Abstract
Purpose
Preoperative on-screen templating is a method of using acetate templates on digital images. The aim of the present study was to evaluate the accuracy, intra- and interobserver reliabilities of preoperative on-screen templating using digital radiographs for total hip arthroplasty (THA).
Materials and Methods
Two hundred patients with hip disease who were treated with primary cementless THA were retrospectively evaluated. The accuracy of on-screen templating was assessed by comparing the predicted prosthesis sizes with the actual sizes used operatively. The inter- and intraobserver reliabilities of the templating results were also evaluated.
Results
The prosthesis prediction accuracy within ±one size was 96.6% for the cup size and 97.8% for the stem size. The inter- and intraobserver reliabilities for the implant size were substantial (kappa>0.70). The intra- and interobserver reliabilities for the leg length discrepancy and femoral offset difference using the intraclass correlation coefficient ranged from 0.89 to 0.97.
Preoperative templating is regarded important in orthopaedic surgery. On the basis of a review of the template and radiographs, we can decide the size and position of the implant used for our patients. Previously many authors have emphasized the importance of preoperative templating in total hip arthroplasty (THA)1234). Benefits of preoperative templating include estimation of appropriate acetabular and femoral component sizing, appropriate restoration of preoperative offset, correction of leg length discrepancy (LLD), and anticipation of special componentry or techniques5). Moreover, the survival of an implant is critically dependent on understanding the biomechanical balance and ensuring the accurate alignment of the implant6).
In former times, preoperative planning had been performed with hard copy radiographs and acetate onlay templates. Now most orthopaedic hospitals are using the picture archiving and communications systems (PACS) instead of conventional radiographs. This has resulted in traditional hard copy radiographs being unavailable for use with the standard acetate templates, and increased use of digital templating method.
Some studies have compared the accuracy of acetate templating and digital templating12789). In most of these studies, digital templating was no more accurate than acetate templating, so we performed preoperative on-screen templating using digital radiographs in order to make the best use of the advantages of acetate templating in a digital environment. In this study, we investigated the accuracy, intra- and interobserver reliabilities of preoperative on-screen templating using digital radiographs for THA. This study is based on the methodology of our previously reported study at early stage, and we intended to verify the usefulness of the on-screen templating method more reliably by making up for the weak points of the existing paper after considerable accumulation of clinical experience10).
Between April 2009 and December 2012, 413 consecutive patients with hip disease who were treated with primary cementless THA at a single institution were retrospectively evaluated. This study was approved by the Clinical Research Ethics Committee of Pusan National University Yangsan Hospital (IRB number 05-2013-047). All the THA operations were performed by one experienced arthroplasty surgeon using a posterolateral approach. We used a Trilogy acetabular cup (Zimmer, Warsaw, IN, USA) and a VerSys Fiber Metal Taper femoral stem (Zimmer) in all patients. Among these, we excluded patients who had undergone THA surgery on the contralateral hip joint, patients from whom adequate radiographs for templating could not be obtained because of improper positioning due to pain like patients with femoral neck fracture or severe deformity, and patients who had been treated with ceramic liners. In total, 200 patients (109 males and 91 females) were enrolled in our study. A mean age of patients was 56.9 years (range, 28 to 81 years; standard deviation [SD], 12.5 years). The preoperative diagnosis was osteonecrosis of the femoral head in 55.5%, degenerative osteoarthritis in 37.5%, and other diagnosis in 7.0%. Degenerative osteoarthritis patients progressed from osteonecrosis of the femoral head were classified to osteonecrosis group.
We produced the preoperative anteroposterior (AP) radiographs of both hips with the femurs rotated 15° to 20° internally. For calibration, a radiopaque bar 10 cm in length was attached to the inner aspect of the thigh, as near as possible to the pelvis. Lateral radiographs were then taken with the radiopaque bar attached to the anterior aspect of the thigh.
