Abstract
Purpose
This study aimed to investigate the outcomes of modular neck-utilization in primary total hip arthroplasty (THA).
Materials and Methods
Thirty patients (34 hips) who had modular stem THA between April 2011 and January 2013 were evaluated. There were 19 men and 11 women with a mean age of 61.2 years at the time of surgery. There were 20 cases of osteonecrosis of femoral head, 7 cases of osteoarthritis, 6 cases of femur neck fracture, and 1 case of rheumatoid arthritis. No patients presented with anatomical deformity of hip. Patients were operated on using a modified Watson-Jones anterolateral approach. All patients underwent clinical and radiological follow-up at 6 weeks, 3, 6, and 12 months, and every year postoperatively. The mean duration of follow-up was 48.2 months (range, 39 to 59 months).
Results
The average Harris hip score improved from 63.7 to 88.1 at the final follow-up. Radiographically, mean acetabular cup inclination was 45.3°(range, 36°-61°) and anteversion was 21.7°(range, 11°-29°). All were neutral-positioned stems except 5 which were varus-positioned stems. In only 3 cases (8.8%), varus or valgus necks were required. A case of linear femoral fracture occurred intraoperatively and 1 case of dislocation occurred at postoperative 2 weeks. No complications at modular junction were occurred.
The use of a modular neck in total hip arthroplasty (THA) was first introduced by Toni et al.1) in 2001. Compared to conventional single neck-head taper or monolithic design, the modular neck system is a beneficial choice in cases with anatomical variations as it allows for increased intraoperative flexibility through more independent control over leg length, femoral offset and femoral version2). Moreover, a modular neck allows changes of the neck without the removal of well-fixed stems in revision surgery2). On the other hand, disadvantages have been identified when using modular necks including corrosion, metallosis3), modular neck fracture4) and others at the second taper junction. This study aimed to investigate the need for and radiological and clinical outcomes of modular necks in primary THA.
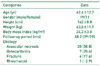
This study was approved by our institutional review board. This study retrospectively reviewed 30 patients (34 cases) who could be followed up for a minimum of three years after undergoing primary THA using a modular neck from April 2011 to January 2013. The mean postoperative follow-up was 48.2 months (range, 39-59 months). The mean age at the time of surgery was 62.4±12.7 years. The subjects were 19 men (23 cases) and 11 women (11 cases). The demographic data for patients are shown in Table 1. No patients had anatomical deformities such as acetabular dysplasia, deformity of the proximal femur and others.
The implants used were the M/L Taper Prosthesis with Kinectiv® Technology (Zimmer, Warsaw, IN, USA) (Fig. 1) as femoral stems and the Continuum® Acetabular System (Zimmer) as acetabular cup components in all cases.
Ceramic-on-ceramic bearings were used in 15 cases, and ceramic-on-polyethylene bearings were used in 9 cases. The head sizes were 32 mm in 14 cases, and 36 mm in 16 cases. All surgical procedures were performed by a single surgeon using an anterolateral (modified Watson-Jones) approach.
The size of the femoral component was predicted by overlaying a template on anteroposterior (AP) radiographs to determine whether the body of femoral component can fill the femoral metaphysis. The medial portion of the body of the component was made to fit the medial cortex of the proximal metaphysis as full as possible. After deciding the height of the femoral component, the length and offset of the neck component were determined according to the center of rotation.
After preoperative templating and intraoperative trial reduction, modular neck selection was finally determined by checking hip joint range of motion (ROM), leg length and soft tissue tension. During the trial, necks with impingement or dislocation were replaced. The version angle of the modular neck used was straight in all cases; anteverted or retroverted necks were not used. A standard offset neck was used in 31 hips (91.2%), a varus or valgus neck was required in 3 hips (8.8%), including a varus neck in 2 and a valgus neck in 1 (Fig. 2). Partial weight bearing walking was begun on the second postoperative day, and walker or crutch walking was carried out for 4 weeks after surgery.
All patients underwent clinical and radiological follow-up at 6 weeks, 3, 6, and 12 months, and every year postoperatively. Clinical results were measured using the Harris hip scores (HHS)5) at each follow-up. Pain, febrile sense, swelling, fullness and soft tissue mass at the surgical site were identified. In radiographic analysis, AP view and translateral view of the operated hip were checked. Periprosthetic proximal femoral osteolysis caused by corrosion was examined in Gruen zones 1 and 76).
On the final follow-up radiographs, the position, stability and leg length discrepancy of cup and stem components were checked. The stability of femoral stems were classified according to the criteria described by Engh et al.7), and acetabular cup inclination and anteversion were evaluated using measurements established by Woo and Morrey8). The angles of the femoral stem greater than 5°were considered varus or valgus positions. Leg length discrepancy was defined as the difference between the distances from horizontal interischial line to the greater trochanter. At the first month postoperatively, laboratory tests of inflammatory profiles, including erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and white blood cell count (WBC) were evaluated.
