Abstract
Marfan syndrome is an autosomal dominant and could decrease bone mineral density. So patients with Marfan syndrome could vulnerable to trauma in old ages. We present the first report, to the best of our knowledge, of a rare fracture of the femoral neck with a minor traumatic history in a juvenile Marfan syndrome patient whose physis is still open. Although the patient is young, her bone mineral density was low and the geometry of femur is changed like old ages. The femur neck fracture in children is very rare and only caused by high energy trauma, we concluded that the Marfan syndrome makes the bone weaker in young age and preventative medications to avoid fractures in younger Marfan syndrome patients are necessary in early ages.
Marfan syndrome is an autosomal dominant disorder of the connective tissue that affects the cardiac system, eyes, and skeletal system. The genetic basis of Marfan syndrome is related to chromosome 15, which encodes fibrillin-1 and 2. The major orthopedic manifestations of Marfan syndrome include scoliosis or lordosis, chest wall deformities (pectus excavatum), dural ectasia, joint hypermobility, acetabular protrusion, pes planus, arachnodactyly, increased height, and a long arm span1). Decreased bone mineral density (BMD) has also been reported in patients with Marfan syndrome. In addition, there have been some reports of adult Marfan patients being predisposed to fractures2). Here, we present the first report, to the best of our knowledge, of a rare fracture of the femoral neck with a minor traumatic history in a juvenile Marfan syndrome patient with an open physis.
A 14-year old female presented with the sudden onset of right hip pain after stepping forward to toss a shuttlecock. The patient reported that it was the first incidence of hip pain, and there was no previous history of other musculoskeletal pain or disease before this admission. In physical examinations, the patient had severe pain on her right inguinal area and was unable to stand on her right limb; however, there were no external wounds or other neurological complaints. She was 180 cm tall and had a prominent pectus excavatum (Fig. 1), a long arm span, spider-like hands, and scoliosis of her back. Her hand span to length ratio of 1.3 (>1.05). The patient’s uncle had been diagnosed with Marfan syndrome and aortic valvular disease, and he had a valve replacement surgery at his aortic valve the previous year. According to the criteria for diagnosing the Marfan syndrome, we diagnosed her as a young Marfan syndrome patient.
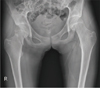
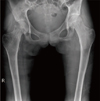
The initial pelvic X-ray revealed a transcervical fracture of the right femoral neck area (Fig. 2). Both of her hip joints had coxa valga appearances (her neck-shaft angle was 142.9° which was higher than 120°-135° as normal value) and both femur necks were 4.02 cm (normal elderly mean femoral neck width 3.27 cm3)). However, there was no acetabular protrusion or other specific radiological findings of Marfan syndrome. Her thoracic (T)-lumbar (L) spine X-ray revealed scoliosis and a Cobb’s angle of 25° (T10 to L4), while the other radiological findings were unremarkable (Fig. 3). A genetic evaluation for Marfan syndrome was refused because of the cost, as well as the possibility of having a “genetic stigma”.
Although the patient had a very low energy trauma, her femoral neck was fractured. To differentiate the pathologic factures we conducted the following serology tests: the C-telopeptide of collagen bone resorption marker was high at 2.120 ng/mL (<0.573 ng/mL); the 1,25-(OH)2 vitamin D3 bone formation marker was 35.45 pg/mL (19.6-54.3 pg/mL); and the osteocalcin bone resorption marker was 33.7 ng/mL (11-43 ng/mL). The patient’s initial BMD (checked for the first time in her life) showed osteoporotic conditions in her spine and femur. Her mean spine BMD from L1 to L4 was 0.831 g/cm2, Z-score was −2.3. In the patient’s femur, the Z-score of her femur neck BMD was 0.69 g/cm2. The Z-score was 0.456 g/cm2 in her femur ward’s triangle 0.338 g/cm2 in her femur major trochanter and 0.582 g/cm2 in her total femur (Fig. 4).
Emergency surgery was performed for a closed reduction and internal fixation with cannulated screws. Before the operation, we requested an urgent consultation with cardiology, including a chest angiography, computed tomography and echocardiography. There were no dilations or aneurysms at the aorta, and the patient’s cardiac function was normal; therefore, there was a low risk for general anesthesia, and the emergency operation was performed. The surgery was conducted within 6 hours, which is the golden time for an young age femur neck fracture. The closed reduction and internal fixation were done using a intraoperative radiologic device and 3 cannulated hip screws. The intraoperative images revealed a satisfactory reduction and stability of the fractured femur and the early post-operative X-rays showed a stable fixation. And there was no post-operative complications (Fig. 5).
At the 12-month follow up, the patient had no problems with ambulation or weight bearing, and an X-ray of the fractured site showed good union of the fracture, so a hardware removal operation was planned. After the hardware removal, there was no evidence of displacement and malalignment. The avascular necrosis (AVN) of the femoral head, one of the most common complications, was not observed until 12 months post-operatively (Fig. 6) and her BMD was recovered to normal with calcaium and vitamin D supplement therapy.