The AP and lateral radiographs of the hip were templated preoperatively using a single set of acetate templates for cementless THA on the 27-inch monitor. We conducted preoperative on-screen templating (Fig. 1) using a 6-step process. Step 1 was magnification of the radiographs by 120%. The size of the image was enlarged using the zoom function of PACS until the size of the radiopaque bar measured its true size of 10 cm, using the magnified ruled line scale on the templates (Fig. 2). Step 2 was measurement of the LLD. On the screen, a line was drawn across the most inferior aspect of both teardrops to meet both femurs. By measuring the distance from this line to the uppermost point of the lesser trochanters of the femur, we determined that difference as a degree of LLD. Step 3 was determination of the acetabular cup size and position on an AP radiograph of the hips. On the screen, we placed the transparent template sheet on the preoperative AP radiograph of both hips at 40° to 45° inclination, just laterally to the teardrop and just above the level of the obturator foramen. Step 4 was determination of the femoral component size and length on the lateral radiograph. We positioned femoral stem template over the normal proximal femur on lateral radiograph as proximally coated implant could be fixed compactly in the proximal femoral metaphysis. Step 5 was determination of the femoral component size and length on the AP radiograph using the same method as step 4. Finally, step 6 was determination of the femoral neck resection level and offset reconstruction (Fig. 3). Using the selected femoral stem size, the overlay template on the normal hip was used to determine the neck resection level that best permitted reproduction of the normal neck-shaft angle and offset for the patient. By moving the neck resection level in a proximal and distal direction, and with the offset possibilities of the hip system being evaluated, the offset could usually be duplicated closely. Once that was accomplished, the level of neck resection was marked on the femoral neck and was measured from the uppermost point of the lesser trochanter, and horizontal offset was measured as a perpendicular distance from the femoral axis to the center of rotation. That planned resection level was then transposed to the pathologic hip at the same femoral neck resection measured from the uppermost point of the lesser trochanter and the center of the prosthetic head was marked.
In order to assess the accuracy of preoperative on-screen templating, we compared the estimated sizes by on-screen templating with the actual sizes used operatively. We also compared the LLD and the femoral offset measured by preoperative radiographs with the LLD and the offset on postoperative radiographs. A positive LLD value was obtained when the operated limb was longer than the contralateral side while a negative value indicated the opposite. A 1-mm precision scale was used. The femoral offset ratio was calculated by dividing the offset of the operated side by the contralateral femoral offset. The femoral offset difference was defined as the value of subtracting the offset of contralateral side from that of the operated side.
One fellowship-trained orthopedic surgeon (a senior rater) performed 200 cases of on-screen templating twice, with a two-week interval, to measure the intraobserver reproducibility, and one orthopedic resident (a junior rater) assessed the same 200 radiographs. The raters who were not involved in the actual surgeries performed were blinded to the actual implants and each other's measurements. The interobserver reliability was evaluated by comparing the two surgeons' measurements.
We used a MedCalc software package (MedCalc, Mariakerke, Belgium) for statistical analysis. The interobserver reliability and intraobserver reproducibility of the prosthesis size (categorical data) were evaluated by weighted kappa. And the interobserver reliability and intraobserver reproducibility of the LLD and the femoral offset (continuous data) were evaluated by the intraclass correlation coefficient (ICC). The values were interpreted according to Landis and Koch's criteria: 0.00-0.20, slight agreement; 0.21-0.40, fair agreement; 0.41-0.60, moderate agreement; 0.61-0.80, substantial agreement; and 0.81-1.00, excellent agreement11).
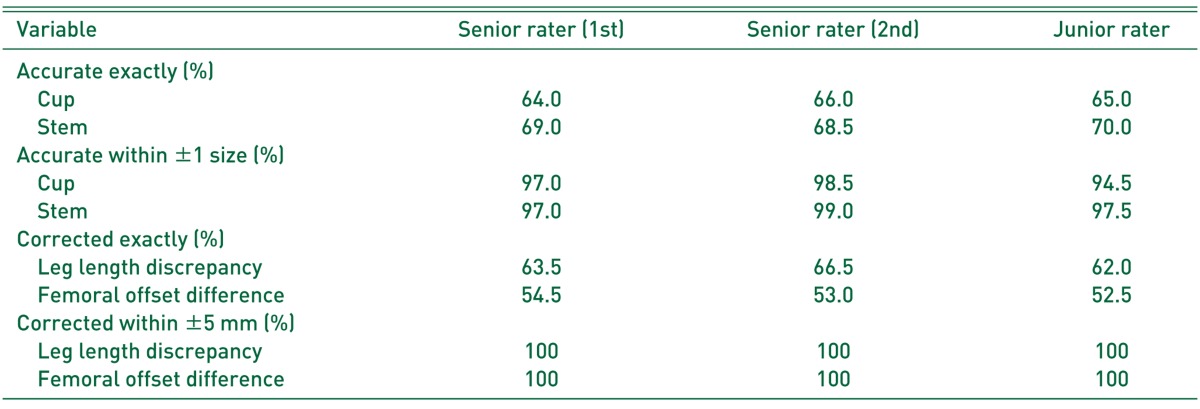