HHS improved from an average 64.0±9.5 points to 88.7±6.3 points in 24 patients, excluding 6 patients with a femur neck fracture (P=0.000). Pain, febrile sense, swelling, fullness and soft tissue mass and other complications at the surgical site were not observed during follow-up. During follow-up periods, radiolucency of more than 2 mm manifesting proximal periprosthetic femoral osteolysis was not seen on radiographs. At the final follow-up, the mean lateral inclination of the acetabular cup was 45.3°(36°-61°) and the mean anteversion was 21.7°(11°-29°) on radiographs. Femoral stems were inserted in a neutral position (29 hips) and a varus position (5 cases). The stability of femoral components was graded as bony stable (31 hips) and fibrous stable (3 hips). Unstable fixation was not observed. Leg length discrepancy with the contralateral side was less than 5 mm in 31 hips (91.2%) and greater than 5 mm in 3 hips (8.8%) (Table 2). At the first month postoperatively, ESR, CRP and WBC values were within the normal range (Table 3).
Additional wiring was done in one patient case due to femur crack, an intraoperative complication, during stem insertion, and bone union was achieved during follow up. Although dislocation, a complication developed on the second postoperative week, occurred in a patient, this complication did not recur after reduction. Implant revision was not conducted till the end of the final follow-up. Revision-free survival was 100% at a maximum follow-up of 59 months.
The use of a modular neck in THA has been found to reduce postoperative dislocation, a serious complication, by allowing intraoperative adjustment of length, version and offset910). However, numerous studies have reported modular neck fracture and mechanical failure as a second taper junction serves as an additional site for failure1112131415161718). Furthermore, the occurrence of local, systemic metallic debris and increase in metallic ions are problematic clinically, and these seem to cause fretting and crevice corrosion at the modular neck-stem junction and head-neck junction1920). More severe fretting and crevice corrosion at the neck-stem junction appear to be attributable to the eccentric load that leads to increased stress on the neck-stem connection, while the forces at the head-neck connection are transmitted through the spherical bearing resulting in relatively lower stresses221). Favorable outcomes have been addressed in several long-term follow-up studies on THA performed using S-ROM (Depuy, Warsaw, IN, USA), a device consisting of titanium-titanium junction2223). Moreover, good clinical results have been achieved in studies on THA conducted with devices composed of titanium-titanium neck-stem junction24). On the contrary, De Martino et al.25) have reported corrosion at the neck-stem taper in all 60 cases retrieved after undergoing THA with cobalt-chromium alloy neck segment and titanium-alloy femoral stem components.
In the retrieval analysis of 7 different types of modular total hip designs, Kop et al.21) observed severe corrosion and fretting in cobalt-chromium alloy devices and mild corrosion in titanium alloy devices in 57 cases.
In the present study, the reason for no complications associated with corrosion seems to be the use of devices consisting of titanium-titanium neck-stem junction with corrosion resistance properties.
In retrieval studies of Kop et al.21), De Martino et al.25), and Lanting et al.26), the average time to revision surgery due to corrosion or periprosthetic fracture was 12, 21.4, and 20.4 months, respectively. In this investigation, the mean duration of postoperative follow-up was 48.2 months, sufficient enough to observe complications in the modular junction.
In cases requiring revision due to adverse local tissue reaction or periprosthetic fractures, symptoms were found to be associated in 80% according to De Martino et al.25) and 100% according to Lanting et al26). In the current study, there were no laboratory findings or symptoms suspected of adverse local tissue reaction caused by corrosion. Even though Archibeck et al.27) and Sariali et al.28) have proposed that the use of modular stems in THA is beneficial in restoration of hip geometry, Gerhardt et al.29) have suggested no clear benefit. The benefit of the modular neck system for hip geometry restoration still remains uncertain.
Although the authors decided femoral stems through preoperative templating in hips with without anatomical deformity, we experienced intraoperative dislocation, leg lengths discrepancy and impingement in some cases. The main reason that we used modular necks was to resolve these clinical problems by increasing intraoperative flexibility even in hips with normal anatomy. Modular necks were finally chosen by comprehensively considering hip ROM, leg length, and soft tissue tension after intraoperative trial reduction.
Our study used two varus necks and a valgus neck, and these neck components were selected intraoperatively to optimize leg length without affecting offset. The HHS improved in all three cases after surgery without any complication. Taking into consideration the fact that varus or valgus necks were used in 8.8% of cases, the effectiveness of the modular neck is partially expected in normal anatomical hip.
This study was limited in certain aspects. First, no comparative analysis was done with the group that underwent surgery using monoblock stems instead of modular necks. This retrospective study was limited by the relatively small sample size and short follow-up period. Additional studies with a larger sample size are warranted to further identify factors that influence postoperative outcomes through long-term follow-up and explore the occurrence of complications. In addition, we did not measure serial metal ion levels necessary to quantitatively analyze corrosion.
Figures and Tables
 | Fig. 1(A) M/L taper with Kinectiv® (Zimmer, Warsaw, IN, USA) is shown. (B) Kinectiv® neck provisional tray is shown. |
 | Fig. 2(A) Hip anteroposterior (AP) radiograph of 62 years old male patient implanted with a valgus neck. (B) Hip AP radiograph of 56 years old male patient implanted with a varus neck. |
References
1. Toni A, Sudanese A, Paderni S, et al. Cementless hip arthroplasty with a modular neck. Chir Organi Mov. 2001; 86:73–85.
2. Dunbar MJ. The proximal modular neck in THA: a bridge too far: affirms. Orthopedics. 2010; 33:640.

