Abstract
Purpose
Cephalomedullary nail (CM nail) in the treatment of femoral intertrochanteric fractures is in the lime light in recent years. The purpose of this study is to compare surgical outcomes between experienced surgeon and non-experienced surgeons in respect of CM nail for femoral intertrochanteric fractures.
Materials and Methods
The 129 patients underwent CM nail for femoral intertrochanteric fracture more than six months of follow-up from April 2011 to March 2014 in Seoul Medical Center (Seoul, Korea) were participated in this study. For this study, group A consisted of experienced surgeons who performed more than 500 times of CM nail, and group B consisted of non-experienced surgeons who performed less than 50 times of CM nail. Clinical and radiologic outcomes, complications and the need for reoperation between both groups were compared in the study.
Results
According to clinical result, both the mean operation time and transfusion volume were significantly longer and greater in group B (P<0.05). In the radiologic outcomes, adequacy of reduction, tip-apex distance and numbers of case placed in the Cleveland zones 5, 6 and 8; there was no statistical difference between both groups. Moreover, rate of complication and reoperation had same results as radiologic outcomes.
Conclusion
There was no significant difference with statistical data in complications from CM nail for femoral intertrochanteric fractures between experienced surgeon and non-experienced surgeon. Although the operation time and transfusion volume were significantly longer and greater in the case of operation by non-experienced surgeon, satisfactory performance was seen in the complications and the need for reoperation.
Femoral intertrochanteric fractures account for a large proportion of proximal femoral fractures. This condition occurs more frequently in the elderly with osteoporosis and its incidence has been gradually increasing along with recent advances in medical technology and prolonged average life expectancy12).
Femoral intertrochanteric fractures are associated with a high rate of morbidity and complication related to prolonged bed rest. Enabling early ambulation through accurate reduction and solid fixation is important to prevent complications, and a large number of studies are further investigating optimal treatment modalities345). Cephalomedullary nail (CM nail) used for the treatment of unstable fractures serves the role of buttress to prevent medial displacement of the distal bone fragment. Subsequently, proximal femur nail (PFN), Gamma nail and others have been developed, and favorable surgical results have been achieved by providing adequate fixation567).
In recent years, CM nailing is a preferred fixation method which offers the advantages of favorable biological fixation and simple surgical procedure8910). However, this closed reduction requires proficient surgical skills in fracture reduction and fixation, and it may have a learning curve. Factors determining stability of internal fixation when treating fractures are bone quality, fragment geometry, reduction, implant selection and implant placement11). Of these, implant placement, implant selection and reduction are factors related with the operating surgeon, and surgical outcome may differ depending on skillfulness of operators. The purpose of this study was to compare surgical results between non-experienced and experienced surgeons. Furthermore, preparatory education and discussion were carried out for all operators before participating in surgery using PFN according to the treatment guidelines.
The inclusion criteria were patients who received CM nailing at Seoul Medical Center (Seoul, Korea) due to femoral intertrochanteric fractures from April 2011 to March 2014, with a minimum follow-up of six months (an average of 11.5 months). The exclusion criterion was those who died during the postoperative period before discharge. A total of 134 patients underwent surgery. Of these, 129 patients were enrolled in the study, excluding five patients who died prior to discharge or were followed up for less than six months.
