Abstract
Periprosthetic joint infection (PJI) of the hip can be difficult to treat and can lead to a number of problems including: i) severe functional decline of the hip joint and ii) increasing financial burden for patients due to long treatment periods and the need for repeated surgical interventions. Because there is risk of inadequate control of infection or relapse of a preexisting infection following the treatment of PJI through surgery, it is important to closely observe clinical symptoms such as systemic fever. Kikuchi-Fujimoto disease is usually a self-limiting disease characterized by fever and cervical lymphadenopathy. We report one case of Kikuchi-Fujimoto disease, with literatures review, that was mistaken for an infection relapse after surgical treatment of the PJI due to sustained fever postoperatively.
Accurate diagnosis of periprosthetic joint infection (PJI) serves an important role because PJI may induce functional decline of the hip joint and pose significant financial burden for patients due to enormous medical costs resulting from long-term treatment and repeat operations1). However, making an accurate diagnosis is challenging since PJI is often asymptomatic or has no definite signs of infection2). For accurate diagnosis of infection after total hip arthroplasty, thorough history taking with physical examination and diagnostic criteria suggested by the Musculoskeletal Infection Society (MSIS) using several screening tools are used and two-stage revision is generally performed as clinical management134). When patients develop fever three days following surgical treatment of the infection, orthopedic surgeons may first consider an inadequate control of the initial infection or an infection relapse and perform variable tests to determine other causes of fever5). Kikuchi-Fujimoto disease (KFD) is a rare disease characterized by fever and cervical lymphadenopathy, but also reported with various non-specific clinical manifestations. The authors experienced a case of KFD misdiagnosed as infection relapse after surgical treatment of PJI, and we report the case with a brief review of literature.
A 24-year old male Cambodian patient had a history of hemiarthroplasty using Austin Moore type unipolar prosthesis after being diagnosed with left-side hip osteoarthritis as sequelae of Legg-Calvé-Perthes disease. He visited our clinic six weeks after undergoing hemiarthroplasty due to persistent hip pain on the left side. He had no systemic symptoms (e.g., fever or signs of infection such as sinus tract formation at the surgical site) at that time. The patient had a normal peripheral white blood cell (WBC) count of 7,210/µL (reference range, 4,000-10,000/µL) with 65% neutrophils ratio (reference range, 40-74%), but had an elevated C-reactive protein (CRP) level of 2.78 mg/dL (reference range, ≤0.5 mg/dL) and erythrocyte sedimentation rate of 114 mm/hour (reference range, <15 mm/hour). Simple X-ray revealed decreased bone density around the acetabulum and femoral prosthesis area. We could not determine whether or not there was prosthetic loosening since: i) the implant position could not be compared with postoperative status because we could not get the radiographs taken immediately after surgery, and ii) femoral stem seemed to be inserted in excessive anterverted state on radiographs obtained at the time of first visit (Fig. 1). He could not afford other further workup such as computed tomographic (CT) scan or magnetic resonance image due to his financial situation.
Surgical intervention was carried out under the diagnosis of PJI according to diagnostic criteria of the MSIS, and we confirmed intra-operatively the presence of a large amount of purulent joint effusion, synovitis and inflammatory granulation tissues. Since intra-operative frozen section biopsy revealed more than 10 polymorphonuclear neutrophil, meticulous debridement and insertion of an antibiotic-loaded cement spacer for infection control was performed (Fig. 2). The result of the intra-operative culture for bacterial identification was negative.
Intravenous (IV) cefazedone, a first-generation cephalosporin antibiotic was administered postoperatively and left-side hip pain gradually subsided after operation. The patient began to complain of dorsal foot and lower back pain from two weeks after surgery, but no specific findings were shown on simple radiographs. Since additional radiologic evaluations were unattainable because of the patient’s financial situation, the patient was followed up with administration of non-steroidal anti-inflammatory drugs (NSAIDs).
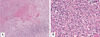
Since the patient had intermittent mild fever from the third postoperative week, we carefully monitored to determine if this was a case of reinfection or failure to control the initial infection at the surgical site; however, his clinical symptoms were not indicative of infection and CRP levels were within the normal range (0.49 mg/dL). Interdisciplinary care was conducted with the Division of Infectious Diseases due to gradual decreases in peripheral WBC count and neutrophil ratio (3,470/µL, 31.5%). IV cefazedone was replaced with vancomycin 23 days after the use of cefazedone because the patient was suspected of neutropenic fever caused by cefazedone-induced bone marrow suppression. Other oral medications were suspended including anti-inflammatory drugs and H2 blocker. However, decrease in WBC count was aggravated, high fever (above 39℃) was accompanied at four weeks and four days after surgery, and CRP gradually elevated to 4.43 mg/dL. Despite the change to vancomycin for a week, neutropenic fever persisted. Also, despite additional changes of antibiotics such as teicoplanin for another week, the use of oral cetirizine for three days followed by IV ciprofloxacin for four days, there was no improvement in symptoms. Even though the use of IV antibiotics was suspended, no improvement in fever was observed. No specific signs were found in tests performed to identify other causes for fever including blood and urine culture, sputum and stool culture, and testing for tuberculosis specific antigens. No abnormal findings were detected in echocardiography and abdominal CT. We re-evaluated the possibility of reinfection or failure of infection control at the surgical site of the left hip. CRP level was elevated, but there were no aggravation of pain and local febrile sense or erythema at the wound site. While considering re-operation for infection control due to the risk of deep infection, the patient was positive for Epstein-Barr virus (EBV), cytomegalovirus (CMV) antibody and antinuclear antibody in immune antibody screening and virus antibody screening tests. A soft tissue mass with tenderness of the upper left clavicle was detected in systemic physical exam performed to find causes for fever. Ultrasonography showed multiple cervical lymphadenopathies and a cervical lymph node biopsy revealed KFD (Fig. 3). Since symptoms became aggravated despite the use of NSAIDs, oral prednisolone (20 mg/day) was given as systemic steroid treatment. Peripheral WBC count and systemic fever improved 10 days after administration of oral prednisolone and then patient discharged. Two weeks after administration of steroid, CRP level was normalized to 0.06 mg/dL. Concurrent use of oral steroids and oral antibiotics was sustained for three months and then revision total hip arthoplasty of left hip joint was performed after one year and five months (Fig. 4).
KFD, also known as histiocytic necrotizing lymphadenitis, is a rare condition that was first described in Japan in 1972. It is a self-limiting disorder and usually appears to resolve spontaneously with no definitive treatment within six months. The symptoms of the disease gradually progress over two to three weeks after onset6). The onset period of KFD in this case was anticipated to be between the first two to three postoperative weeks when the patient complained of pain at the dorsum of the foot and lower back accompanied by a fever. KFD usually affects females under the age of 30 years and is most commonly seen in countries in East Asia, but has a worldwide distribution including Europe and the Americas67). Although the pathogenesis of KFD is unknown, it is predicted to be associated with viral infections such as EBV and CMV or auto-immune diseases such as systemic lupus erythematosus67). Common symptoms are fever, unilateral cervical lymphadenopathy, respiratory tract symptoms, leukopenia and others. Furthermore, KFD is reported to be associated with a variety of clinical manifestations including axillary or peritoneal lymphadenophathy with fever, parotid gland enlargement, skin eruption and others67). Patients with KFD may complain of musculoskeletal symptoms including myalgia and symmetric or multiple arthralgia as synovitis of peripheral joints such as hands and feet67). Previous case reports have presented with such symptoms as neck or low back pain. KFD is usually managed with observation or symptomatic management using NSAIDs; steroids could be used in severe cases6).
Orthopedic surgeons are always careful and concerned about the risk of PJI because the course of treatment is very challenging for both patients and surgeons. CRP level is an useful marker in forecasting treatment outcomes during antibiotic therapy or after surgical management of PJI18), but clinical symptoms such as pain, the surgical wound status, systemic fever and others cannot be overlooked. Most postoperative fevers are related to non-infective causes such as inflammatory cytokines (related to the development of surgery-induced tissue injury), responses to drugs or transfusion, anemia, deep vein thrombosis9). However, in cases of fever above 39℃ after three postoperative days, infection of the surgical site can be suspected and diagnostic tests need to be performed910). In this case, since a young healthy patient with no medical history underwent surgical treatment due to infection, failure to control the initial infection or infection relapse at the surgical site had been first considered as the cause of fever. However, because pain and wound status of the surgical site was favorable and there was a leukopenia on laboratory test, we considered the cause of fever as long-term use of IV antibiotics instead of infection. After being diagnosed as KFD and treated with oral steroids, the time period of improvement of symptoms was relatively short. In terms of the patient’s time and cost spent on examinations and treatment, early diagnosis would have been helpful to patient.
In summary, we initially approached this patient’s fever as failure to control the initial infection following surgical treatment for PJI or neutropenic fever due to use of IV antibiotics. Consequently, the time to detect the cervical lymphadenopathy through systemic physical exam was delayed resulting in a late diagnose of KFD following biopsy. The patient’s disease rapidly resolved after systemic steroid therapy.
Since KFD is a very rare condition characterized by non-specific musculoskeletal system symptoms, the diagnosis of KFD is often difficult for orthopedic surgeons. Moreover, because of recent increases in foreign patients, we cannot overlook the onset of the affected disease to certain racial populations or regions. A young healthy Asian female patient confirmed with cervical lymphadenopathy, fever and leukopenia can be suspected of KFD. Also, systemic fever after surgical treatment after PJI, determining the presence of infection of the surgical site is important, but identifying other possible causes of fever is also critical by performing systemic physical examination.
Figures and Tables
Fig. 1
Preoperative simple radiographs shows osteopenic bone shadows of the left acetabulum and left proximal femur around the implant. The femoral stem was seemed to be positioned with excessive anteversion.