The results of the prosthesis size predictability are shown in Table 1. The exact acetabular cup size was predicted in 65.0% of cases, and a total of 96.6% of cup sizes were predicted within ±one size. For the femoral component, the exact size was predicted in 69.1% of cases, and 97.8% of stem sizes were predicted to within ±one size. The accuracy of on-screen templating by a senior rater (exactly predicted size of cup and stem, 64.0% and 69.0% of cases; within ±one size, 97.0% and 97.0%) was not always higher than that by a junior rater (exactly predicted size of cup and stem, 65.0% and 70% of cases; within ±one size, 94.5% and 97.5%) in the comparison of their first measurement results.
The results of LLD and femoral offset measurements are shown in Table 1. Preoperative LLD was exactly corrected in 64.0% of cases, and 100% of cases were corrected within ±5 mm. The femoral offset difference was exactly corrected in 53.3% of cases, and 100% were corrected within ±5 mm. The average preoperative LLD was –4.1 mm (range, –20.0 to 0.0 mm; SD, 4.5 mm), and after the operation 1.0 mm (range, –5.0 to 5.0 mm; SD, 1.8 mm). The average ratio of preoperative femoral offset was 94.2% (range, 72.0% to 122.7%; SD, 10.3%), and after the operation 100.8% (range, 88.9% to 115.6%; SD, 5.3%).
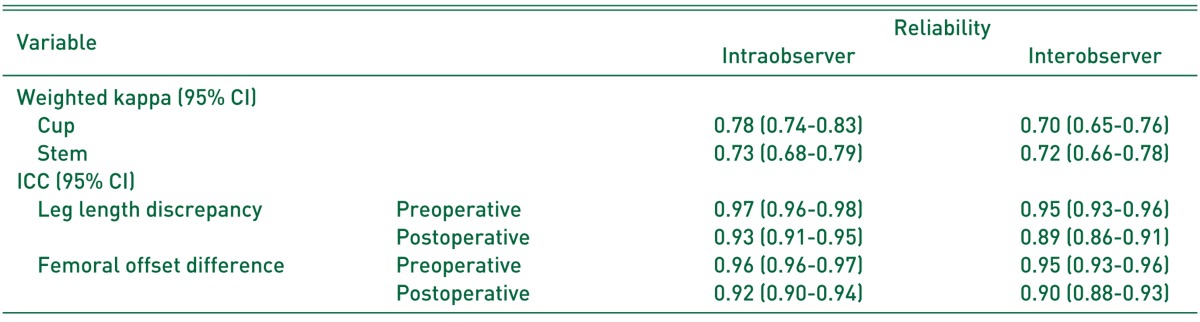
The results are shown in Table 2. The intraobserver reproducibility for the cup size and the stem size using weighted kappa statistics was 0.78 (95% confidence interval [CI], 0.74-0.83) and 0.73 (95% CI, 0.68-0.79), respectively. The interobserver reliability was also analyzed using weighted kappa statistics. The kappa was 0.70 (95% CI, 0.65-0.76) for the acetabular cup and 0.72 (95% CI, 0.66-0.78) for the femoral stem. The senior rater achieved substantial agreement for intraobserver reliability, indicating good reproducible results. Kappa values for interobserver variability between two of the observers were also substantial, indicating large agreement between these two observers.
The results are shown in Table 2. The intra- and interobserver reliability for LLD and femoral offset difference using the ICC ranged from 0.89 (95% CI, 0.86-0.91) to 0.97 (95% CI, 0.96-0.98). All the results showed good reproducibility with high ICC values (ICC >0.70), indicating good intra- and interobserver reliability.
Preoperative templating is an essential process in order to implement THA successfully. Although PACS has been used in many hospitals, preoperative templating using digital radiographs is not universal. Accordingly, we used an easy and effective on-screen templating technique for an exact preoperative templating technique in a digital environment. We aimed to investigate the accuracy and reliability of this technique in our study.
Digital radiographs have numerous advantages compared with hard-copy radiographs, including reduced radiation exposure and reduced numbers of unsatisfactory films. There are potential cost savings associated with the conversion to digital radiography. Also, the image quality of the digital radiograph is superior to that of the hard-copy radiograph. For these reasons the standardized printed films required for templating are currently being replaced by digital images that can be displayed on a PACS monitor.
After the introduction of the digital templating algorithm by Bono12), digital templating has been performed by numerous arthroplasty surgeons. But many studies comparing the accuracy of acetate templating with digital templating reported that acetate templating was more accurate than digital templating1289). And digital templating requires special software provided by the companies. As these digital templates are not commonly available, many centres have stopped templating prior to surgery. This highlights the fact that there is a need to find a more suitable option for templating; one that combines the use of digital radiographs and templating with universally available acetate templates13).
Preoperative on-screen templating methods have been described in several earlier papers1314151617). Petretta et al.17) compared acetate templating of digitally calibrated images on an liquid crystal display (LCD) monitor to digital templating in their 52 THAs, and concluded that acetate onlay templating on digitally calibrated images can be a reliable substitute for digital templating. Krishnamoorthy et al.13) also studied the accuracy and reliability of templating the acetabular cup size using conventional acetate templates on digital radiographs, and they reported 90% prediction rate for the acetabular cup size within ±1 size. In our study, we applied on-screen templating to 200 cases to investigate the availability of this method, the results showed that on-screen templating is substantial with