Abstract
Purpose
We investigated the incidence and time of dislocation and other factors associated with dislocation of bipolar hemiarthroplasty related to the treatment of femoral neck fracture in old age patients.
Materials and Methods
Between January 2002 and April 2014, 498 femoral neck fractures (467 patients) were treated with bipolar hemiarthroplasty and included in this study. All surgeries were performed using the postero-lateral approach. The incidence of dislocation was investigated. A comparative analysis between a control group and dislocation group was performed with respect to patient factors including age, gender, body mass index, comorbidities, the ASA (American Society of Anesthesiologists) score, mental status and center-edge angle, and surgical factors including type of femoral stem, leg length discrepancy, femoral offset and method of short external rotator (SER) reconstruction.
Results
The incidence of dislocation was 3.8%, and the dislocation occurred on average 2.2 months (range, 0.6-6.5 months) after operation. No difference in patient-related factors was observed between the two groups. However, a smaller center edge (CE) angle was observed in the dislocation group (42.1°±3.2° vs. 46.9°±5.4°, P<0.001), and significantly lower incidence of dislocation was observed in tendon to bone repair group (0.7% vs 7.8%, P<0.001).
Conclusion
SERs should be repaired using the tendon-to-bone repair method to reduce dislocation rate in elderly patients who undergo bipolar hemiarthroplasty using the postero-lateral approach due to femoral neck fracture. In addition, patients with smaller CE angle should be carefully monitored due to high incidence of dislocation.
The incidence rate of hip fractures shows an increasing trend along with increase in average life span and social activities in elderly patients. Even a minor injury can result in hip fractures in older people and patients with underlying medical conditions are known to have higher mortality rates after hip fractures12). Therefore, the goal of hip fracture management in elderly patients is recovering their ability to perform daily activities as soon as possible after fracture by minimizing complications; bipolar hemiarthroplasty is commonly performed for elderly patients with femoral neck fracture.
Dislocation is one of the most serious complications following total hip arthroplasty (THA). Risk factors for dislocation can be patient related or surgery related. Patient-related risk factors are abductor muscle weakness, deformity of hip joint and general neurological problems, while surgical-related risk factors are prosthetic problems, different surgical approaches and others3). Although the postero-lateral approach is a commonly used technique and considered an easy procedure with minimal blood loss and less damage to the hip abductor, this approach is more prone to dislocation than the anterior approach45). In order to reduce dislocation rates, secure reconstruction of posterior soft tissues and joint capsule should be emphasized678). Recent studies have been conducted to verify the risk factors of dislocation as femoral offset; leg length discrepancy and acetabular center edge (CE) angle have been identified as causes. Mukka et al.9) observed a higher dislocation rate due to decreased soft-tissue tension resulting from a short femoral offset and limb length shortening, and reported a small CE angle indicating a shallow acetabulum as a risk factor for dislocation. Furthermore, Madanat et al.10) and Ninh et al.11) also studied short femoral offset and a small CE angle as potential factors for dislocation.
Nevertheless, dislocation following bipolar hemiarthroplasty remains a consistent occurrence. Even though its incidence is lower than that of THA1213), this can increase readmission rates of patients, result in revision and cause a rise in prevalence and mortality rates of patients. In particular, dislocation after bipolar hemiarthroplasty can increase prevalence and mortality rates of elderly patients14).
We aimed to investigate the incidence and time of dislocation and risk factors associated with dislocation following bipolar hemiarthroplasty for the treatment of femoral neck fracture in elderly patients.
This study was approved from the institution review board of Hanyang University Hospital (HYUH 2014-12-022-001). All data for this study were retrieved from our institution's database.
Between January 2002 and April 2014, 519 patients were treated with bipolar hemiarthroplasty due to femoral neck fractures and had a minimum follow-up of one year. A total of 498 femoral neck fractures (467 patients) were finally enrolled in this study, excluding 30 cases treated with approaches other than the postero-lateral approach; 17 with a history of hip surgery, and 5 with pathological fracture secondary to underlying disease. Of the 467 subjects, 114 were men and 353 were women. The mean age at the time of surgery was 75.9 years old (range, 71-98 years), and the mean duration of follow-up was 2.6 years (range, 1.2-10.3 years). Cementless femoral stems were used in all surgeries, and the cementless prostheses used were SL-Plus® (Smith & Nephew, Memphis, TN, USA) in 385 cases and Accolade®(Stryker, Cork, Ireland) in 113 (Table 1).