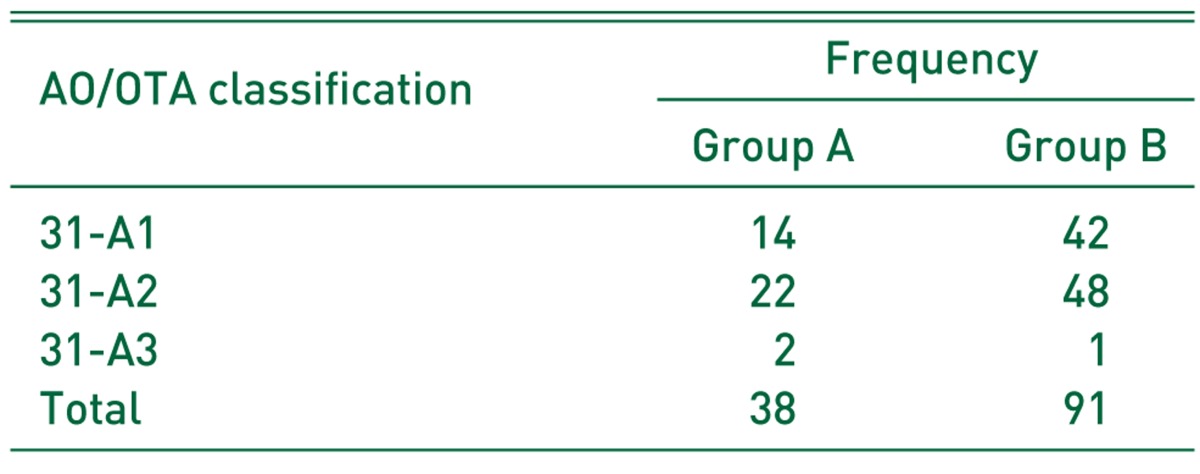
The surgical devices used were Gamma 3 nail (Stryker, Mahwah, NJ, USA) in 94 cases and intertrochanteric/subtrochanteric nail (ITST nail; Zimmer, Winterthur, Switzerland) in 35 cases, and short nails were used in all 129 patients. The AO/OTA classification was used in preoperative assessment to classify the fractures (Table 1). The shape of the medullary canal was grouped based on the Dorr classification. The patients were classified as 6 Dorr type A (4.7%), and 103 Dorr type B (79.8%) and 20 Dorr type C (15.5%)12). The American Society of Anesthesiologist (ASA) classification system was used to assess the fitness of patients, and five patients were graded as ASA grade 1, 85 as grade 2, 36 as grade 3, and three as grade 461314).
An experienced surgeon was an orthopedic surgeon who performed more than 500 times of CM nail surgery to fix intertrochanteric fractures after completing a four-year orthopedic surgery residency program and obtaining a medical license. Non-experienced surgeons were those who performed less than 50 times of CM nail surgery after completing four years of training and becoming a board certified orthopedic surgeon. All operations were conducted by a single experienced surgeon and four non-experienced surgeons. Non-experienced surgeons conducted surgery under supervision by an experienced attending surgeon, but they were not assisted.
This study was performed after gaining an approval from the Institutional Review Board of Seoul Medical Center (IRB 2015-018). The authors of the study collected plain radiographs and computed tomography scans of all patients preoperatively, immediately after surgery, and at final follow-up. We reviewed the charts based on the electronic medical records, and obtained addition information on clinical progress through telephone survey.
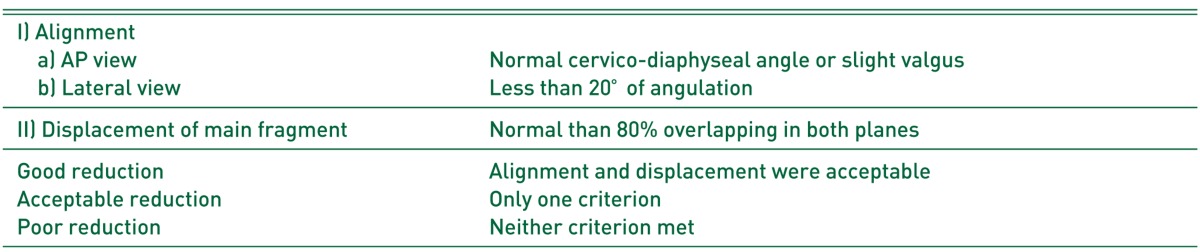
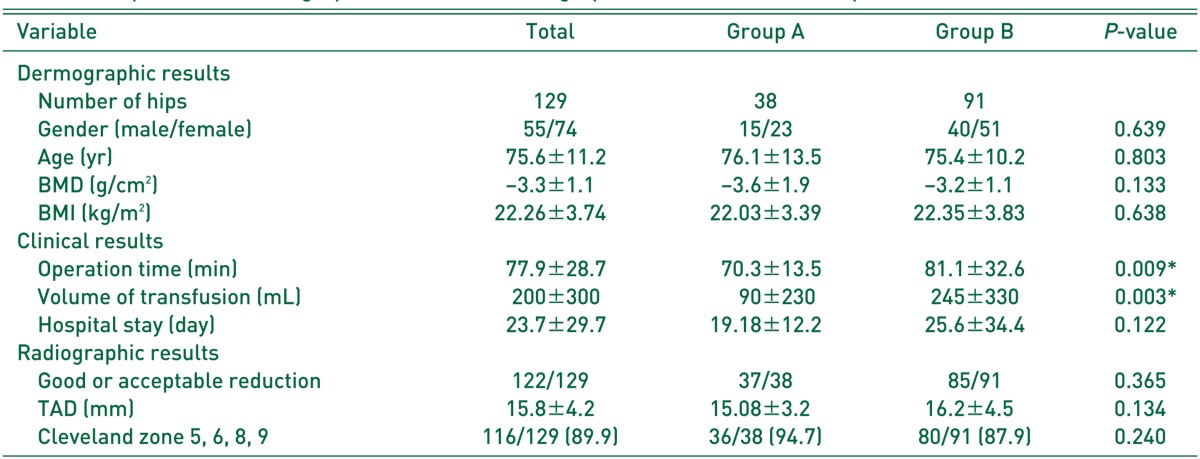
We collected patients’ demographic data (gender and age), body mass index (BMI), bone mineral density (BMD), and basic operative data (operation time, transfusion volume and others). For radiographic assessment, we evaluated adequacy of fracture reduction (Table 2) and implant site based on internal tip-apex distance (TAD) and Cleveland zone, and examined complications including fixation failure such as screw cutout and varus collapse, infection, non-union and avascular necrosis and postoperative medical problems151617). Callus formation union time of the fracture site were determined during the routine radiographic exams. Bone union was defined when callus appearance and formation of a bridge between bone fragments and trabeculae were confirmed on simple X-rays. Reoperation for any reason was considered as fixation failure, and the causes and methods of reoperation were examined.
Based on collected data, patients who received surgery by an experienced surgeon were grouped into group A (38 cases) and those by non-experienced surgeons into group B (91 cases), and clinical and radiographic results, complications and reoperation were compared between the two groups.
Surgical results were explored based on the overall statistics of 129 patients. We compared differences in demographic data, pre- and post-operative clinical and radiographic variables, complications and reoperation between group A and group B. Continuous variables were analyzed using Student t-test, categorical data, chi-square test and Fisher’s exact test. Statistical analyses were performed using PASW Statistics ver. 18.0 (IBM Co., Armonk, NY, USA). P-values of less than 0.05 were considered statistically significant.
The subjects consisted of 55 male and 74 female patients in the present study, and their mean age was 75.6 (±11.2) years. The mean BMD and BMI were −3.28 (±1.13) g/cm2 and 22.26 kg/m2, respectively. The total operation time was defined as the time from skin incision to the end of the skin closure, and the mean operation time was 77.9 (±28.7) minutes.