Marfan syndrome is an autosomal dominant disorder of the connective tissue, with an incidence in the general population of approximately 1 in 10,000. Almost 15% of the cases occur in the absence of a family history, representing new mutations14). With a positive family history, an affected person should display one major criterion in an organ system, and the involvement of a second organ system. The musculoskeletal criteria requires at least four phenotypic expressions, including: pectus excavatum/carinatum, reduced upper to lower body segment ratio or hand span to length ratio of >1.05 (museaured by height and arm span. Standing height was measured with footwear removed. Arm span was defined as the maximal distance between the tips of the two middle fingers with arms outstretched in centimeters and the patient standing against the wall), wrist and thumb signs, scoliosis of >20° or spondylolisthesis, reduced extension of the elbows <170° (also evident in the fingers, often referred to as spider-like hands due to flexion contractures of the interphalangeal joints), medially displaced medial malleoli, and acetabular protrusion5). And this could accompany with the significant osteopenia and fairly high prevalence of fractures in old ages2).
Generally hip fractures in children usually occur with high energy, often life threatening injuries. Additionally, complications, such as osteonecrosis, coxa vara, non-union, and premature physeal closure, can severely decrease their functional outcomes, aggressive treatment is necessary5). But in this case, the young patient’s femur was fractured by the only a minor trauma. There have been reports of traumatic femur neck fractures, with or without skeletal deformities, as a result of Marfan syndrome, but our patient developed a fracture with only little traumatic history especially in young age.
Preparing the surgical treatment of her femur neck fracture, we evaluated her Z-score. Several investigators have reported that the BMD is decreased in patients with Marfan syndrome. For example, Le Parc et al.6) using dual energy X-ray absorptiometry (DXA) showed a significant decrease in BMD at the hip and radius in adult men and women affected with Marfan syndrome and decrease was observed equally in affected men and women. Additionally, Kohlmeier et al.7) performed DXA studies in a series of 32 women and 14 children with Marfan syndrome. They observed that bone mass is decreased in women with Marfan syndrome, presented that Marfan children have age-specific deficits in bone mineral at the lumbar spine and femoral neck and recommend that adequate calcium uptake and safe weightbearing activity or hormonal therapy for osteoporosis in Marfan syndrome patients should be considered7).
Our patient was an adolescent, and we attempted to interpret the values with the methods for analyzing pediatric BMD scores. In interpreting pediatric BMD scores, the T-score (comparison of the current Z-score with the peak adult BMD) usually used in the adult interpretation of the DXA should not be included in the pediatric DXA report8). Therefore, we applied our patient’s BMD values to the mean values of 14 year-old Korean girls910): the BMD of the lumbar spine (L1 to L4) and femur neck are 0.886 g/cm2 and 0.76 g/cm2, and the standard deviations (SDs) are 0.106 and 0.131, respectively. According to these values, our patient’s BMD values were lower than those of the girls her age in the femur neck and in multiple spine levels (L1 to L4). While calculating the Z-scores8), our patient’s Z-score of the spine was −0.46 and of the femur neck was −0.53. We concluded that her bones are osteopenic and more vulnerable than other girls her age.
In our case, she showed coxa valga appearance on her femur and increased femur neck width. In previous reports, the neck-shaft angle showed significant differences between the fracture patients and controls in the elderly patients (60 to 90 years old) of both sexes. The increase in the neck-shaft angle was associated with a relative risk for hip fractures, and the mean femoral neck width was higher in the fracture cases than in the controls in both sexes. For an increase of 1 SD in the mean femoral neck width, the risk for hip fracture increased more than twofold in both sexes. Based on this report, as osteoporosis progresses, the femoral neck is widened and neck-shaft angle is increased to compensate for the weakened bones3). Although the subjects of this research were elderly patients between 60 and 90 years old, we assumed that her increased neck-shaft angle and femur neck width could represent the compensatory change about her osteoporotic bone quality which made the bone fragile.
Through the previous reports and clues that representing her osteoporotic bone quality, we conclude that her femur neck fracture was due to the low BMD and osteoporotic bones. So we treated our patient with bone mineral replacement therapy as in the previous reports.
Although relationship between vascular abnormalities and abnormality in the skeletal system, such as AVN of the femur, has not been clearly described, there are some reports that Marfan syndrome patients presenting with fractured femur necks may have an increased risk of developing AVN due to the disease’s vascular system phenotype1). But in our case, there was no apparent AVN on the patient’s femur until her last follow up.
Here, we reported the case of a 14 year-old juvenile Marfan syndrome patient with a femoral neck fracture caused by a minor traumatic history. To our knowledge, it is the first time that this has been reported in the literature. It is known that Marfanoid patients who have a low BMD and skeletal deformities are vulnerable to trauma in old ages. But in our case, a young adolescent aged patient who had no skeletal deformities, got femur neck fracture which is rare and usually caused by high energy trauma, just stepping forward to play badminton. We concluded that although she was young, her Marfan syndrome made her bone osteoporotic, which is represented by increased neck-shaft angle and neck width. And this change caused her femur neck fracture. Although a Marfan syndrome patient has no other skeletal deformity which can cause fractures like acetabular protrusion except an increased neck shaft angle and femoral neck width, that patient should be treated as having a high risk for a femoral neck fracture. Consideration of preventative treatment as well as increased calcium uptake, safe weightbearing and bone mineral replacement therapy for the patient should be needed.
Figures and Tables
References
1. Hindocha S, Kershaw S, Clayson AD. Atraumatic fracture neck of femur in Marfan’s syndrome: a case report. Injury Extra. 2007; 38:343–345.