All hip arthroplasties were performed in a lateral position by two surgeons. In all cases, the short external rotator (SER) tendons were separated including the piriformis muscles, and the quadratus femoris muscles were separated when the lower femoral neck needed to be exposed. SER tendon and posterior joint capsule were sutured using modified Kessler's method with 1-0 Ethibond. The surgical site was fixed in abduction for three postoperative days, and patients were put on bed rest. Partial weight bearing was begun by using crutches or wheelchair on the first postoperative week, and full weight-bearing was started in the fourth week after surgery. Until the 8th postoperative week, patients were instructed to avoid excessive hip movement and flexion greater than 90° or external and internal rotation greater than 45°. Age, gender, body mass index (BMI), American Society of Anesthesiologists (ASA) classification, mental illnesses such as dementia and delirium and others were reviewed retrospectively as dislocation-related patient factors based on medical records. Dementia was examined by reviewing a history of diagnosis in our hospital or other institutions based on medical records, and the risk of anesthesia was assessed according to patient physical status at the time of admission. ASA scores were classified into Grade I (healthy), Grade II (mild systemic disease), Grade III (moderate systemic disease), and Grade IV (severe systemic disease).
The type of femoral stem was examined as a surgical factor, and femoral offset, leg length discrepancy, and acetabular CE angle were measured using the immediate postoperative anteroposterior radiographs of the hip. Femoral offset was defined as the sum of the distance between the center of the femoral head to the longitudinal axis of the femur plus the perpendicular distance passing through the medial margin of the ipsilateral teardrop point. The affected and healthy sides were compared (Fig. 1). Leg length discrepancy was defined as the difference in the distance between a line passing through the lower edge of the teardrop points to the corresponding tip of the lesser trochanter (Fig. 2). CE angle was defined as the angle between the center of the bipolar cup and the lateral edge of the acetabulum (Fig. 3). All measurement was made by a surgeon who did not perform the actual surgery. In addition to radiologic findings, SER repair method was examined as a surgical factor. The separated SER tendons were fixed through a 2-mm drill hole in the greater trochanter in tendon-to-bone repair group, while the separated SER tendons were directly sutured to the gluteus medius tendon in the tendon-to-bone group.
In regards to the above variables, patient factors and surgical factors were compared between the dislocation group with dislocation occurring during follow-up and a control group with no dislocation. Continuous variables such as age, BMI, and radiological measurements were analyzed using the Student's t-test, and categorical variables including gender and mental symptoms such as dementia or delirium were compared using the chi-square test. Statistical analyses were performed using IBM SPSS Statistics software (version 21.0; IBM Co., Armonk, NY, USA), and differences were considered statistically significant at P<0.05.
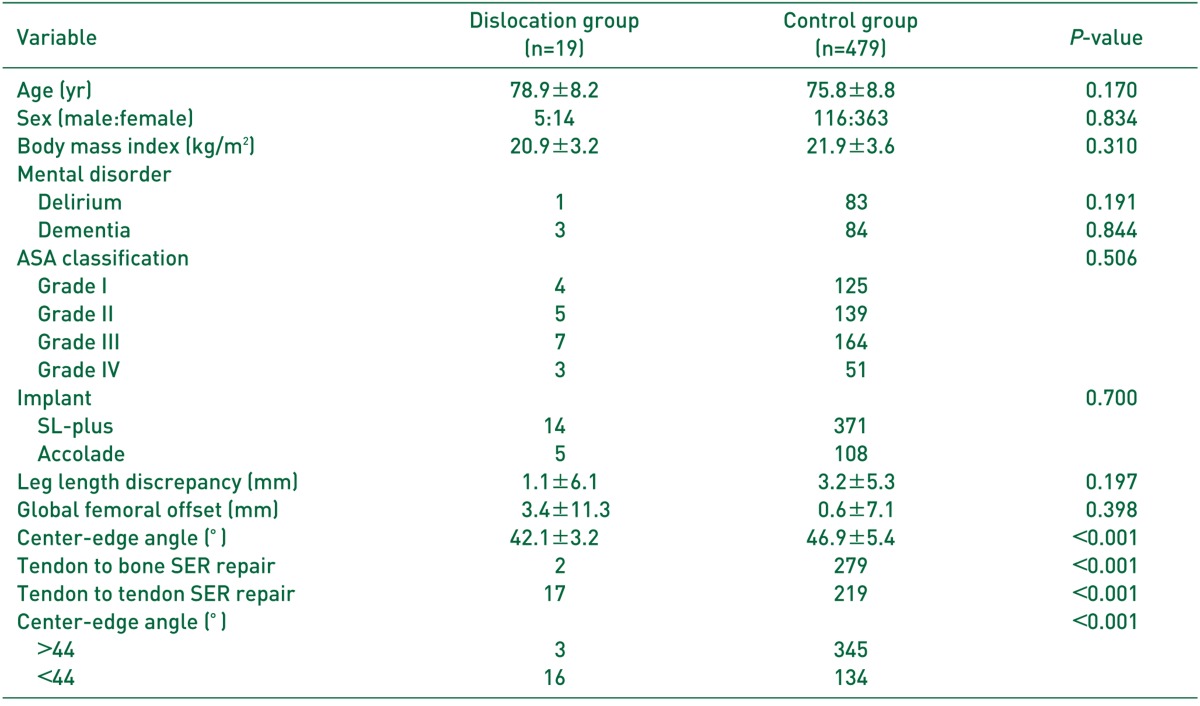
Among 498 cases with bipolar hemiarthroplasty, dislocation occurred in 19 cases (3.8%) during follow-up and all dislocations were posterior. The mean time from surgery to the first dislocation was 2.2 months (range, 0.6-6.5 months), and dislocation occurred within the first three months after surgery with the exception of 2 cases. Of all 19 dislocation cases, 5 were male and 14 were female (P=0.834). The mean age was 78.9±8.2 years in the dislocation group and 75.8±8.8 years in the control group, exhibiting no difference between the two groups. The mean BMI was 20.9±3.2 kg/m2 in dislocation group and 21.9±3.6 kg/m2 in control group, showing no statistically significant difference (P=0.310). The number of patients with delirium and dementia were 1 and 3, respectively, in the dislocation group and 83 and 84, respectively, in the control group (P=0.191, P=0.844). According to the ASA classification, the risk assessment of anesthesia was Grade I, in 4 patients, Grade II in 5 patients, Grade III in 7 patients and Grade IV in 3 patients within the dislocation group, and Grade I in 125 patients, Grade II in 139 patients, Grade III in 164 patients and Grade IV in 51 patients within the control group, showing no significant difference between the two groups (P=0.506). No difference was observed in the type of femoral stem used (P=0.700) (Table 2).