The average length of hospital stay was 23.7 (±29.7) days, and other blood products were not used in transfusion. Closed reduction was performed in all operations. Adequacy for reduction was 94.6% indicating good or acceptable. The mean TAD was 15.8 (±4.2) mm, and lag screws were inserted into safe zones (Cleveland zones 5, 6, 8 and 9) in 116 cases (89.9%) (Fig. 1, 2).
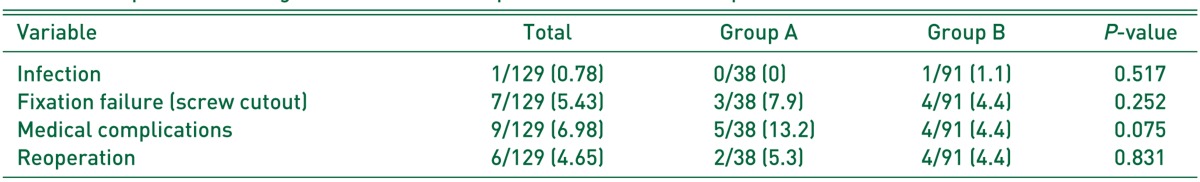
Delayed union, nonunion, infection and periprosthetic fracture were not detected in group A, and reoperation was done in two cases due to fixation failure (screw cutout) by performing conversion arthroplasty. Meanwhile, four cases underwent reoperation in group B. The causes for reoperation were fixation failure (screw cutout) in three cases treated with conversion arthroplasty and deep infection in 1 case managed with conversion arthroplasty using two-stage operation. Reoperation was planned for one case in each group due to fixation failure (screw cutout), but they refused surgical treatment because of old age, dementia and other reasons.
With respect to clinical results, the mean operation time was 70.3 (±13.5) minutes in group A and 81.1 (±32.6) minutes in group B, and the mean duration of surgery was significantly longer in group B (P<0.05). The amount of blood transfusion was 90 (±230) mL in group A and 245 (±330) mL in group B, which was significantly higher in group B than in group B (P<0.05). With respect to radiographic outcomes, adequacy of reduction was good or acceptable in 37 cases and poor in one case in group A, good or acceptable in 85 cases and poor in six cases in group B, showing no statistically significant difference. The average TAD was 15.1 mm (±3.2) in group A and 16.2 mm (± 4.5) in group B, having no statistically significant difference. Screw position in the Cleveland zones 5, 6, 8 and 9 was 36 (94.7%) cases in group A and 80 (87.9%) cases in group B, exhibiting no statistically significant difference (Table 3). In addition, no statistically significant difference was found in demographic data, radiologic data, postoperative and medical complications and reoperation (Table 4).
The CM nail is being used increasingly for femoral intertrochanteric fractures because of its advantages of biomechanical benefit and solid fixation of unstable fractures5618). Moreover, the advantages of CM nailing include less invasive procedures, small amount of blood loss, short operation time, promotion of biological healing, low infection rate and others1920). The surgical technique of CM nailing is considered a highly standardized modality and is commonly used for the purpose of training non-experience surgeons. For these reasons, orthopedic surgeons should be well acquainted with the concept and technique of CM nailing skillfully. Therefore, this study was performed to compare and examine the surgical outcomes of this procedure between experienced and non-experienced surgeons.
The results of this study revealed that no significant difference was found in operation time and transfusion volume between group A and B. Longer operation time and greater transfusion volume in operations performed by non-experienced surgeons are assumed to be attributable to different levels of experience in CM nailing procedure. Differences in levels of surgical experience appear to induce differences in operation time and blood loss volume, leading to a difference in transfusion volume. Although statistical significance was small, inappropriate screw placement was more commonly found in group B. Non-experienced surgeons had difficulty in inserting the guide pin for lag screw fixation after reduction due to lack of experience in guide pin insertion for the placement of the lag screw in safe zones of the femoral head. Repeated attempts of guide pin insertion seemed to generate differences in lag screw insertion and operation time. In a study on the learning curve of proximal