3. Gill IP, Webb J, Sloan K, Beaver RJ. Corrosion at the neck-stem junction as a cause of metal ion release and pseudotumour formation. J Bone Joint Surg Br. 2012; 94:895–900.

4. Murugappan KS, Graves S. Outcome after modular neck hip arthroplasty: lessons from the registry. J Bone Joint Surg Br. 2012; 94-B SUPP XLI:112.
5. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51:737–755.

6. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; (141):17–27.
7. Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990; (257):107–128.

8. Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982; 64:1295–1306.

9. Berry DJ, von Knoch M, Schleck CD, Harmsen WS. The cumulative long-term risk of dislocation after primary Charnley total hip arthroplasty. J Bone Joint Surg Am. 2004; 86-A:9–14.

10. Collier JP, Mayor MB, Williams IR, Surprenant VA, Surprenant HP, Currier BH. The tradeoffs associated with modular hip prostheses. Clin Orthop Relat Res. 1995; (311):91–101.
11. Atwood SA, Patten EW, Bozic KJ, Pruitt LA, Ries MD. Corrosion-induced fracture of a double-modular hip prosthesis: a case report. J Bone Joint Surg Am. 2010; 92:1522–1525.
12. Garbuz DS, Tanzer M, Greidanus NV, Masri BA, Duncan CP. The John Charnley Award: Metal-on-metal hip resurfacing versus large-diameter head metal-on-metal total hip arthroplasty: a randomized clinical trial. Clin Orthop Relat Res. 2010; 468:318–325.

13. Sporer SM, DellaValle C, Jacobs J, Wimmer M. A case of disassociation of a modular femoral neck trunion after total hip arthroplasty. J Arthroplasty. 2006; 21:918–921.

14. Sotereanos NG, Sauber TJ, Tupis TT. Modular femoral neck fracture after primary total hip arthroplasty. J Arthroplasty. 2013; 28:196.e7–196.e9.

15. Ellman MB, Levine BR. Fracture of the modular femoral neck component in total hip arthroplasty. J Arthroplasty. 2013; 28:196.e1–196.e5.

16. Skendzel JG, Blaha JD, Urquhart AG. Total hip arthroplasty modular neck failure. J Arthroplasty. 2011; 26:338.e1–338.e4.

17. Wilson DA, Dunbar MJ, Amirault JD, Farhat Z. Early failure of a modular femoral neck total hip arthroplasty component: a case report. J Bone Joint Surg Am. 2010; 92:1514–1517.

18. Dangles CJ, Altstetter CJ. Failure of the modular neck in a total hip arthroplasty. J Arthroplasty. 2010; 25:1169.e5–1169.e7.

19. Jacobs JJ, Skipor AK, Patterson LM, et al. Metal release in patients who have had a primary total hip arthroplasty. A prospective, controlled, longitudinal study. J Bone Joint Surg Am. 1998; 80:1447–1458.

20. Willert HG, Buchhorn GH, Fayyazi A, et al. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am. 2005; 87:28–36.

21. Kop AM, Keogh C, Swarts E. Proximal component modularity in THA--at what cost? An implant retrieval study. Clin Orthop Relat Res. 2012; 470:1885–1894.

22. Imbuldeniya AM, Walter WK, Zicat BA, Walter WL. The S-ROM hydroxyapatite proximally-coated modular femoral stem in revision hip replacement: results of 397 hips at a minimum ten-year follow-up. Bone Joint J. 2014; 96-B:730–736.
23. Tanzer M, Chan S, Brooks CE, Bobyn JD. Primary cementless total hip arthroplasty using a modular femoral component: a minimum 6-year follow-up. J Arthroplasty. 2001; 16:8 Suppl 1. 64–70.

24. Ollivier M, Parratte S, Galland A, Lunebourg A, Flecher X, Argenson JN. Titanium-titanium modular neck for primary THA. Result of a prospective series of 170 cemented THA with a minimum follow-up of 5 years. Orthop Traumatol Surg Res. 2015; 101:137–142.

25. De Martino I, Assini JB, Elpers ME, Wright TM, Westrich GH. Corrosion and fretting of a modular hip system: a retrieval analysis of 60 rejuvenate stems. J Arthroplasty. 2015; 30:1470–1475.

26. Lanting BA, Teeter MG, Vasarhelyi EM, Ivanov TG, Howard JL, Naudie DD. Correlation of corrosion and biomechanics in the retrieval of a single modular neck total hip arthroplasty design: modular neck total hip arthroplasty system. J Arthroplasty. 2015; 30:135–140.

27. Archibeck MJ, Cummins T, Carothers J, Junick DW, White RE Jr. A comparison of two implant systems in restoration of hip geometry in arthroplasty. Clin Orthop Relat Res. 2011; 469:443–446.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download