Based on radiologic examinations, leg length discrepancy was 1.1 mm between the affected side and the healthy side in the dislocation group and 3.2 mm in the control group, but no statistically significant difference was found between the two groups (P=0.197). The difference in femoral offset was 3.4 mm in the dislocation group, and 0.6 mm in the control group, exhibiting no statistically significant difference between the two groups (P=0.398). On the contrary, the average CE angle was 42.1°±3.2° in the dislocation group and 46.9°±5.4° in the control group, showing a significant difference between the two groups (P<0.001) (Table 2). Defining dislocation as the existence of a CE angle greater than 44° had a sensitivity of 81.3% and a specificity of 76.0%. Among 348 cases with a CE angle greater than 44°, dislocation occurred in 3 cases (0.9%). Among 150 cases with a CE angle less than 44°, dislocation occurred in 16 (10.7%), showing a significant difference between the two groups (P<0.001). According to SER repair methods, tendon-to-bone repair was performed in 279 cases and dislocation occurred in 2 (0.7%) while, tendon-to-bone repair was conducted in 219 cases and dislocation occurred in 17 (7.8%). There was a significant difference between the two groups (P<0.001) (Table 2). To manage dislocation, close reduction was done in 18 cases with a first-time dislocation, and all patients were instructed to wear a hip abduction brace for 6 weeks postoperatively and to avoid hip flexion greater than 90°. There was no recurrence of dislocation thereafter (Fig. 4). However, a case had 5 recurrent dislocations and treated with revision using constrained acetabular components.
This study investigated the incidence and time of dislocation and risk factors associated with dislocation following bipolar hemiarthroplasty in elderly patients with femoral neck fractures. The incidence of dislocation was 3.8%, and the mean onset time of dislocation was 2.2 months (range, 0.6-6.5 months). Moreover, a significantly higher dislocation rate was observed in the SER muscles treated with tendon-to-bone repair compared to tendon-to-tendon repair, and a high dislocation rate was seen when acetabular CE angle was less than 44°.
The incidence rate of hip fractures shows a gradual rise with increasing average life span and population aging1516). Surgical treatment is warranted for elderly people with hip fractures to reduce complications with early ambulation and to return to pre-injury ambulation ability1718). Bipolar hemiarthroplasty is generally the preferred choice for treating displaced femoral neck fractures and is gradually increasing in popularity161920). Bipolar hemiarthroplasty is commonly used for older patients with femoral neck fractures or intertrochanteric fractures by enabling early ambulation, and the potential complications of hip implants are loosening, wear of acetabular cartilage, infection, dislocation and others21). Dislocation often accompanies difficulty with closed reduction and higher mortality and morbidity rates, warranting careful close attention22). Several studies reported incidence rates of dislocation, one of the severe complications after bipolar hemiarthroplasty, ranging between 1.5-16%1223). By using a postero-lateral approach as the common treatment option, dislocation rate after bipolar hemiarthroplasty was 5.6% according to Madanat et al.10) and 10.7% according to Mukka et al.9) This research had a comparable or slightly lower dislocation rate at 3.8% compared with other studies.
This study explored patient factors, surgical techniques and problems of implants as risk factors of bipolar hemiarthroplasty. Of these, dislocation commonly occurred in patients with a smaller CE angle. Mukka et al.9) reported that the shortening of femoral offset and leg length can increase dislocation rate by decreasing tension in the peripheral soft tissues, and suggested a small CE angle indicating a shallow acetabulum as a risk factor for dislocation. Madanat et al.10) and Ninh et al.11) suggested a shorter femoral offset and a smaller CE angle as risk factors for dislocation. A decrease in femoral offset and limb length shortening may reduce tension of muscles attached to the greater trochanter, decrease the length of the lever arm, and induce impingement between the femoral head and acetabulum, resulting in dislocation. However, no significant difference was found in femoral offset and leg length between dislocation and control groups in the present study, and a significant difference was detected only in acetabular CE angle. In particular, a higher dislocation rate was observed in patients with acetabulum having a CE angle of 44° or less. Rather than soft-tissue tension, acetabular morphology is associated with greater attribution to dislocation. Thus, when considering bipolar hemiarthroplasty for elderly patients with femoral neck fracture, it is thought to be important to select patients with sufficient coating in the lateral edge of acetabulum through radiologic examination preoperatively by measuring CE angle on the healthy side. For patients with insufficient coating in the lateral edge of acetabulum due to a small CE angle, anterior or lateral approach or THA needs to be considered as a treatment option, instead of postero-lateral approach, in order to minimize dislocation.