regard to accuracy and reliability. Moreover, we proposed the use of a 27-inch monitor for its convenience. Using a 19-inch monitor screen caused visual discomfort during on-screen templating as the field of vision was too narrow. When an AP radiograph of both hips is magnified by 20%, the size of the image is too large to display in its entirety on a 19-inch monitor screen, which is most often used. For this reason, many movements of the computer mouse are needed so that other portions of the AP radiograph are visible during on-screen templating. These factors made on-screen templating cumbersome. A 20% magnified AP radiograph of both hips can show both sides of the hip joint on a 27-inch monitor screen, so a monitor screen of this size has made the on-screen templating procedure simple and easy compared with using a 19-inch monitor screen.
For accurate magnification, we used the 10-cm magnification bar provided by prosthetic manufacturer. Whiddon and Bono18) reported that the use of radiographic size markers is encouraged to mitigate potential errors, and this marker provides an easy calculation of magnification because the actual measurement will correspond with the percentage of magnification. Whereas one recent study suggested that the use of magnification marker while taking preoperative radiographs of the hip may be unnecessary, as simply setting the software to assume a 20% magnification actually was more accurate5).
Our results showed that prediction rates using on-screen templating was 96.6% for cup size within ±one size and 97.8% for stem size within ±one size. Also, we had good results in correction of LLDs and offset differences by using on-screen templating. All cases showed within 5 mm in LLDs and offset differences postoperatively. These results are substantial when comparing with the results of various studies of acetate and digital templating123478919202122232425). Although digital templating was less accurate than acetate templating in many studies, some studies reported no differences between the two templating methods, and concluded that digital templating was safe and reliable128926). But one recent study comparing acetate templating on an LCD monitor to digital templating reported the superiority of the acetate onlay templating in terms of accuracy, reproducibility and time efficiency17).
It is generally thought that the accuracy of templating is influenced by the surgeon's experience. In a previous study on acetate templating, it was reported that the accuracy of templating increased gradually with the level of training27). But in our study, both junior and senior rater showed substantial results in the predictability and reliability of on-screen templating. This result is thought to be related to the simplicity and ease of on-screen templating.
In terms of reliability, the intraobserver reliability was better than the interobserver reliability for all parameters (cup size, stem size, LLD and offset). Previously, it was recommended that the same surgeon who carries out the preoperative templating should perform the operation, because all surgeons have their own templating technique and know what works best in their cases19). This conclusion is entirely consistent with our own.
Our study has several limitations that require consideration. First, the number of observers (two for interobserver measurements) was small, which diminished the persuasive power of our study. Second, we assumed that the implanted prosthesis was always the optimal size and position, which might not have been the case. Third, the angles and reference lines were determined manually on the digital radiograph. On some radiographs, it was difficult to determine the inferior point of the teardrop figure for the horizontal reference line, so an alternative to this would be to use the interobturator, which a previous study reported as revealing the least amount of variance28). Fourth, because of no control group is present we cannot rule out the possibility that some part of the results might be associated with other factors.
Our study indicates that preoperative on-screen templating using digital radiographs is substantial in terms of its accuracy and reliability because it is a templating method that combines the advantages of acetate templating and digital radiographs. We hope that our results may encourage THA surgeons to use preoperative on-screen templating.
References
1. Crooijmans HJ, Laumen AM, van Pul C, van Mourik JB. A new digital preoperative planning method for total hip arthroplasties. Clin Orthop Relat Res. 2009; 467:909–916. PMID: 18781367.

