Abstract
Purpose
We aimed to quantify proximal femoral shortening after operation with compression hip screws for intertrochanteric fracture in patients under the age of 60 years.
Materials and Methods
We followed 37 consecutive patients with intertrochanteric fractures treated with compression hip screws from March 2005 to February 2014. We designated the aspect of the fracture, a defect of the postero-medial wall, a defect of the lateral wall, and the degree of reduction as four potentially important factors we assumed would strongly affect proximal femoral shortening. We quantified proximal femoral shortening and compared the effects of above factors. We divided femoral shortening into two plane vectors; femoral offset in the horizontal plane and leg length discrepancy in the vertical plane. We measured shortening separately during two periods: during operation and after weight bearing (called dynamic compression).
Results
After bone union, the average femoral offset shortening was 5.45 mm. Patient groups with anatomic reduction and intact postero-medial wall showed lower femoral offset shortening than the respective opposite groups. As to functional score using modified Harris hip score, low femoral offset shortening group showed more 2.35 scores than high groups. None of the factors significantly affected leg length shortening.
Femoral intertrochanteric fractures in elderly patients often result in serious complications if proper and timely treatment is not provided. In particular, the major objective of surgical treatment in the elderly might be the recovery of ambulatory ability in conjunction with fixation of fractures. It is however important to note that treatment of young patients for intertrochanteric fractures should not be limited to ambulation recovery but should also consider resumption of sport activities.
Intertrochanteric fractures are often treated by surgical approaches that use compression hip screws, intramedullary nails, or hip arthroplasty1). These approaches have their own several benefits. One of them is that compression hip screws provide compression pressure force on the surface of the fractures, thereby enhancing bone union. In the case of unstable fractures, however, excessive compression force may result in femoral shortening, which would be a significant drawback2). Proximal femoral shortening causes shortening of the abductor lever arm and results in leg length discrepancy (LLD). These drawbacks increase physical stress on the hip when walking, which may result in pain and development of osteoarthritis, particularly in non-elderly patients who are required to be socially active3).
The compression force may occur at two different points in procedures that involve the use of compression hip screws. First, it may take place during fracture reduction via compression screw insertion. The other possibility is when physical stress is applied to patient's hip through their body weight, that is weight bearing. So far, most studies have discussed compression without considering the timing34). In addition, most results in previous studies were not adjusted; hence, patient's body weight and size were not considered.
The major objective of the present study was to investigate proximal femoral shortening after surgical treatment of femoral intertrochanteric fractures using compression hip screws in patients who were under the age of 60 years and had no history of diseases requiring regular treatment.
From March 2005 through February 2014, patients who underwent femoral intertrochanteric fracture surgery using compression hip screws were enrolled in the study. Inclusion criteria were as follows: 1) patients who had no history of diseases requiring treatment on a regular basis and 2) patients were younger than 60 years. Exclusion criteria were as follows: 1) fracture non-union was observed, 2) patients had previous damage of both femora when the fracture occurred, 3) no radiological data was available before and after surgical procedures and for the follow-up period, 4) radiological data was not able to be measured, and 5) patients had pathological fractures. The present study was done retrospectively. All procedures were performed by a single surgeon, while data analysis was done by the same surgeon and another doctor (fellowship). Statistical analyses were done by another doctor (fellowship). A total of 185 patients under the age of 60 years underwent surgical treatment, of which 37 patients (23 males and 14 females) were included in this study based on our inclusion and exclusion criteria. The average age of the patients was 47 years (range, 26-60 years). The average follow-up period after surgery was 23 months (Table 1).
In this study, we assumed that the following four major factors may significantly influence femoral shortening: the aspect of the fracture, a defect of the postero-medial wall, a defect of the lateral wall, and the degree of reduction. Using these factors, we categorized the patients into subgroups and then the impact of each factor was estimated by quantifying the degree of proximal femoral shortening it caused. Proximal femoral shortening was expressed as femoral offset and LLD, which represent the changes of horizontal and vertical vectors, respectively. The changes were measured at two different time points when compression was occurring: right after surgery and after bone union; the total value was then subtracted by the femoral shortening value measured right after surgery to calculate the shortening ratio caused by dynamic compression.
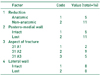
Fractures were classified by using the AO/OTA classification system. A fracture was defined as 31 A1 if a single fracture line was extending to the medial cortex by intertrochanteric fractures and as A2 if more than one such fracture line was present. Nine, 18, and 10 patients were found to have 31 A1, 31 A2, and 31 A3 fractures, respectively (Table 2). Fractures were further classified according to syntripsis of the lateral wall of the proximal femur from the tip of the greater trochanter through the lesser trochanter site. Fourteen patients had syntripsis of the lateral wall. The defect of the postero-medial wall was defined as more than two-thirds of the lesser trochanter being isolated from the medial intertrochanteric region in the post-operative anteroposterior (AP) view of the pelvis. Fifteen patients had this defect.