Preservation of posterior soft tissues and SER repair are known to be important preventive measures for reducing dislocation rates in postero-lateral approach678). Although several studies have covered tendon-to-tendon repair and tendon-to-bone repair as reconstruction methods for SER, comparative studies between these two methods have been rarely conducted. Weeden et al.24) achieved a satisfactory dislocation rate of 0.85% through reconstruction of SER and remaining soft tissues after THA with posterior approach. Furthermore, Ko et al.7) reported a dislocation rate of 0% through tendon-to-bone repair by the Krackow technique. According to Sherman et al.25), tendon-to-bone repair was a useful method for repairing tendons as ultimate load to failure comparable to tendon repair using suture anchors was observed. In the present study, a lower dislocation rate was obtained using tendon-to-bone repair compared to that of tendon-to-tendon repair. For this reason, better fixation can be achieved by repairing the bone rather than the soft tissue, since trochanteric soft tissues are more susceptible to tears than the bone during tendon-to-tendon repair. Since drilling through the greater trochanter is possible in older patients with osteoporosis, dislocation needs to be prevented by restoring maximum soft-tissue tension including joint capsule tension by performing tendon-to-bone repair, despite the complicated surgical procedures.
Dementia has been suggested as one cause for dislocation in several studies. A higher frequency of dislocation following THA has been found due to patient's lack of understanding, communication problems with physicians, a decreased response to pain and decline in walking ability112627). According to a study by Mukka et al.9), mental status was more likely to be associated with dislocation than age, gender, ASA and other factors. On the other hand, a recent study proposed that there was no association between mental status and dislocation. Madanat et al.10) reported that dislocation had no association with age, gender, BMI, dementia, alcohol consumption, living environment, operation time, operator experience and others. Comparable to these previous studies, no association was found between dislocation incidence and patient-related factors including mental status in this study. Hemiarthroplasty has relatively greater resistance to dislocation than THA, since this procedure tends to be less prone to abnormal location of acetabular cup and has bipolar articulation. Hence, this surgical procedure is anticipated to be relatively safe with a lower risk of dislocation in patients with mental illnesses such as dementia.
There are several limitations to note in the present study. First, study findings may fall short of statistical significance due to the relatively small sample size. However, the advantage of this study is that the total sample size was larger than the average number of subjects in other studies. Second, as a retrospective study, mental status was insufficiently assessed because mental state was examined based on medical records. Since some previous studies have identified the presence of mental symptoms as a critical risk factor for dislocation, further studies are warranted by performing a thorough mental status evaluation. Third, patient's cooperation on dislocation-inducing behaviors that should be avoided such as fall, early ambulation, excessive hip flexion or others was inadequately evaluated in the early postoperative period. Fourth, this study was limited in examining prosthesis-related factors. Although the rotational alignment of the femoral component could be associated with dislocation, this factor was not examined since it was difficult to identify on plain radiographs. In addition, the type of bipolar components could be also related to dislocation, but the authors did not analyze implant size because we used femoral stems close to the actual size.
SERs should be repaired using tendon-to-bone repair method to reduce dislocation rate in elderly patients undergoing bipolar hemiarthroplasty using postero-lateral approach due to femoral neck fracture. In addition, patients with smaller CE angle should be carefully monitored due to high incidence of dislocation.
References
1. Klop C, Welsing PM, Cooper C, et al. Mortality in British hip fracture patients, 2000-2010: a population-based retrospective cohort study. Bone. 2014; 66:171–177. PMID: 24933345.