femoral nail, Altintas et al.21) identified that operation time was longer in the first 15 operations performed for traning purpose compared to that of the following operations among surgeons. Likewise, they thought that operators with more experience were less likely to attempt lag screw placement in safe zones. Since insertion of the lag screw into the anterosuperior aspect of the femoral head may lead to complications such as screw cutout by inducing fixation failure, caution is warranted162223). Despite sufficient education on surgical procedures, insertion of the lag screw into the anterosuperior aspect of the femoral head occurred. Thus, in addition to acceptable reduction, careful attention should be paid to lag screw fixation during fixation among non-experienced surgeons.
There was no statistically significant difference in the rates of complication and reoperation between the two groups. This outcome is thought to be resulted from specific treatment guidelines and thorough preparatory education about acceptable reduction and fixation method. In operations such as reduction of acetabular fractures having a steep learning curve and requiring much clinical experience, satisfactory reduction was achieved after performing at least 60 times of surgery. On the contrary, satisfactory reduction was obtained in CM nail surgery performed for management of greater trochanteric fractures, despite relatively less clinical experience2124).
Of all operations conducted in our hospital, a total of six cases (4.7%) underwent reoperation due to surgical failure and eight cases (6.2%) had postoperative complications. Even though statistical analysis is challenging because of differences in study design and methods, the current study achieved satisfying results with respect to complication and reoperation rates in comparison with other previous studies252627).
The limitations of this study are as follows: First, as a retrospective study, this study had insufficiently collected and managed data. For example, a high fixation failure rate, despite high rates of acceptable reduction, is anticipated to be associated with postoperative care and patients' motor functional recovery immediately after surgery. However, hip scores were not measured at final follow-up and the degree of functional recovery was not assessed. Since, follow-up plans had not been clearly designed for every patient, the mean follow up period was short (an average of 11.5 months) and complications that could be detected in long-term follow-up were excluded. We can only predict increases in blood loss volume according to increasing operation time because accurate volumes of blood loss had not been gathered in all patients. Thus, we were unable to prove a direct relationship between blood loss volume and transfusion volume. Second, the results of this study are data gathered from five surgeons. There are possibilities that each surgeon may not have followed initial operative guidelines and may have a different approach. Despite these limitations, this investigation seems to have achieved high external validity by comprehensively interpreting surgical outcomes of several surgeons.
There was no significant difference with statistical data in complications following CM nailing for femoral intertrochanteric fractures between experienced and non-experienced surgeons. Although the operation time and transfusion volume were significantly longer and greater in operations carried out by non-experienced surgeons, satisfactory performance was seen in complications and the need for reoperation. In conclusion, CM nailing is an optimal surgical option having a high success rate regardless of surgical experience, when treatment guidelines are accurately followed and thorough preparatory education is preceded for orthopedic surgeons.
References
1. Hernández JL, Olmos JM, Alonso MA, et al. Trend in hip fracture epidemiology over a 14-year period in a Spanish population. Osteoporos Int. 2006; 17:464–470. PMID: 16283063.