During surgery, two different tools were used: 1) 135° compression hip screws (CHS System; Solco, Pyeongtaek, Korea) and 2) 129°anti-hypersliding compression hip screws developed in our hospital (Break Top System Compression Hip Screw; Solco). In addition to these basic compression hip screws, greater trochanter-stabilizing plates were used for unstable fractures; fracture stability was estimated in advance to or in the middle of surgery when the general condition of the patient allowed.
If their condition allowed, all patients were advised to sit on their bed upright as well as in a wheelchair right after surgery. Radiographs were taken on the next day after surgery and then the patients were assessed for their ambulation level, pain, and activity level 2 weeks, 3 months, 6 months, and 1 year after surgery, respectively, radiographs were taken at the same time points. The modified Harris hip score (HHS) was used after bone union to assess the recovery of patients' function. Pelvis AP and hip axial view radiographs were taken whilst the tip-apex distance (TAD), degree of reduction, location of lag screws, and proximal femoral shortening were assessed using post-operative radiographs.
The reduction of fractures was determined as non-anatomical reduction if more than one site had a 3-mm or larger step-off of the cortex in post-operative AP or axial view radiographs. Shortening of the proximal femur was measured from changes in femoral offset and leg length. In the AP view of the pelvis obtained using the picture archiving and communication system (PACS), shortening of the femoral offset was measured as a surrogate marker given its similarity with the length of the abductor lever arm5). To measure the femoral offset, a circle close to the femoral head was drawn on the AP radiograph of the pelvis using the PACS in order to make the head center, and then a line dividing the stem part that is 10 cm apart from the lowest part of the lesser trochanter was drawn; the horizontal distance between the line and the head center was measured (Fig. 1). When measured, the diameter of the lag screw shaft was assessed to correct measuring errors potentially due to differences in magnification, and then the measured value was corrected again based on the obtained ratio compared to the actual diameter, 8.4 mm.
To estimate the LLD, the tear drop was established based on patient's pelvis and then the tip of either the greater or lesser trochanter (whichever of them did not show any changes during bone union) was selected as a femoral reference to measure the difference between the normal and damaged sites. To minimize error due to rotation in measurements using AP views of the pelvis, radiographs showing the same size of lesser trochanters were selected; in serial follow-up analyses, only radiographs showing similar sizes of lesser trochanters were chosen for further analyses. Measurements were performed right after surgery and after bone union, i.e. the two time points at which compression was occurring, as mentioned above. In addition, percentage was calculated by dividing the corrected value per body size by femoral offset on the normal side.
Nonparametric analyses, Mann-Whitney test, and Kruskal-Wallis test were used to examine the differences in the four major factors (the aspect of the fracture, a defect of the postero-medial wall, a defect of the lateral wall, and the degree of reduction) using the IBM SPSS Statistics software ver. 19.0 (IBM Co., Armonk, NY, USA). A P-value less than 0.05 was considered statistically significant.
The TAD was within 25 mm in 30 patients and 25-28 mm in 7 patients. All 37 patients were satisfied with the location of lag screws (center-center on the pelvis AP and hip axial view radiographs). The patient group (n=37) had an average LLD shortening of 8.84 mm. Shortening that occurred during surgery was subtracted from this value to obtain shortening that solely resulted from dynamic compression because of weight loading; it was found to be 3.48 mm. Shortening of the femoral offset was 5.45 mm after bone union, whereas corrected shortening (i.e., shortening that was caused solely by weight loading) was 3.56 mm. The average shortening caused by dynamic compression divided by the femoral offset on the normal side was found to be 8.32%. Overall, in a total of 37 patients, 65.32% of femoral offset shortening and 39.36% of LLD were caused by dynamic compression.
We further investigated the effects of the four major factors on proximal femoral shortening. A significant femoral offset reduction was found in the group that had non-anatomical reduction, a defect of the postero-medial wall compared to the group with anatomical reduction and the group with no defect on postero-medial wall (P=0.002; Table 3). Both the decrease in femoral offset by weight loading and the percentage corrected for individual body size were statistically significant. In contrast, neither the aspect of the fracture nor the defect of the lateral wall was significantly associated with femoral shortening (P=0.552 and 0.237, respectively).
Regarding femoral offset reduction and the percentage corrected for body size, high-risk and low-risk groups were defined on the basis of the reference value of 10%. The high-risk group included 16 patients. In the functional test using the modified HHS, the low-risk group had an average value of 85.47 points, which was slightly higher than the group with a high risk of shortening (83.13), yet the difference did not reach statistical significance (P=0.091). Logistic regression analysis showed that none of the risk factors was statistically significant in the group with a high risk of femoral offset shortening; however, the P-values for three risk factors (except for the fracture aspect) were on the borderline of statistical significance (Table 4, 5).