2. Brozek W, Reichardt B, Kimberger O, et al. Mortality after hip fracture in Austria 2008-2011. Calcif Tissue Int. 2014; 95:257–266. PMID: 24989776.

3. Turner RS. Postoperative total hip prosthetic femoral head dislocations. Incidence, etiologic factors, and management. Clin Orthop Relat Res. 1994; (301):196–204. PMID: 8156674.

4. Moore AT. The self-locking metal hip prosthesis. J Bone Joint Surg Am. 1957; 39-A:811–827. PMID: 13438939.

5. Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg Br. 1982; 64:17–19. PMID: 7068713.

6. Suh KT, Park BG, Choi YJ. A posterior approach to primary total hip arthroplasty with soft tissue repair. Clin Orthop Relat Res. 2004; (418):162–167. PMID: 15043109.

7. Ko CK, Law SW, Chiu KH. Enhanced soft tissue repair using locking loop stitch after posterior approach for hip hemiarthroplasty. J Arthroplasty. 2001; 16:207–211. PMID: 11222895.

8. Pellicci PM, Bostrom M, Poss R. Posterior approach to total hip replacement using enhanced posterior soft tissue repair. Clin Orthop Relat Res. 1998; (355):224–228. PMID: 9917607.

9. Mukka S, Lindqvist J, Peyda S, et al. Dislocation of bipolar hip hemiarthroplasty through a postero-lateral approach for femoral neck fractures: a cohort study. Int Orthop. 2015; 39:1277–1282. PMID: 25557759.