2. Lönnroos E, Kautiainen H, Karppi P, et al. Increased incidence of hip fractures. A population based-study in Finland. Bone. 2006; 39:623–627. PMID: 16603427.

3. Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. Mortality risk after hip fracture. J Orthop Trauma. 2003; 17:S2–S5. PMID: 14696770.

4. Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005; 87:1123–1126. PMID: 16049251.

5. Kaplan K, Miyamoto R, Levine BR, Egol KA, Zuckerman JD. Surgical management of hip fractures: an evidence-based review of the literature. II: intertrochanteric fractures. J Am Acad Orthop Surg. 2008; 16:665–673. PMID: 18978289.

6. Sadowski C, Lübbeke A, Saudan M, Riand N, Stern R, Hoffmeyer P. Treatment of reverse oblique and transverse intertrochanteric fractures with use of an intramedullary nail or a 95 degrees screw-plate: a prospective, randomized study. J Bone Joint Surg Am. 2002; 84-A:372–381. PMID: 11886906.
7. Sung YB, Nam CH, Ahn JK, Sohn YJ, Chung HJ, Kim JH. A comparative study between the proximal femoral nail and dynamic hip screw for intertrochanteric fracture -preliminary report. J Korean Hip Soc. 2002; 14:208–215. Korean.
8. Nuber S, Schönweiss T, Rüter A. Stabilisation of unstable trochanteric femoral fractures. Dynamic hip screw (DHS) with trochanteric stabilisation plate vs. proximal femur nail (PFN). Unfallchirurg. 2003; 106:39–47. German. PMID: 12552392.
9. Yuan X, Yao Q, Ni J, Peng L, Yu D. Proximal femoral nail antirotation versus dynamic hip screw for intertrochanteric fracture in elders: a meta-analysis. Zhonghua Yi Xue Za Zhi. 2014; 94:836–839. Chinese. PMID: 24854751.
10. Kwon CS, Kim BJ, Go HS, Kim YU, Kim ES. Gamma nailing in pertrochanteric fracture of femur. J Korean Hip Soc. 1991; 3:87–93.
11. Kaufer H. Mechanics of the treatment of hip injuries. Clin Orthop Relat Res. 1980; (146):53–61. PMID: 7371269.

12. Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993; 14:231–242. PMID: 8363862.

13. Saudan M, Lübbeke A, Sadowski C, Riand N, Stern R, Hoffmeyer P. Pertrochanteric fractures: is there an advantage to an intramedullary nail?: a randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma. 2002; 16:386–393. PMID: 12142826.
14. Keats AS. The ASA classification of physical status--a recapitulation. Anesthesiology. 1978; 49:233–236. PMID: 697075.

15. Baumgaertner MR, Solberg BD. Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. J Bone Joint Surg Br. 1997; 79:969–971. PMID: 9393914.

16. Cleveland M, Bosworth DM, Thompson FR, Wilson HJ Jr, Ishizuka T. A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am. 1959; 41-A:1399–1408. PMID: 13849408.

17. Baumgaertner MR, Curtin SL, Lindskog DM. Intramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop Relat Res. 1998; (348):87–94. PMID: 9553538.

