Abstract
Purpose
This study aims to determine the correlation between the fracture patterns and the complications in patients with femoral neck fracture treated with internal fixation.
Materials and Methods
The study comprises 45 patients with femoral neck fracture treated with multiple screws or compression hip screw between May 2008 and April 2012. The mean age was 48 years at the time of the surgery and the mean duration from initial injury to surgery was 20 hours. The fracture patterns were identified according to the anatomical location, the Garden classification and the Pauwels classification. The occurrence of nonunion and avascular necrosis were reviewed with clinical results including Harris hip score and Lunceford hip function test. The correlation between the fracture pattern and occurrence of complications were analyzed.
Results
Fracture site union was achieved in 40 hips with the average union time of 17 weeks. Five nonunions occurred which showed high likelihood to occur in subcapital type, displaced (Garden stage III or IV) and Pauwels type III fractures (P<0.05). Avascular necrosis was developed in 10 hips which was mostly in subcapital type and Pauwels type III fracture but no statistical significance was found (P>0.05). The mean Harris hip score was 91 points, and Lunceford functional results were excellent in 15 hips, good in 24, fair in 4 and poor in 2.
The prevalence of femoral neck fracture has risen significantly due to increase in life expectancy in elderly patients and due to increased exposure to high energy injuries such as car accident or sport injury in young populations. The treatment modality of femoral neck fracture depends on the age, fracture severity and the expectation of the patient but the primary osteosynthesis with internal fixation is generally considered as a treatment of choice in the young patients. However, internal fixation can result in fatal complications such as avascular necrosis of femoral head (AVN) or nonunion thus the risk of reoperation remains high1234). The outcome of primary osteosynthesis depends on the patient's age at the time of the injury, the duration from the time of injury to the operation, the quality of reduction and the primary stability achieved by the prosthesis56). The fracture pattern is also considered to be an important prognositic factor as it can be an indicative of vessel injury and intrinsic stability. Number of previous studies has validated correlation of complications with each fracture types but, we feel it is necessary to update the previous studies with the Korean population. Therefore, in this study, we analyzed the radiological and the clinical result of the young patients who were treated with femoral neck fracture in effort to determine the correlation between the fracture type and the occurrence of nonunion and AVN. More specifically, we aim to find the contributing factors that lead to poor outcome.
The femoral neck fracture that were operated with primary osteosynthesis between May 2008 to April 2012 in Chosun University Hospital (Gwangju, Korea) were reviewed. The exclusion criteria was patients with age 70 years and older or adolescent under 18 years of age and pathologic fractures. With our exclusion criteria, 45 hips from 45 patients were availble for analysis which constitute the bases of our study. All patients were followed for minimum of 2 years (range, 24 to 75 months). Twenty five were male and 20 were female. The mean age of entire study group at the time of the surgery was 48 years (range, 19 to 69 years). We aim to operate within 24 hours from the time of the injury but the patients who were accompanied by other medical comorbidities which put patient to high risk for anesthesia were operated as soon as the general condition was improved and determined safe for operation. With this principle, the mean time to operation from the time of the injury was 20 hours (range, 2 to 48 hours). Using anatomical classification, 25 hips were classified as subcapital type while transcervical and basicervical was 12 and 8, respectively. Using Garden classification, type III fracture was the most common type with 22 hips followed by type II with 16, type IV with 5 and type I with 2. With Pauwels classification, 2 patients were type I, 18 were type 2 and 25 were type III (Table 1).
All operation was performed in supine position with conventional operation table using lateral approach to proximal femur. In non-displaced fractures or valgus impacted fractures, the fractures were fixated in situ without reduction while in displaced fractures, closed reduction was performed using Whitman method; briefly, the hip was initially placed in extension with traction in slightly externally rotated and abducted position. The attempt to reduce was made by internally rotating and adducting the hip and the achieved reduction was confirmed with portable C-arm fluoroscopy by checking anteroposterior and direct lateral view. The fixation was performed after successful anatomical reduction was achieved. Multiple cannulated screws (6.5 mm cannulated screw, Solco, Pyeongtaek, Korea) were used in 38 hips while compression hip screws (Zimmer, Warsaw, IN, USA) were used in remaining 7 hips. Of note, all cases which used compression hip screw was basicervical type fractures.