Fig. 2
Postoperative simple anteroposterior pelvis and left hip axial radiographs of antibiotics loaded cemented implant insertion.

References
2. Savarino L, Baldini N, Tarabusi C, Pellacani A, Giunti A. Diagnosis of infection after total hip replacement. J Biomed Mater Res B Appl Biomater. 2004; 70:139–145.

3. Workgroup Convened by the Musculoskeletal Infection Society. New definition for periprosthetic joint infection. J Arthroplasty. 2011; 26:1136–1138.
4. Cho YJ, Kim KI, Chun YS, et al. Treatment of infected hip arthroplasty with antibiotic-loaded cement spacers. J Korean Hip Soc. 2009; 21:148–155.

5. Czaplicki AP, Borger JE, Politi JR, Chambers BT, Taylor BC. Evaluation of postoperative fever and leukocytosis in patients after total hip and knee arthroplasty. J Arthroplasty. 2011; 26:1387–1389.

6. Jamal AB. Kikuchi fujimoto disease. Clin Med Insights Arthritis Musculoskelet Disord. 2012; 5:63–66.

7. Kucukardali Y, Solmazgul E, Kunter E, Oncul O, Yildirim S, Kaplan M. Kikuchi-Fujimoto disease: analysis of 244 cases. Clin Rheumatol. 2007; 26:50–54.

8. Hur CR, Park CE, Hong JY, Shon WY. Change of erythrocyte sedimentation rate (ESR) and C-reactive protenin (CRP) after hip arthroplasty. J Korean Hip Soc. 2005; 17:188–194.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download