2. Iorio R, Siegel J, Specht LM, Tilzey JF, Hartman A, Healy WL. A comparison of acetate vs digital templating for preoperative planning of total hip arthroplasty: is digital templating accurate and safe? J Arthroplasty. 2009; 24:175–179. PMID: 18534425.
3. Suh KT, Cheon SJ, Kim DW. Comparison of preoperative templating with postoperative assessment in cementless total hip arthroplasty. Acta Orthop Scand. 2004; 75:40–44. PMID: 15022804.

4. Unnanuntana A, Wagner D, Goodman SB. The accuracy of preoperative templating in cementless total hip arthroplasty. J Arthroplasty. 2009; 24:180–186. PMID: 18534455.

5. Archibeck MJ, Cummins T, Tripuraneni KR, et al. Inaccuracies in the use of magnification markers in digital hip radiographs. Clin Orthop Relat Res. 2016; 474:1812–1817. PMID: 26797909.

6. Charles MN, Bourne RB, Davey JR, Greenwald AS, Morrey BF, Rorabeck CH. Soft-tissue balancing of the hip: the role of femoral offset restoration. Instr Course Lect. 2005; 54:131–141. PMID: 15948440.
7. Gamble P, de Beer J, Petruccelli D, Winemaker M. The accuracy of digital templating in uncemented total hip arthroplasty. J Arthroplasty. 2010; 25:529–532. PMID: 19493647.

8. González Della Valle A, Comba F, Taveras N, Salvati EA. The utility and precision of analogue and digital preoperative planning for total hip arthroplasty. Int Orthop. 2008; 32:289–294. PMID: 17404731.

9. The B, Diercks RL, van Ooijen PM, van Horn JR. Comparison of analog and digital preoperative planning in total hip and knee arthroplasties. A prospective study of 173 hips and 65 total knees. Acta Orthop. 2005; 76:78–84. PMID: 15788312.
10. Kim MS, Jeong MC, Ji NG, Lee JS, Kim JI, Suh KT. Preoperative templating in PACS for total hip replacement. J Korean Orthop Assoc. 2011; 46:472–477.

11. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174. PMID: 843571.

12. Bono JV. Digital templating in total hip arthroplasty. J Bone Joint Surg Am. 2004; 86-A(Suppl 2):118–122.

13. Krishnamoorthy VP, Perumal R, Daniel AJ, Poonnoose PM. Accuracy of templating the acetabular cup size in Total Hip Replacement using conventional acetate templates on digital radiographs. J Clin Orthop Trauma. 2015; 6:215–219. PMID: 26566332.

14. Berstock JR, Webb JC, Spencer RF. A comparison of digital and manual templating using PACS images. Ann R Coll Surg Engl. 2010; 92:73–74. PMID: 20056068.

15. Meyer C, Kotecha A, Richards O, Isbister E. Acetate templating for total hip arthroplasty using PACS. Ann R Coll Surg Engl. 2009; 91:162–163. PMID: 19317940.

16. Oddy MJ, Jones MJ, Pendegrass CJ, Pilling JR, Wimhurst JA. Assessment of reproducibility and accuracy in templating hybrid total hip arthroplasty using digital radiographs. J Bone Joint Surg Br. 2006; 88:581–585. PMID: 16645101.