When multiple cannulated screws were used, the first screw was placed along the calcar femorale, the second screw on posterior cortex and the third screw on anterior cortex so that the head of the three cannulated screws formed reverse triangular shape (Fig. 1). However, in 8 cases with severe comminution, additional fourth screw formed diamond shape. The screw was inserted so that the distal tip to the subchondral bone distance was less than 5 mm in each screw and special care was taken to prevent cortical perforations during guide pin or screw placement. When compression hip screw was used, the screw was introduced at the center of the femoral head and the tip to apex distance was confirmed to be under 25 mm with fluoroscopy (Fig. 2).
For radiographic evaluation, preoperative and postoperative simple radiograph and computed tomography (CT) scan were taken during the follow up. Additionally, bone scan, single-photon emission CT/CT and magnetic resonance imaging were used if diagnosis of nonunion or AVN was questionable. In the simple radiograph, Garden alignement index was checked by measuring the angle of the compression trabeculae related to the longitudinal axis of the femoral shaft in anteroposterior and lateral view. Anatomical reduction was defined when Garden alignment index was between 160° and 180° in anteroposterior view and 180°±10° in lateral view78). The initial fixation was considered stable when screw tip to subchondral bone distance was less than 5 mm with use of cannulated screw or when tip to apex distance is less than 25 mm with use of compression hip screw. The position of the screws and the fracture site alignment was assessed by comparing the latest follow up radiograph to that of the immediately after the operation and fixation failure was defined when there are 1) more than 10 mm displacement, 2) progression to varus angulation, 3) more than 5% change between the axis of the screws, 4) more than 20 mm of posterior translation, and 5) femoral head perforation91011). Nonunion was diagnosed when evidence of bone healing could not be witnessed after 6 months11), and AVN was defined if the patients complained of pain and the simple radiograph shows cystic change, femoral head collaps, focal bone radiolucency12). When one of these evidences were presented, advance imaging was taken to further confirm the diagnosis. For the functional outcome, Harris hip score and Lunceford hip functional score were used to evaluate the pain, ability to walk, and performance daily activities13).
The aim of the current study is to find out whether the fracture classifciation can predict nonunionor AVN. To fulfill our purpose, JMP software (SAS Institute, Cary, NC, USA) was used for the statistical analysis independantly for each classifications and for complications. Chi-squared test was used and if any category or classification had fewer than 5 patients, Fisher's exact test was utilized. Due to the relatively small number of cases, rather than compare each categories of Garden classifcation, Garden type I and II were grouped as undisplaced fracture while type III and IV were grouped as displaced fracture. Significance was set at P-value less than 0.05.
The mean screw tip to subchondral distance was 5.7 mm (range, 3.7 to 8.2 mm) and all hips were noted to achieve stable fixation when simple radiographs immediately following the operation were assessed. The bone union was achieved in 40 hips with the mean of 17 weeks (range, 8 to 32 weeks) from the time of the surgery. Delayed union and the nonunion occurred in 5 cases respectively. All 5 nonunions occurred in subcapital type of fracture. Using Garden classification, 3 cases were classified as type III and 2 were type IV while all 5 were classified as type III fracture when Pauwels classification was used. With the statistic analysis, nonunion was significantly high in subacaptal type fracture, with displacement (Garden type III and IV) and vertically oreiented fracture line (Pauwels III type fracture) (Table 2). Of the hips with nonunion, 2 were treated with total hip replacement while one had valgus osteotomy and blade plate fixation which was healed without further complications. Remaining 2 cases were treated conservatively as the patients refused to undergo additional operation but both patients were unable to achieve bonunion at the last follow up. The Garden alignment