18. Wang W, Yang T, Fang Y, Wang G, Pu J, Liu L. [Treatment of reverse oblique fractures of intertrochanteric region of femur with proximal femoral nail antirotation]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2009; 23:1306–1310. Chinese. PMID: 19968168.
19. Zeng C, Wang YR, Wei J, et al. Treatment of trochanteric fractures with proximal femoral nail antirotation or dynamic hip screw systems: a meta-analysis. J Int Med Res. 2012; 40:839–851. PMID: 22906256.

20. He YQ, Ruan ZY, Xiang C, Zhang G, Zhu QW, Qian Z. Treatment of intertrochanteric fractures over age of 80 years old patients with proximal femur intramedullary nail. Zhongguo Gu Shang. 2013; 26:833–835. Chinese. PMID: 24490531.
21. Altintas B, Biber R, Bail HJ. The learning curve of proximal femoral nailing. Acta Orthop Traumatol Turc. 2014; 48:396–400. PMID: 25230261.

22. Gundle R, Gargan MF, Simpson AH. How to minimize failures of fixation of unstable intertrochanteric fractures. Injury. 1995; 26:611–614. PMID: 8550168.

23. Sommers MB, Roth C, Hall H, et al. A laboratory model to evaluate cutout resistance of implants for pertrochanteric fracture fixation. J Orthop Trauma. 2004; 18:361–368. PMID: 15213501.

25. Herrera A, Domingo LJ, Calvo A, Martínez A, Cuenca J. A comparative study of trochanteric fractures treated with the Gamma nail or the proximal femoral nail. Int Orthop. 2002; 26:365–369. PMID: 12466870.
26. Herrera A, Domingo J, Martinez A. Results of osteosynthesis with the ITST nail in fractures of the trochanteric region of the femur. Int Orthop. 2008; 32:767–772. PMID: 17618438.

27. Georgiannos D, Lampridis V, Bisbinas I. Complications following treatment of trochanteric fractures with the Gamma3 nail: Is the latest version of Gamma nail superior to its predecessor? Surg Res Pract. 2014; 2014:143598. PMID: 25374946.

Fig. 1
(A-C) Initial radiographs of a 75-year-old women shows unstable fracture (Evans type V; 31A2.2 AO/OTA), fixed with Gamma 3 nail (B and C) by experienced surgeon. Immediate postoperative anteroposter and translateral views.
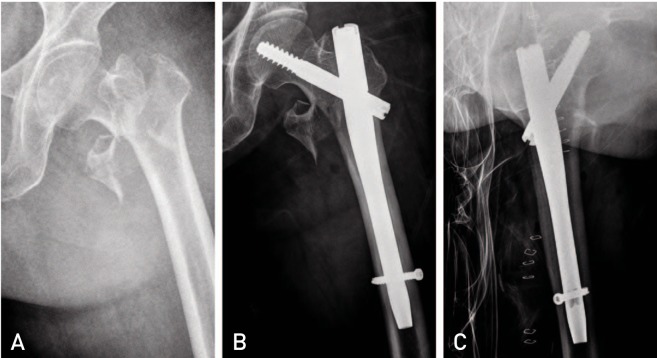
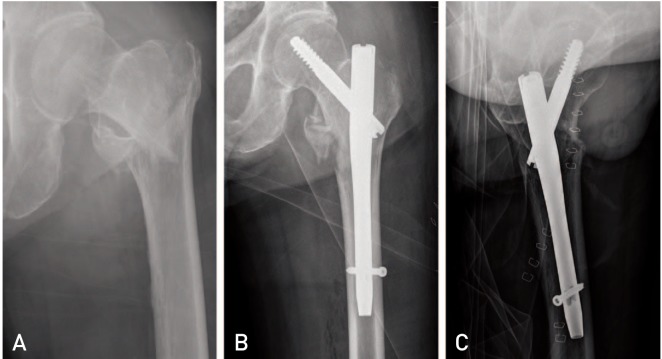
Fig. 2
(A-C) Initial radiographs of a 74-year-old man shows unstable fracture (Evans type V; 31A2.2 AO/OTA), fixed with Gamma 3 nail (B and C) by non-experienced surgeon. Immediate postoperative anteroposter and translateral views.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download