2. Moura B, Tubach F, Sulpice M, et al. Bone mineral density in Marfan syndrome. A large case-control study. Joint Bone Spine. 2006; 73:733–735.

3. Alonso CG, Curiel MD, Carranza FH, Cano RP, Peréz AD. Femoral bone mineral density, neck-shaft angle and mean femoral neck width as predictors of hip fracture in men and women. Multicenter Project for Research in Osteoporosis. Osteoporos Int. 2000; 11:714–720.
4. Avivi E, Arzi H, Paz L, Caspi I, Chechik A. Skeletal manifestations of marfan syndrome. IMAJ. 2008; 10:186–188.
5. Boardman MJ, Herman MJ, Buck B, Pizzutillo PD. Hip fractures in children. J Am Acad Orthop Surg. 2009; 17:162–173.

6. Le Parc JM, Plantin P, Jondeau G, Goldschild M, Albert M, Boileau C. Bone mineral density in sixty adult patients with Marfan syndrome. Osteoporos Int. 1999; 10:475–479.

7. Kohlmeier L, Gasner C, Bachrach LK, Marcus R. The bone mineral status of patients with Marfan syndrome. J Bone Miner Res. 1995; 10:1550–1555.

8. Shin YL. Assessment of bone mineral density. J Korean Soc Pediatr Endocrinol. 2006; 11:123–130.
9. Lee HJ, Song BS, Kim DH, et al. Bone mineral density reference of 10-20 year-old Korean children and adolescents: based on hologic DXA from the Korean national health and nutrition examination surveys. J Korean Soc Pediatr Endocrinol. 2011; 16:92–99.

10. Oh YJ, La KS, Rhie YJ, et al. Bone mineral density and correlation factors in normal children and adolescence. J Korean Soc Pediatr Endocrinol. 2009; 14:38–44.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download