10. Madanat R, Mäkinen TJ, Ovaska MT, Soiva M, Vahlberg T, Haapala J. Dislocation of hip hemiarthroplasty following postero-lateral surgical approach: a nested case-control study. Int Orthop. 2012; 36:935–940. PMID: 21931967.

11. Ninh CC, Sethi A, Hatahet M, Les C, Morandi M, Vaidya R. Hip dislocation after modular unipolar hemiarthroplasty. J Arthroplasty. 2009; 24:768–774. PMID: 18555648.

12. Barnes CL, Berry DJ, Sledge CB. Dislocation after bipolar hemiarthroplasty of the hip. J Arthroplasty. 1995; 10:667–669. PMID: 9273380.

13. Bhuller GS. Use of the giliberty bipolar endoprosthesis in femoral neck fractures. Clin Orthop Relat Res. 1982; (162):165–169. PMID: 7067210.

14. Petersen MB, Jørgensen HL, Hansen K, Duus BR. Factors affecting postoperative mortality of patients with displaced femoral neck fracture. Injury. 2006; 37:705–711. PMID: 16765352.

15. Chang JD, Yoo JH, Lee SS, Kim TY, Jung KH, Kim YK. Bipolar hemiarthroplasty for hip fractures in patients aged over 90 years - the factors influencing the postoperative mortality. J Korean Hip Soc. 2010; 22:283–290.
16. Lim CH, Chung YY, Kim JS, Kim CY. Hemiarthroplasty for hip fractures in elderly patients over 80 years old-comparative analysis between femoral neck fracture and intertrochanteric fracture. Hip Pelvis. 2013; 25:44–50.
17. Alarcón T, González-Montalvo JI, Bárcena A, Saez P. Further experience of nonagenarians with hip fractures. Injury. 2001; 32:555–558. PMID: 11524088.

18. Ooi LH, Wong TH, Toh CL, Wong HP. Hip fractures in nonagenarians--a study on operative and non-operative management. Injury. 2005; 36:142–147. PMID: 15589932.

19. Iorio R, Schwartz B, Macaulay W, Teeney SM, Healy WL, York S. Surgical treatment of displaced femoral neck fractures in the elderly: a survey of the American Association of Hip and Knee Surgeons. J Arthroplasty. 2006; 21:1124–1133. PMID: 17162171.
20. Raaymakers EL. Fractures of the femoral neck: a review and personal statement. Acta Chir Orthop Traumatol Cech. 2006; 73:45–59. PMID: 16613748.
21. Kim SH, Lee SW, Kong GM, JeaGal MU. Comparison between the results of internal fixation using proximal femur nail anti-rotation and bipolar hemiarthroplasty in treatment of unstable intertrochanteric fractures of elderly patients. J Korean Hip Soc. 2012; 24:45–52.

22. Gregory RJ, Gibson MJ, Moran CG. Dislocation after primary arthroplasty for subcapital fracture of the hip. Wide range of movement is a risk factor. J Bone Joint Surg Br. 1991; 73:11–12. PMID: 1991741.

23. Pajarinen J, Savolainen V, Tulikoura I, Lindahl J, Hirvensalo E. Factors predisposing to dislocation of the Thompson hemiarthroplasty: 22 dislocations in 338 patients. Acta Orthop Scand. 2003; 74:45–48. PMID: 12635792.

24. Weeden SH, Paprosky WG, Bowling JW. The early dislocation rate in primary total hip arthroplasty following the posterior approach with posterior soft-tissue repair. J Arthroplasty. 2003; 18:709–713. PMID: 14513442.

25. Sherman SL, Copeland ME, Milles JL, Flood DA, Pfeiffer FM. Biomechanical evaluation of suture anchor versus transosseous Tunnel quadriceps tendon repair techniques. Arthroscopy. Published online February 16, 2016. DOI: 10.1016/j.arthro.2015.11.038.

26. Enocson A, Tidermark J, Tornkvist H, Lapidus LJ. Dislocation of hemiarthroplasty after femoral neck fracture: better outcome after the anterolateral approach in a prospective cohort study on 739 consecutive hips. Acta Orthop. 2008; 79:211–217. PMID: 18484246.