None of the risk factors were significant for LLD. In the group with anatomical reduction, the average value of LLD caused by dynamic compression was 3.07 mm, whereas in the group with non-anatomical reduction it was 4.08 mm. The LLD values of the group with a defect of the postero-medial wall and the one without a defect were 3.72 mm and 3.34 mm, respectively.
The compression hip screw is a tool that uses the concept of a tension band plate6). Consequently, the defects on the medial wall may lead to significant clinical outcomes after surgery. In this study, we found that 15 patients had defects on the postero-medial wall. We also found a significant femoral offset reduction in the groups with non-anatomical reduction and a posteromedial wall defect. These results indicate that the fixation force of a compression hip screw weakens in the absence of proper support when weight bearing is resumed.
Neither the aspect of the fracture nor syntripsis of the lateral wall was shown to be significant for proximal femoral shortening. Regarding the aspect of the fracture, a trochanteric stabilizing plate (TSP) was employed in patients with AO/OTA 31 A2 and 31 A3 fractures, which may confer additional stability and explain the absence of significant association between the aspect of the fracture and proximal femoral shortening. Similarly, we believe that no association was observed between the defect of the lateral wall (syntripsis) and proximal femoral shortening because of the additional stability provided by the TSP7).
It has been demonstrated that proximal femoral shortening is affected by multiple factors after surgical treatment for femoral intertrochanteric fractures. In particular, the degree of TAD and the fracture aspect have been suggested to be significant risk factors8). In the present study, 7 patients had TAD exceeding 25 mm; among them, 6 were further categorized into the high-risk group (>10% of femoral offset shortening).
When bone density was categorized by using the Singh index, all patients except 5 had the index values higher than 4. This might be because our study included patients under the age of 60, which limited the comparison between groups with different bone density. Another limitation of our study was that the femoral offset was measured using two-dimensional (2D) AP views of the pelvis. In other studies, changes in the abductor lever arm were analyzed using either CAD or PACS9), both of which can accurately measure when no change of greater trochanteric shape is shown. However, changes in the shape of the greater trochanter during bone union are very often found in patients with syntripsis. In this, the use of CAD may result in errors, beause their shape (i.e., that of the greater trochanter) is not identical to the one on the normal side. Similarly, when X-rays are used, the image of the outer slope of the greater trochanter is modified; thus, considerable measuring error might be expected in drawing vertical lines. To overcome such limitations, we measured femoral offset shortening on pelvis AP view radiographs using the PACS instead of measuring the length of the abductor lever arm. In addition, it was suggested that 3D measurements could be more accurate than 2D measurements10). In 2D measurements, femoral rotation, intramedullary changes, and femoral shape may cause errors. Importantly, we noted that considerable numbers of post-operative radiographs showed femoral rotation. These results indicate that, for reduction, the fixation was done in which internal rotation was excessive. In the present study, these patients were excluded as significant error was expected in measurements. Lastly, we aimed to achieve consistent femoral rotation by comparing the sizes of the lesser trochanter and greater trochanter in serial pelvis AP radiographs of the same patient.
In surgical procedures for femoral intertrochanteric fractures, one should consider post-operative activities, especially for non-elderly patients. Although compression hip screws may enhance bone union through compression force, excessive force often results in proximal femoral shortening, thereby hindering patients' normal physical activities and functions. Theoretically speaking, stable fixation using compression hip screws is contingent to the stability of the femoral postero-medial wall. As expected, in the present study, we were able to confirm a significant association between the stability of the proximal femoral postero-medial wall and the reduction in femoral offset. Hence, we recommend that surgeons 1) secure the reconstruction of damaged postero-medial wall and 2) perform anatomical reduction in intertrochanteric surgeries using compression hip screws.
Figures and Tables
 | Fig. 1Radiographic images. (A) Measurement of femoral offset on immediate postoperative pelvic anteroposterior view. (B) Red line indicates femoral offset on the last follow-up. |
References
1. Kiran Kumar GN, Sanjay M, Vijaya Kumar N, Manjunath S, Vinaya Raj MK. Bipolar hemiarthroplasty in unstable intertrochanteric fractures in elderly: a prospective study. J Clin Diagn Res. 2013; 7:1669–1671.
2. Yoo JH, Kim TY, Chang JD, Kwak YH, Kwon YS. Factors influencing functional outcomes in united intertrochanteric hip fractures: a negative effect of lag screw sliding. Orthopedics. 2014; 37:e1101–e1107.

3. Platzer P, Thalhammer G, Wozasek GE, Vécsei V. Femoral shortening after surgical treatment of trochanteric fractures in nongeriatric patients. J Trauma. 2008; 64:982–989.

4. Cho MR, Lee SH, Cho DW, Ko SB. Treatment of unstable intertrochanteric fractures of the femur using an antihypersliding compression hip screw and TSP. J Korean Hip Soc. 2012; 24:37–44.

5. Lecerf G, Fessy MH, Philippot R, et al. Femoral offset: anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop Traumatol Surg Res. 2009; 95:210–219.

6. Güven M, Yavuz U, Kadioğlu B, et al. Importance of screw position in intertrochanteric femoral fractures treated by dynamic hip screw. Orthop Traumatol Surg Res. 2010; 96:21–27.

7. Gupta RK, Sangwan K, Kamboj P, Punia SS, Walecha P. Unstable trochanteric fractures: the role of lateral wall reconstruction. Int Orthop. 2010; 34:125–129.

8. Abdulkareem IH. A review of tip apex distance in dynamic hip screw fixation of osteoporotic hip fractures. Niger Med J. 2012; 53:184–191.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download