index showed mean of 168° (range, 155° to 179°) in anteroposterior view and 176° (range, 170° to 183°) which were within acceptance rate. However, 4 hips developed varus malunion during the follow up. One of these 4 malunion cases advanced to AVN while other three were healed uneventfully. However, although significance was not achieved, the Harris hip score of the malunion hips were lower than that of the hips without evidence of malunion (mean 66.0 and 81.1, respectively). The AVN was diagnosed in 10 hips with majority (7 hips) occured in Garden type III fracture which was followed by type II (2 hips) and type IV (1 hip). No statistical significance was found between the displacement of the fracture and the occurrence of AVN (P=0.1294). Using anatomical classification, seven of the AVN hips occurred in subcapital type while 3 in transcervical type fracture. With Pauwels classification, 1 hip was classified as type I, 5 hips as type II and 4 hips as type III. No significance was found when occurrence of AVN was correlated with anatomical classification or Pauwels classification (P=0.1038 and 0.6768, respectively). The severity of AVN was determined according to the Arco classification and diagnosed to be stage Ia in 4 hips, Ib in 3, IIb in 2 and IIIa in 1. One hip with stage IIIa rquired total joint replacement (Fig. 3) while other 9 hips did not progress and were treated conservatively. The time to index operation on the patients who developed AVN were 18 hours which was longer than mean of entire group (14 hours) but the difference did not reach significance (P>0.05). At the most recent follow up, the harris hip score was 91 points (72 to 100 points) and using Lunceford hip function score, excellent result was on 15 hips, good in 24, fair in 4 and poor in 2.
Femoral neck fracture commonly occurs in the old age but recent data indicates that prevalence rate has increased in the younger population due to the increased exposure to the car accidents and the high energy sports injuries2). The treatment method should be selected based on numerous factors including patient's age, medical comorbidities and patient's expectation but the fracture severity including level of comminution and displacement should also be considered. In the younger population, primary osteosyntheisis is recommended as it is relatively inexpensive and minimally invasive procedure. Also with adequate reduction, maximal bone contact can be achieved which is sufficient for early immobilization and efficiently promote bone healing1714). Specially, when the cannulated screw is used as a fixation method, the use of guide wire can accurately determine the size and the position of the screw thereby providing optimal stability even with minimal invasion to the fracture site411) The operation of femoral neck fracture is usually perfromed with the use of fracture table but in the current series, all operations were performed using conventional operation table. Our institution prefer this method as this requires less preparation time and the stability of the frature after the screw fixaqtion can be tested immediately. However, the operation result depends on the experience and proficiency of the operator and the exposure to radiation by the fluoroscopy, risk of fixation failure, nonunion and AVN remains possible complications1234). When the primary osteosynthesis is attempted in the femoral neck fracture, AVN is reported to occur in 10-45% and nonunion in 10-30%3561415). This is consistent with our series as the nonunion occurred in 11% and AVN in 22%.
The Garden type I and II fractures are non displaced fracture and considered to be associated with none or minimal vessel injury as compare to the type III and IV fractures and the previous studies reported favorable outcome in this fracture types16). Also, numerous studies considered preoperative displacement as an important prognostic factor after internal fixation is performed and emphasized on the importance of anatomical reduction and secure fixation to decrease the occurrence of postoperative complications including nonunion and AVN217). In the current study, all of the nonunion occurred in displaced fracture (3 in Garden type III and 2 in Garden IV) and statistically, it was confirmed that the displacement had significantly high likelihood of developing nonunion (P<0.05). Similar trend was found in the hip with AVN as out of 10 AVN hips, 8 occurred in displaced fractures (7 in Garden type III and 1 in type IV). With the number available for analysis, the statistical significance was not reached (P>0.05) but as majority of AVN occurred in Garden type III and IV fractures, we believe that the amount of displacement could also have an influence on the AVN. Thus we believe presence of displacement is a risk factor for developing both AVN and nonunion after femoral neck fracture.