Fig. 1
Measurement of global femoral offset on plain radiograph was defined as the addition of the distance between the longitudinal axis of femur to center of femoral head plus the distance from the center of the femoral head to a perpendicular line passing through the medial edge of the ipsilateral teardrop point of the pelvis.
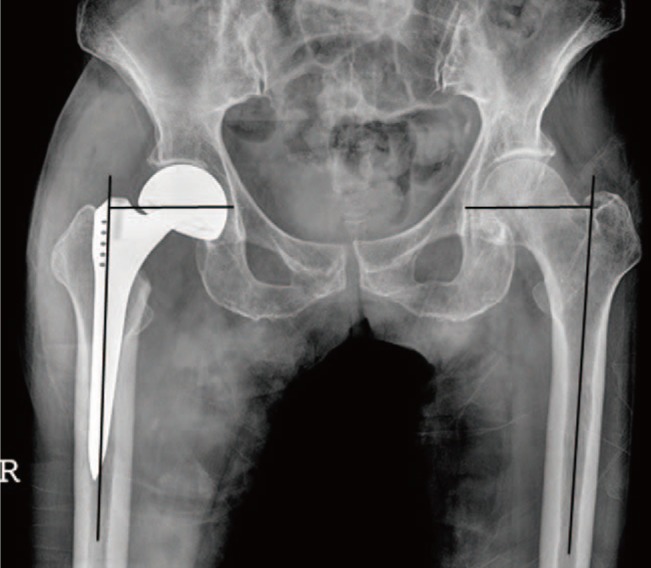
Fig. 2
Measurement of leg length discrepancy on plain radiograph was defined as the difference in perpendicular distance in millimeters between a line passing through the lower edge of the teardrop points to the corresponding tip of the lesser trochanter.
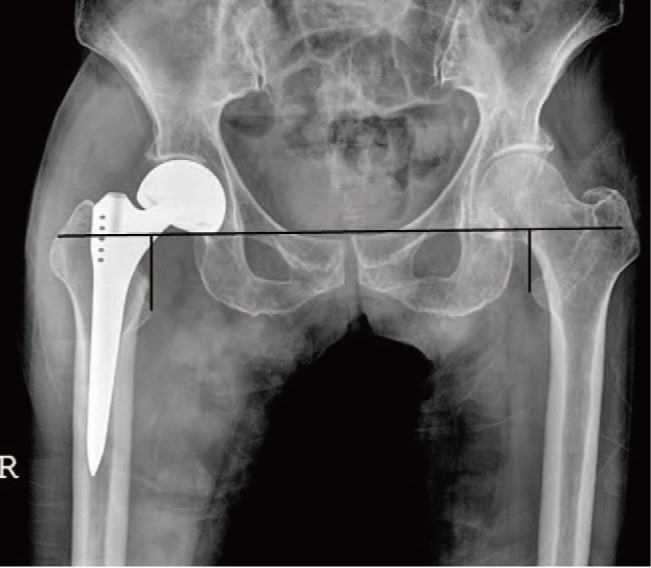
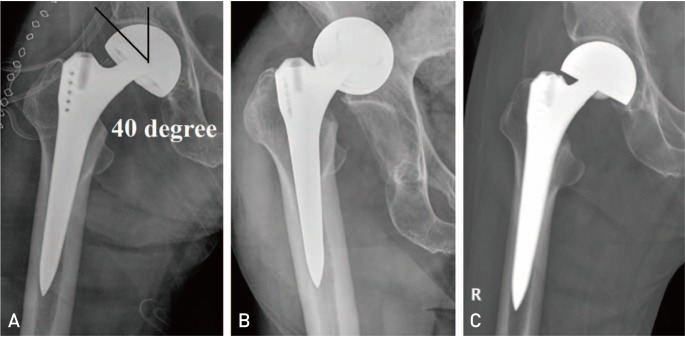
Fig. 3
Measurement of center-edge angle on plain radiograph was defined as the angle between the center of prosthetic head and the lateral edge of acetabulum.