17. Petretta R, Strelzow J, Ohly NE, Misur P, Masri BA. Acetate templating on digital images is more accurate than computer-based templating for total hip arthroplasty. Clin Orthop Relat Res. 2015; 473:3752–3759. PMID: 25910779.

18. Whiddon DR, Bono JV. Digital templating in total hip arthroplasty. Instr Course Lect. 2008; 57:273–279. PMID: 18399591.
19. Bertz A, Indrekvam K, Ahmed M, Englund E, Sayed-Noor AS. Validity and reliability of preoperative templating in total hip arthroplasty using a digital templating system. Skeletal Radiol. 2012; 41:1245–1249. PMID: 22588597.

20. Davila JA, Kransdorf MJ, Duffy GP. Surgical planning of total hip arthroplasty: accuracy of computer-assisted EndoMap software in predicting component size. Skeletal Radiol. 2006; 35:390–393. PMID: 16572344.

21. Eggli S, Pisan M, Müller ME. The value of preoperative planning for total hip arthroplasty. J Bone Joint Surg Br. 1998; 80:382–390. PMID: 9619923.

22. Knight JL, Atwater RD. Preoperative planning for total hip arthroplasty. Quantitating its utility and precision. J Arthroplasty. 1992; 7(Suppl):403–409. PMID: 1431923.
23. Kumar PG, Kirmani SJ, Humberg H, Kavarthapu V, Li P. Reproducibility and accuracy of templating uncemented THA with digital radiographic and digital TraumaCad templating software. Orthopedics. 2009; 32:815. PMID: 19902895.

24. Shaarani SR, McHugh G, Collins DA. Accuracy of digital preoperative templating in 100 consecutive uncemented total hip arthroplasties: a single surgeon series. J Arthroplasty. 2013; 28:331–337. PMID: 22854351.
25. Steinberg EL, Shasha N, Menahem A, Dekel S. Preoperative planning of total hip replacement using the TraumaCad™ system. Arch Orthop Trauma Surg. 2010; 130:1429–1432. PMID: 20069428.

26. Bracey DN, Seyler TM, Shields JS, Leng X, Jinnah RH, Lang JE. A comparison of acetate and digital templating for hip resurfacing. Am J Orthop (Belle Mead NJ). 2014; 43:E19–E24. PMID: 24490189.
27. Carter LW, Stovall DO, Young TR. Determination of accuracy of preoperative templating of noncemented femoral prostheses. J Arthroplasty. 1995; 10:507–513. PMID: 8523011.

28. Tripuraneni KR, Archibeck MJ, Junick DW, Carothers JT, White RE. Common errors in the execution of preoperative templating for primary total hip arthroplasty. J Arthroplasty. 2010; 25:1235–1239. PMID: 20022456.

Fig. 1
Preoperative on-screen templating is a method to use acetate template on digital radiographs.
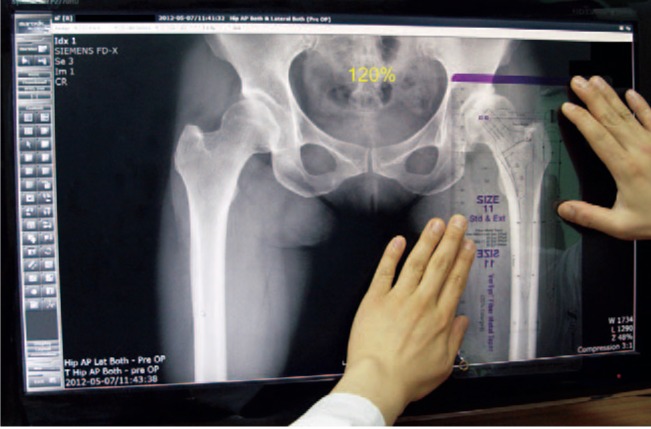
Fig. 2
The size of this image was 48% enlarged using the zoom function of the picture archiving and communications system (PACS), so the size of the radiopaque bar was measured its true size of 10 cm, using the magnified ruled line scale on the templates.

Fig. 3
The final step of the on-screen templating process is determination of the femoral neck resection level and the offset reconstruction. The femoral head center of the femoral template is placed 5 mm higher than the marked center of the acetabular template to restore the leg length.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download