The study from Callaghan et al.18) and Leonardsson et al.19) reported high rate of AVN in the subcapital type fracture as the vessels are likely to be injured during the injury or during the reduction process. The manipulation of the fracture site and applying internal fixation can potentially increase rotational displacement and could further damage the blood vessels which may ultimately result in AVN. Our study also showed that the even after anatomical reduction was achieved, the subcapital type had higher rate of developing nonunion and AVN. In the other hand, even in the subcaptial type of fracture, the number of complication was very small in impacted fractures when the fractures were treated by in situ fixation without reduction.
According to the Pauwels classification, more vertical oriented type of fracture can result in increased shear stress and theoretically in risk of nonunion. However, the interpretation of the fracture type using simple anteroposterior X-ray has been reported to have high interobserver error and the thus the correlation between Pauwels classification and the nonunion was unclear20). In the current study, authors tried to minimize the error of classifying the fractures by having three evaluators. The classification was determined based on the agreement of the evaluators. With this method, we were able to find that the Pauwels type III fracture significantly high likelihood of developing nonunion as all 5 nonunions in our series occurred from this type of fracture.
Eighty percents of the AVN of femoral head is reported to occur within 6 months to 2 years from the time of the injury2). The AVN in our series occurred at the mean of 15 months (range, 6 to 27 months) which is consistent with the previous study but diagnosis was made after 2 years in one patient suggesting possibility of developing AVN even after bone healing is achieved. Therefore, longer follow up is required to accurately determine the occurrence of AVN.
Despite the high percentage of displaced fracture in our study, the overall clinical outcomes were satisfactory with the mean Harris hip score of 91 points (range, 72 to 100 points) and 86% good or excellent result in Lunceford hip function score. We believe this favorable result is due to the following reasons: first, we had tried to achieve anatomical reduction to gain acceptable Garden index, second, the subject patients were relatively young and therefore due to better muscle strength and bone quality, secure screw fixation and prompt rehabilitation was possible, and third, although AVN occured in 10 patients, they remained in early stage without progression and developed only minimal clinical symptoms.
The limitation of the current study includes relatively small number of patients which prevented statistical anaylsis for each complication categories. Also, although the subject of the current study included only the patients with more than 2 year follow up, the result of longer follow up is necessary.
The occurence of nonunion in subcaptal type fracture, Garden stage III and IV fracture and Pauwels III fracture were higher than other type of fractures with statistical significance. Also, although statistical significance was not reached, there was high likelihood of developing AVN in subacapital type femoral neck fracture and displaced fracture. Therefore, these fracture types should be treated with special care to achieve anatomical reduction and stable fixation to minimize complications.
Figures and Tables
Fig. 1
(A) Simple anteroposterior radiograph of pelvis shows nondisplaced femoral neck fracture. (B, C) Immediate postoperative radiographs showing internal fixation with 3 cannulated screws. (D, E) Postoperative 2 years and 8 months radiograph showing bone union without complications.
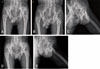
Fig. 2
(A) Simple anteroposterior radiograph of pelvis shows displaced basiceervical type femoral neck fracture. (B, C) Immediate postoperative radiographs showing internal fixation with compression hip screw. (D, E) Postoperative 2 years and 3 months radiograph showing bone union without complications.
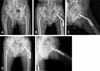
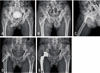
Fig. 3
(A) Simple anteroposterior radiograph of pelvis shows displaced femoral neck fracture. (B, C) Immediate postoperative radiographs showing internal fixation with 4 cannulated screws. (D) Postoperative 3 years and 6 months radiograph showing avascular necrosis of right femoral head. (E) Secondary postoperative radiograph of pelvis showing total hip arthroplasty.
References
1. Kaplan T, Akesen B, Demirağ B, Bilgen S, Durak K. Comparative results of percutaneous cannulated screws, dynamic compression type plate and screw for the treatment of femoral neck fractures. Ulus Travma Acil Cerrahi Derg. 2012; 18:65–70.

