcome these challenges, a variety of prostheses are being developed. Of these, tantalum metal augments-introduced in 1997-possesses a higher porosity and coefficient of friction than titanium alloy. Moreover, these tantalum components offer good bioactive and biological bond to bone, and its features include a high degree of porosity, which appears optimal for ingrowth, and a roughened surface microtexture that provides a scratch fit for better initial stability upon implantation3). This material is increasingly used in revision THA with severe acetabular bone defects and its remarkable bone ingrowth properties have been demonstrated in recent short-term follow-up studies345121314). Elganzoury and Bassiony4) followed up a total of 18 patients who underwent revision THA using tantalum augments. Of these, 15 patients (83.3%) had good or better results and tantalum components treated bone defects and enhanced fixation of other implants. Grappiolo et al.12) suggesting that the use of tantalum augments had a statistically significant influence on restoration of range of motion of the hip joint, improvement of patient satisfaction, recovery of limb length, and others. Tokarski et al.13) reporteded that a survival rate of 95% was achieved (434 out of 454 patients followed up for 40 months), and the risk of complications after revision such as infection was reduced. Del Gaizo et al.14) identified that the use of tantalum in revision was effective in pain relief and reduction of risk of complications. As several studies have demonstrated advantages of using tantalum augments, the use of tantalum augments in revision THA is expected to continue to increase. Furthermore, Gehrke et al.5) revealed satisfactory results in restoring range of motion of the hip joint and improving Harris hip score after revision THA using tantalum augments combined with bone grafting and a cemented cup for patients with severe acetabular defects. The combined use of tantalum augments with other prostheses is expected to be more effective, and further investigation is warranted.
Del Gaizo et al.14) reported that survival rate was 94% over 2 years after revision surgery in patients with Paprosky type III and IV bone defects and that complications requiring more than one revision occurred in 7 out of 36 patients. Of these 7 hips, revision was caused by periprosthetic fractures of the femur in 2 hips, acute infection in 3, and recurrent dislocation in 2. Grappiolo et al.12) followed up 55 cases (42 Paprosky type IIIA, 13 type IIIB) for an average of 53.7 months. Revision of the prosthesis was done in 4 cases (7.3%) due to aseptic loosening of the acetabular component in 3 and recurrent dislocation in 1. In the present study, stable fixation of the acetabular components was seen in 12 (80.0%) of 15 hips at an average follow-up of 29 months. No patients had undergone revision surgery due to mechanical failure of the acetabular components, excluding one patient with acute hematogenous infection that was managed by surgical debridement and long-term antibiotic suppression.
This study was limited by its retrospective nature, the relatively small sample size, and short follow-up period. Nevertheless, given the rarity of outcome data for revision THA with Paprosky type III and IV bone defects, we believe that the findings of this study are of value, because the study was based on patients with Paprosky type III and IV bone defects who were treated using tantalum augments by a single surgeon at a single institution.
In the present study, we observed satisfactory clinical and radiographic outcomes in patients who received revision THA using tantalum augments due to severe acetabular bone defects of Paprosky type III or IV at a minimum follow-up of 2 years. Based on the satisfactory results of this study and previous reports, we believe that revision THA using tantalum augments due to severe acetabular bone defects of Paprosky type III or IV could be an acceptable alternative method providing good mechanical stability.
Figures and Tables
Fig. 1
(A-C) A 64-year-old female patient with failed revision total hip arthroplasty using antiprotrusio cage and morselized allograft associated pelvic discontinuity (Paprosky type IV acetabular defect). (D) Radiograph 2 years after acetabular reconstruction using jumbo cup and tantalum augment showing a well-maintained acetabular construct.

References
1. Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009; 91:128–133.

2. Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994; 9:33–44.

3. Long WJ, Noiseux NO, Mabry TM, Hanssen AD, Lewallen DG. Uncemented porous tantalum acetabular components: Early follow-up and failures in 599 revision total hip arthroplasties. Iowa Orthop J. 2015; 35:108–113.
4. Elganzoury I, Bassiony AA. Early results of trabecular metal augment for acetabular reconstruction in revision hip arthroplasty. Acta Orthop Belg. 2013; 79:530–535.
5. Gehrke T, Bangert Y, Schwantes B, Gebauer M, Kendoff D. Acetabular revision in THA using tantalum augments combined with impaction bone grafting. Hip Int. 2013; 23:359–365.

6. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51:737–755.

7. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976; (121):20–32.

8. Lim SJ, Lee KH, Park SH, Park YS. Medium-term results of cementation of a highly cross-linked polyethylene liner into a well-fixed acetabular shell in revision hip arthroplasty. J Arthroplasty. 2014; 29:634–637.

9. Shi HF, Xiong J, Chen YX, Wang JF, Wang YH. Radiographic analysis of the restoration of hip joint center following open reduction and internal fixation of acetabular fractures: a retrospective cohort study. BMC Musculoskelet Disord. 2014; 15:277.

10. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007; 89:780–785.

11. Haynes JA, Stambough JB, Sassoon AA, Johnson SR, Clohisy JC, Nunley RM. Contemporary surgical indications and referral trends in revision total hip arthroplasty: A 10-year review. J Arthroplasty. 2016; 31:622–625.

12. Grappiolo G, Loppini M, Longo UG, Traverso F, Mazziotta G, Denaro V. Trabecular metal augments for the management of Paprosky type III defects without pelvic discontinuity. J Arthroplasty. 2015; 30:1024–1029.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download