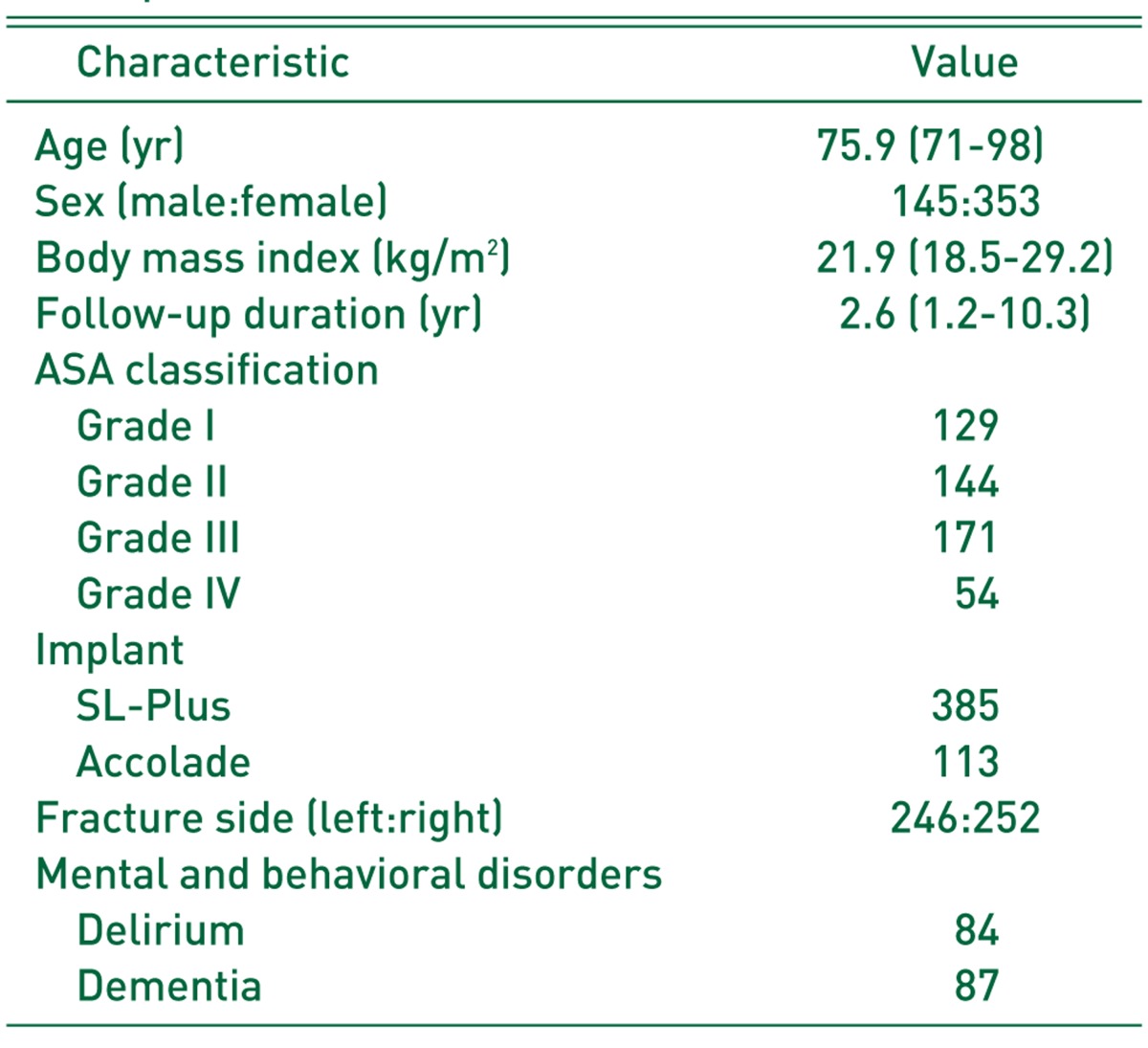
Fig. 4
A 72 years old woman with femur neck fracture. (A) An immediate postoperative anteroposterior radiograph shows 40° of center-edge angle, measured as the angle between the center of prosthetic head and the lateral edge of acetabulum. (B) Radiograph obtained at postoperative 14th day showed dislocation of bipolar hemiarthroplasty. (C) The patient was treated with closed reduction and the radiograph was taken after closed reduction. There was no recurrence of dislocation thereafter.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download