2. Pauyo T, Drager J, Albers A, Harvey EJ. Management of femoral neck fractures in the young patient: A critical analysis review. World J Orthop. 2014; 5:204–217.

3. Yang JJ, Lin LC, Chao KH, et al. Risk factors for nonunion in patients with intracapsular femoral neck fractures treated with three cannulated screws placed in either a triangle or an inverted triangle configuration. J Bone Joint Surg Am. 2013; 95:61–69.

4. Bhandari M, Devereaux PJ, Tornetta P 3rd, et al. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Joint Surg Am. 2005; 87:2122–2130.

5. Huang TW, Hsu WH, Peng KT, Lee CY. Effect of integrity of the posterior cortex in displaced femoral neck fractures on outcome after surgical fixation in young adults. Injury. 2011; 42:217–222.

6. Jain R, Koo M, Kreder HJ, Schemitsch EH, Davey JR, Mahomed NN. Comparison of early and delayed fixation of subcapital hip fractures in patients sixty years of age or less. J Bone Joint Surg Am. 2002; 84-A:1605–1612.

7. Blomfeldt R, Törnkvist H, Ponzer S, Söderqvist A, Tidermark J. Comparison of internal fixation with total hip replacement for displaced femoral neck fractures. Randomized, controlled trial performed at four years. J Bone Joint Surg Am. 2005; 87:1680–1688.

8. Szita J, Cserháti P, Bosch U, Manninger J, Bodzay T, Fekete K. Intracapsular femoral neck fractures: the importance of early reduction and stable osteosynthesis. Injury. 2002; 33:Suppl 3. C41–C46.

9. Alho A, Benterud JG, Solovieva S. Internally fixed femoral neck fractures. Early prediction of failure in 203 elderly patients with displaced fractures. Acta Orthop Scand. 1999; 70:141–144.

10. Min BW, Bae KC, Kang CH, Song KS, Kim SY, Won YY. Valgus intertrochanteric osteotomy for non-union of femoral neck fracture. Injury. 2006; 37:786–790.
11. Haidukewych GJ, Rothwell WS, Jacofsky DJ, Torchia ME, Berry DJ. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J Bone Joint Surg Am. 2004; 86-A:1711–1716.

12. Bray TJ. Femoral neck fracture fixation. Clinical decision making. Clin Orthop Relat Res. 1997; (339):20–31.
13. Lunceford EM Jr. Use of the moore self-locking vitallium prosthesis in acute fractures of the femoral neck. J Bone Joint Surg Am. 1965; 47:832–841.

14. Khoo C, Haseeb A, Ajit Singh V. Cannulated screw fixation for femoral neck fractures: A 5-year experience in a single institution. Malays Orthop J. 2014; 8:14–21.
15. Nikolopoulos KE, Papadakis SA, Kateros KT, et al. Long-term outcome of patients with avascular necrosis, after internal fixation of femoral neck fractures. Injury. 2003; 34:525–528.

16. van Embden D, Roukema GR, Rhemrev SJ, Genelin F, Meylaerts SA. The Pauwels classification for intracapsular hip fractures: is it reliable? Injury. 2011; 42:1238–1240.

17. Ly TV, Swiontkowski MF. Treatment of femoral neck fractures in young adults. J Bone Joint Surg Am. 2008; 90:2254–2266.
18. Callaghan JJ, Liu SS, Haidukewych GJ. Subcapital fractures: a changing paradigm. J Bone Joint Surg Br. 2012; 94:11 Suppl A. 19–21.
19. Leonardsson O, Sernbo I, Carlsson A, Akesson K, Rogmark C. Long-term follow-up of replacement compared with internal fixation for displaced femoral neck fractures: results at ten years in a randomised study of 450 patients. J Bone Joint Surg Br. 2010; 92:406–412.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download